Abstract
Moyamoya disease is a rare neurovascular disorder that involves constriction of certain arteries in the brain. In patients with moyamoya disease, it is very important to prevent cerebral ischemic attacks and intracerebral bleeding caused by fluctuating blood pressure and increased respiration. A 40-year-old woman with moyamoya disease was scheduled for extraction of her right upper and lower impacted wisdom teeth. Her lower impacted wisdom tooth was situated close to the inferior alveolar nerve. We decided to continue her oral antiplatelet therapy and planned intravenous sedation with analgesic agents administered approximately five minutes prior to extraction of the root of the mandibular wisdom tooth. Oral analgesic medications were regularly administered postoperatively to alleviate pain and anxiety. During the perioperative period, no cerebrovascular event occurred, and the wisdom teeth were successfully extracted as per the planned procedure. It is thought that the perioperative risks of wisdom tooth extraction in patients with moyamoya disease can be minimized with the use of our protocols.
Moyamoya disease is a rare neurovascular disorder that involves constriction of intracranial internal carotid artery and its branches. Collaterals form around the occlusion of the vessels to compensate for the blockage, but the collateral vessels (moyamoya vessels) are small, weak, and prone to bleeding, aneurysm, and thrombus formation1. On internal carotid artery angiogram, these collateral vessels appear as a 'smoke-like echo' ('moyamoya' in Japanese). This disease is reported more prevalent in East Asia than in Western countries2.
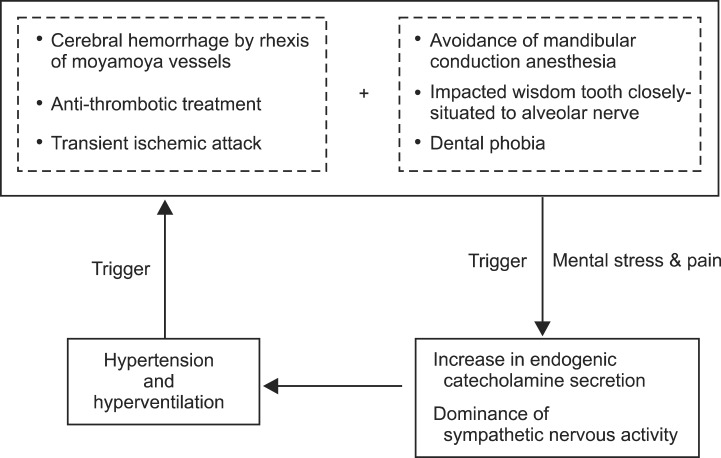
Antiplatelet agents are usually prescribed to prevent the formation of a blood thrombus, and it is recommended that invasive oral surgery be performed under continuous administration of antithrombotic drugs. In patients with moyamoya disease, it is extremely important to prevent cerebral ischemic attacks and intracerebral bleeding caused by fluctuating blood pressure and increased respiration.(Fig. 1)
We report the case of wisdom teeth extraction in a patient with moyamoya disease.
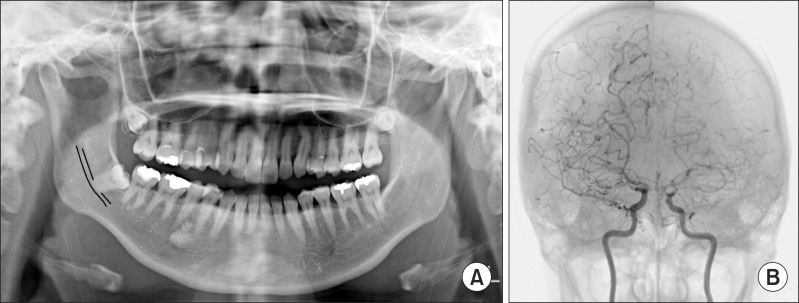
A 40-year-old woman with moyamoya disease was scheduled to extract the right upper and lower impacted wisdom teeth. Her lower impacted wisdom tooth was positioned close to the inferior alveolar nerve.(Fig. 2. A)
She underwent right encephaloduro-arterio-synangiosis (EDAS) procedure. An internal carotid artery (ICA) angiogram showed coarctation at the anterior cerebral artery and middle cerebral artery (MCA) through the bilateral terminal intracranial ICA. Moyamoya vessels were seen from the coarctation area to the posterior basal nucleus. Cerebral blood flow scintigraphy revealed reduced blood flow to the left frontal lobe.(Fig. 2. A) She was taking an antiplatelet agent and was nervous about undergoing dental treatment.
We decided to continue her oral antiplatelet therapy and planned to induce only infiltration anesthesia. Given the invasive nature of the procedure, we planned to put additional administration of the intravenous non-steroidal anti-inflammatory drug (NSAID) about five minutes prior to extraction of the root of the mandibular wisdom tooth on intravenous sedation with midazolam and propofol.
The patient was instructed not to eat or drink four hours before surgery. Once she was in the operating room and the monitors (non invasive blood pressure, electrocardiogram, and arterial oxygen saturation) were set up, we started oxygenation with a nasal canula at a flow rate of 3 L/min. After securing an intravenous line, the sedation was started with 3 mg maintained with 2 mg/kg/h propofol. Once an observer's assessment of alertness/sedation scale (OAA/S) level of 10/20 was reached, topical anesthesia was done by ethyl aminobenzoate (Gingicaine, Osaka, Japan) to the gingiva to relieve pain upon needle insertion. Infiltration anesthesia was then induced using lidocaine 1% with 1 : 100,000 epinephrine (Xylocaine; AstraZeneca, Osaka, Japan). The flurbiprofen (Ropion; Kaken Pharmacentical, Tokyo, Japan) 50 mg was subsequently administered intravenously where the right mandibular wisdom tooth crown and root began to divide. We completely extracted the right lower impacted wisdom tooth. Then we extracted a maxilla impacted wisdom tooth in a similar way. We filled all extraction sockets with collagen sponge (Teruplug; Terumo, Tokyo, Japan) and stitched up a cut wound with an absorbable multifilament suture (Opepolyx 2; Alfresa Pharma Co., Osaka, Japan). The operation lasted for one hour, and the duration of sedation was one hour and 45 minutes. The patient's circulatory dynamics and oxygen saturation remained stable. Oral analgesic drugs were adminis tered postoperatively at regular intervals to alleviate the patient's pain. During the perioperative period, no cerebrovascular event occurred, and the wisdom teeth were successfully extracted.
