Abstract
Objectives
Osteoporosis is a prevalent problem amongst the elderly. Bone mineral density (BMD) obtained from dual X-ray absorptiometry (DXA) is the gold standard in diagnosing osteopenia (-1.0 < t < -2.5) and osteoporosis (t > -2.5). However, following osteoporosis therapy, increases in BMD may be unreliable. Although hip fracture risk can be reduced with the aid of drugs, treated patients still face considerable risk as most people who sustain hip fracture do not have generalized osteoporosis. A study of the local distribution of bone mass was necessary as they contribute to the geometry and consequently the bone strength.
Methods
By identifying the respective regions in the femoral neck, the geometric changes were localized and differed between each patient, proving that drug treatment elicits local changes in mean outer radius and mean cortical thickness. Numerical analysis also validated the above findings, where critical strain regions were predicted at similar zones and this is coherent with the fact that reduced thickness of the cortical bone has been related to increased risk of fracture initiation.
Results
Hence, from individual radar plots, we can determine if the effect of drugs had outweighed the effect of aging. We can then propose a course of treatment drug better suited for the patient in the clinical scenario.
Conclusion
Clinically, little conclusion can be drawn from just the BMD in osteopenic / osteoporotic patients. This emphasizes the necessity of using geometry and structure to predict fracture risk. Focusing on a patient specific analysis at a local level will improve diagnosis of osteoporosis and ultimately fracture prediction.
Osteoporosis causes high social and economic costs to the society and thus is a critical problem of concern amongst the elderly especially.1 Incidences of osteoporotic fractures are known to happen more frequently in the elderly than in the young. However, osteoporosis is diagnosed based on the bone mineral density (BMD) retrieved from dual energy X-ray absorptiometry (DXA) scans. This is a problem as the diagnosis is often inaccurate in identifying people with and without osteoporosis. Many who obtain a fracture have not been diagnosed with osteoporosis previously. A study has shown that only 48% of patients who were diagnosed as osteoporotic, experienced hip fractures.2 Furthermore, amongst patients who were treated with risedronate, a drug of interest in this study, only 40% of the osteoporotic patients and 30% of the elderly patients had decreased fracture risk.3 This goes to show that BMD only partially reflects hip fracture risk.4,5
While BMD itself has several inherent limitations, the main criticisms can be summarized as follows; it is obtained from a single areal projection in one plane and consequently cannot be characteristic of overall three-dimensional bone mass distribution.6 Secondly, the non-uniform geometry of the bone renders averaged or mean parameters less useful as they could mask the net gain or loss of bone mass. Lastly, we also overestimate the capability of BMD to be a substitute for geometry and strength which can be an ambitious task from a single predictor.
During the course of our study, we observed that changes in BMD across a follow-up study likes ours was meaningless as an increase in BMD due to drug treatment did not represent an improved structure. Instead, we found local regions of osteoporosis, or in other words, extreme loss of bone mass in localized regions. Therefore, we analyzed local buckling ratio (BR) values in the femoral neck (FN) over three years in risedronate treated patients, which is a common bisphosphonate, used to treat osteoporosis. And these BR values were then used to characterize finite element predicted fracture loads and thus discover regions of local osteoporosis. And this pathogenic existence of local osteoporosis could mean a higher risk of FN fracture despite drug treatment.4
As this study aims to understand the local geometric instabilities in the FN, two subjects were analyzed in details. These two subjects were administered risedronate drug treatment, over three years from 2008 to 2010. To compare the geometries of their FNs, BR was calculated. This was attained by measuring the outer radius and the cortical thickness at twelve different intervals along the cross section of the FNs.7 Commercial software, Mimics® (Materialise, Leuven, Belgium), was used to extract these geometric values. BR is given as the ratio of the mean outer radius to the mean cortical thickness.8 Therefore, prior to averaging the outer radius and cortical thickness values obtained at the twelve intervals, BR is calculated. Consequently, a BR value for each year (2008, 2009 and 2010) for each of the two subjects was obtained. Through use of finite element analysis, we obtained the critical fracture load (Fcr) which was used as the ultimate point in which failure occurs in the femur and in particular, the FN. Also, a Fcr was derived from finite element analysis, using commercial software, ABAQUS® (Dassault Systèmes Simulia Corp., Providence, RI, USA).9
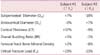
Subject #1 was a 73 year old Korean female with a body mass index (BMI) of 26.1 and FN BMD of 0.628 in the baseline year, whereas subject #2 was a 75 year old Korean female with a BMI of 26 and FN BMD of 0.594 (Table 1). Both subjects were in the same age group with little difference in their BMI and a 3.4% difference in their FN BMD,10 which is insignificant. Thus, the comparison of their geometrical and structural parameters is a fair one.
As shown by Table 2, mean geometrical properties, FN BMD and Fcr of the two subjects are tabulated. It can be seen that Subject #1 exhibited an increase in Fcr (+23%), with an increase in periosteal diameter and no change in endocortical diameter, consequently reflecting an increase in mean cortical thickness (+37%). While FN BMD did not show a significant change from 2008 to 2010 (+2%), the overall BR seems to show an unexpected increase (+5%). In contrast, subject #2 exhibited a decrease in Fcr (-23%), with a decline in the subperiosteal diameter (-18%) and an increase in the endocortical diameter (+7%). Due to this unmatched changes, the mean cortical thickness declined (-9%) which seems to be matched by a similar decline in FN BMD (-8%). Also, overall BR only changed by -1%, which was insignificant.
The study then proceeded to observe the local changes in periosteal diameter, endocortical diameter, cortical thickness and BRs. While the radar plot of BRs of subject #1 shows a uniform annular structure with no abrupt changes in cortical thicknesses, the computed tomography-scan image shows limited information due to lack of resolution (Fig. 1). However, subject #2 exhibited critical regions at the supero-anterior region (30°) and a largely thick cortice at the infero-anterior region (300°-330°) (Fig. 1). In addition, plots of local BR values against the respective regions again emphasizes the fact that subject #1 had local BR values well below the critical value of 10 in 2008 and 2010 while subject #2 had a critical region in the infero-posterior region (210°-240°) in 2008 and that critical region passed on and a new one formed in the supero-anterior region (0°-60°) in 2010 (Fig. 2).
In this study, the structural parameter predicted from finite element analysis was analyzed together with the derived geometric parameter, to observe any patterns or correlations, which may provide more insight in the etiology of FN fractures. The penultimate aim is to work towards a more rigorous diagnosis. By observing more predictors with localized changes, with the inclusion of geometry and strength in the diagnosis through use of imaging and finite element analysis, this aim could be achieved.
With respects to both subject #1 and subject #2, it was found that the changes in the overall BR were insignificant. This was because an increase in BR is supposed to reflect cortical instability and vice versa. This would mean that the overall BR for subject #1 should decrease while for subject #2 it should increase, based on their respective fracture load changes. This shows that other than the mean cortical thickness,11 which seems to correlate with changes in Fcr, the changes in the other mean geometrical parameters as well as FN BMD did not provide any useful information. This warranted a look at the local BRs.
Despite the fact that both subjects were under antiresorptive drug treatment, only subject #1 has shown a positive response as there were no critical regions of extremely thin cortices. On the other hand, subject #2 has shown a negative response. This is because although, the critical region at the infero-posterior region disappeared, another critical region formed at the supero-anterior region. This suggests that the drug treatment could be more effective in selective regions, for example, at regions with higher loadings, in response to greater mechanical demands.10
Hence, the findings prove the importance of patient-specific analysis. Patients may already be facing a pathogenic existence of local osteoporosis that may compromise on their anti-resorptive drug treatments.4 By assessing their radiological scans, and with the help of radar plots as shown in this study, detailed observations can be made on their FN regions and appropriate exercise strategies that provide increased loadings at the critical zones can be implemented that would benefit the patients more than just the administration of drug treatment.
Figures and Tables
Fig. 1
Computed tomography (top) and radar plot (bottom) cross-sections of femoral necks of Subject #1 (left) and Subject #2 (right).

Fig. 2
Plots of local buckling ratio of Subject #1 and Subject #2 in 2008 and 2010 (BR: buckling ratio).

Acknowledgement
This work was supported by the Academic Research Funding (AcRF #R397-000-094-112) from the Ministry of Education (MoE), Singapore.
References
1. Melton LJ 3rd. Hip fractures: a worldwide problem today and tomorrow. Bone. 1993; 14:Suppl 1. S1–S8.
2. Schott AM, Cormier C, Hans D, Favier F, Hausherr E, Dargent-Molina P, et al. How hip and whole-body bone mineral density predict hip fracture in elderly women: the EPIDOS Prospective Study. Osteoporos Int. 1998; 8:247–254.
3. McClung MR, Geusens P, Miller PD, Zippel H, Bensen WG, Roux C, et al. Hip Intervention Program Study Group. Effect of risedronate on the risk of hip fracture in elderly women. N Engl J Med. 2001; 344:333–340.
4. Anitha D, Kim KJ, Lim SK, Lee T. Implications of local osteoporosis on the efficacy of anti-resorptive drug treatment: a 3-year follow-up finite element study in risedronate-treated women. Osteoporos Int. 2013; 24:3043–3051.
5. Kim TH, Lee HH, Chung SH, Lee WS, Park J, Lee S. Routine application of the Korean FRAX model in women: a single-center study. Korean J Bone Metab. 2012; 19:29–34.
6. Kanis JA, Melton LJ 3rd, Christiansen C, Johnston CC, Khaltaev N. The diagnosis of osteoporosis. J Bone Miner Res. 1994; 9:1137–1141.
7. Carpenter RD, Sigurdsson S, Zhao S, Lu Y, Eiriksdottir G, Sigurdsson G, et al. Effects of age and sex on the strength and cortical thickness of the femoral neck. Bone. 2011; 48:741–747.
8. Young WC. Elastic stability formulas for stress and strain. In : Crawford H, Thomas S, editors. Roark's formulas for stress and strain. 6th ed. New York, NY: McGraw-Hill;1989. p. 688.
9. Keyak JH. Improved prediction of proximal femoral fracture load using nonlinear finite element models. Med Eng Phys. 2001; 23:165–173.
10. Ruff C, Holt B, Trinkaus E. Who's afraid of the big bad Wolff?: "Wolff's law" and bone functional adaptation. Am J Phys Anthropol. 2006; 129:484–498.
11. Pisharody S, Phillips R, Langton CM. Sensitivity of proximal femoral stiffness and areal bone mineral density to changes in bone geometry and density. Proc Inst Mech Eng H. 2008; 222:367–375.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download