In moyamoya disease, normocapnia, normotension, and pain control must be strictly controlled to prevent postoperative ischemic complications3. An encephalic blood vessel shrinks as the carbon dioxide level in the blood decreases. Hyperpnea causes such decrease and these lead to decreased cerebral blood flow in constricted blood vessels. Patients with moyamoya disease are more prone to developing ischemia because of decreased cerebral blood flow. Prevention of intracerebral bleeding caused by fluctuations in blood pressure is also important. A major stroke or bleeding could result in permanent loss of function.
The EDAS procedure is a synangiosis procedure that requires dissection of a scalp artery over several inches and then the creation of a small temporary opening in the skull directly beneath the artery. The artery is then sutured to a branch of the MCA on the surface of the brain, and the bone is replaced. Moyamoya disease is a bilateral disorder of certain arteries in the brain. Although the patient had undergone a left EDAS, the right side had not been operated on. Furthermore, this surgical procedure is mainly indicated in pediatric cases and is said to generally have little effect in adult cases4. It is important to maintain the patient's respiration and hemodynamics in the resting state when extracting wisdom teeth. Stress caused by anxiety or predictions regarding blood pressure and respiratory rate results in a rise in catecholamine secretion and sympathetic nervous system dominance5,6. Minimizing anxiety and pain is important during dental treatment in moyamoya patient.
We managed our patient with a combination of local anesthesia and intravenous sedation to minimize her anxiety. Sedation was started with midazolam, which is a short-acting agent without vascular pain. Subsequently, propofol, the dose of which is easy to adjust to ensure appropriate sedation, was administered continuously. One of the disadvantages of propofol is the vascular pain at the time of administration. The patient was rapidly sedated following the administration of midazolam, and she did not complain of vascular pain.
One of the objective evaluations for sedative depth is bispectral index (BIS) value. This device is highly complex and difficult to interpret. OAA/S is the current method used to measure the level of patient sedation. It is often based on the subjective observation of the anesthetist, and clinical scoring methods are commonly used. OAA/S evaluates four items ('responsiveness to name', 'speech', 'facial expression', and 'eyes') with five points possible for each item and 20 points possible at full arousal. Liu et al.7,8 demonstrated that the BIS value correlates with the depth of both midazolam- and propofol-induced sedation as validated by use of the OAA/S rating scale. The depth of sedation was adjusted in accordance with OAA/S to a score of 10-12/20 by the same anesthetist. It can be considered that the dose of sedatives that needed to maintain sedative depth would be correlated to BIS value. This case was able to stabilize circulatory dynamics with sedative depth of OAA/S score of 10-12/20.
Concerning local anesthesia, mandibular foramen conduction anesthesia is effective for pain relief when extracting teeth close to the inferior alveolar nerve. However, we decided that mandibular foramen conduction anesthesia should be avoided in the present case. The risk of hematoma formation is considered for the antiplatelet agents-treated patient. It was thought that we must provide enough analgesic efficacy while avoiding mandibular foramen conduction anesthesia. In this case, it appears that NSAID administration and adequate level of sedation in addition to appropriate infiltration anesthesia made it possible to avoid both hemodynamic changes and strong pain during the extraction of the roots of the teeth.
In conclusion, the perioperative risks of wisdom tooth extraction in patients with Moyamoya disease can be minimized with the use of appropriate intravenous sedation and medication in addition to appropriate infiltration anesthesia.
References
1. Scott RM, Smith ER. Moyamoya disease and moyamoya syndrome. N Engl J Med. 2009; 360:1226–1237. PMID: 19297575.
2. Wakai K, Tamakoshi A, Ikezaki K, Fukui M, Kawamura T, Aoki R, et al. Epidemiological features of moyamoya disease in Japan: findings from a nationwide survey. Clin Neurol Neurosurg. 1997; 99(Suppl 2):S1–S5. PMID: 9409395.

3. Iwama T, Hashimoto N, Yonekawa Y. The relevance of hemodynamic factors to perioperative ischemic complications in childhood moyamoya disease. Neurosurgery. 1996; 38:1120–1125. PMID: 8727141.

4. Kawaguchi T, Fujita S, Hosoda K, Shose Y, Hamano S, Iwakura M, et al. Multiple burr-hole operation for adult moyamoya disease. J Neurosurg. 1996; 84:468–476. PMID: 8609560.

5. Masaoka Y, Onaka Y, Shimizu Y, Sakurai S, Homma I. State anxiety dependent on perspiration during mental stress and deep inspiration. J Physiol Sci. 2007; 57:121–126. PMID: 17389060.

6. Homma S. The effects of stress in response to mirror drawing test trials on the electrogastrogram, heart rate and respiratory rate of human subjects. J Smooth Muscle Res. 2005; 41:221–233. PMID: 16258235.

7. Liu J, Singh H, White PF. Electroencephalogram bispectral analysis predicts the depth of midazolam-induced sedation. Anesthesiology. 1996; 84:64–69. PMID: 8572355.

8. Liu J, Singh H, White PF. Electroencephalographic bispectral index correlates with intraoperative recall and depth of propofol-induced sedation. Anesth Analg. 1997; 84:185–189. PMID: 8989022.

Fig. 2
Imaging findings. A. Panoramic radiography. The right impacted wisdom tooth is situated near the inferior alveolar nerve. B. Internal carotid artery (ICA) angiogram. Anterior cerebral artery (ACA) and middle cerebral artery (MCA) are not clearly visualized. Coarctation at the ACA and MCA through the bilateral terminal intracranial ICA. Moyamoya vessels are seen from the coarctation area to the posterior basal nucleus.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download