Dear Editor,
Catabacter hongkongensis, a newly described anaerobic Gram-positive coccobacillus pathogen, was first isolated in 2007; its draft genome sequence was revealed in 2015 [12]. C. hongkongensis infections are rare, mostly occurring in Hong Kong, but clinically relevant, presenting as sepsis resulting from gastrointestinal disease [12].
A 77-yr-old man was admitted to the hospital for febrile sensation and abdominal pain. Eight years previously, he underwent endoscopic retrograde cholangiopancreatography (ERCP) and endoscopic sphincterotomy for acute cholangitis with a common bile duct stone. He also had a history of hypertension, diabetes mellitus, dilated cardiomyopathy, and atrial fibrillation. Physical examination revealed tenderness over the right upper quadrant of the abdomen, and a diagnosis of acute cholecystitis was made. Laboratory parameters were as follows: leukocyte count, 11.3×109/L (neutrophils, 90.9%); Hb, 16.3 g/dL; platelet count, 113×109/L; AST, 96 U/L; ALT, 52 U/L; alkaline phosphatase, 84 U/L; γ-glutamyl transpeptidase, 163 U/L; total bilirubin, 3.35 mg/dL; direct bilirubin, 1.68 mg/dL; and C-reactive protein, 8.6 mg/dL. Coagulation profiling revealed prolonged prothrombin time (PT, 23.0 sec) and activated partial thromboplastin time (aPTT, 54.1 sec) due to warfarin treatment. Abdominal CT showed gallbladder stones, edematous thickening of the gallbladder wall, mild dilatation and pneumobilia in the left intrahepatic bile duct. The day after admission, ERCP and endoscopic retrograde biliary drainage was performed. Hemobilia originating from the gallbladder was detected, but an emergency operation could not be performed because of prolonged PT and aPTT.
Two blood cultures were obtained, and treatment with empirical intravenous cefodizime and metronidazole was initiated. On day 3 post-incubation, Gram-positive coccobacilli were isolated from the two anaerobic blood cultures. These organisms grew on sheep blood agar as non-hemolytic, white, pinpoint colonies after 48-72 hr of anaerobic incubation at 37℃ (Fig. 1). The bacteria produced catalase. The isolate was not identified by phenotypic identification methods using the Vitek2 ANC card (bioMérieux, Marcy l'Etoile, France) or the API 20A system (bioMérieux). Two matrix-assisted laser desorption/ionization time-of-flight (MALDI-TOF) mass spectrometry instruments, a MALDI Biotyper (Bruker Daltonics Inc., Billerica, MA, USA) and a VITEK MS (bioMérieux), also could not identify the isolate. We therefore sequenced the 16S rRNA gene for identification at the species level [3]. The 16S rRNA sequences (1,358 bp) showed 100.0% similarity with the sequence of C. hongkongensis strains (GenBank accession no: LT223646.1, AB671763.1, NR_115269.1). There were some differences in the biochemical test results of the isolate from that of genetically similar organisms: Ruminococcus species (GenBank accession no: AJ318864.1) that showed Gram-positive diplococci and catalase negativity and Christensenella species (GenBank accession no: LT223568.1) that showed Gram-negative bacilli. Thus, the pathogen was identified as C. hongkongensis.
Antimicrobial susceptibility testing was performed by E-test strips (bioMérieux) or disk diffusion method on Mueller–Hinton agar. Categorical interpretation according to CLSI breakpoints was used. The isolate was susceptible to vancomycin (minimum inhibitory concentration [MIC] 0.5-0.75 µg/mL) and metronidazole, but resistant to penicillin, cefotaxime (MIC>32 µg/mL), colistin, and gentamicin (MIC>256 µg/mL). After seven days of antibiotic treatment, the patient was discharged, and his operation was scheduled at the time of next admission. The patient underwent elective laparoscopic cholecystectomy and recovered without any complications.
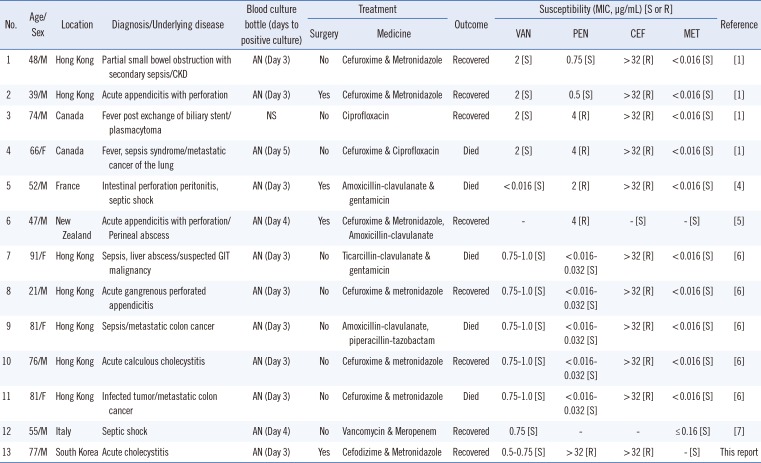
C. hongkongensis has been recently described as a pathogen capable of causing bacteremia [1]. Only twelve cases of bloodstream infection with this organism have been reported to date (Table 1) [14567]. This patient recovered rapidly with antimicrobial therapy and surgery, but five of the 12 reported cases of C. honkongensis bacteremia were fatal. Considering that C. hongkongensis bacteremia is often associated with complications and high mortality, especially in patients with advanced malignancies [6], the importance of accurately identifying this microorganism should be highlighted in clinical microbiology laboratories. Our isolate was susceptible to vancomycin, similar to the isolates reported by Lau et al [6] in 2012. Six out of the seven (86%) patients who were treated with a combination of metronidazole and cefuroxime or cefodizime recovered, whereas four out of the 6 patients who had poor prognosis, i.e., death, were treated by other modalities. These results support the claim that metronidazole-based combination therapy with cefuroxime or cefodizime could be effective for treating C. hongkongensis bacteremia. Because phenotypic identification of C. hongkongensis is difficult and unreliable, the prevalence of infections caused by this organism is likely to be underestimated. Therefore, systemic gram-positive bacilli should not be ignored, and 16S rRNA gene sequencing is a unique technique for accurate species-level identification of C. hongkongensis.
Acknowledgments
This work was supported by a research grant from the Research Institute of Medical Sciences, Chonnam National University (2010-CURIMS-DR007). We are grateful to Bong-Ju Kang, M.T. at the Laboratory of Clinical Microbiology of Chonnam National University Hospital for technical assistance.
References
1. Lau SK, McNabb A, Woo GK, Hoang L, Fung AM, Chung LM, et al. Catabacter hongkongensis gen. nov., sp. nov., isolated from blood cultures of patients from Hong Kong and Canada. J Clin Microbiol. 2007; 45:395–401. PMID: 17122022.
2. Lau SK, Teng JL, Huang Y, Curreem SO, Tsui SK, Woo PC. Draft genome sequence of Catabacter hongkongensis type strain HKU16T, isolated from a patient with bacteremia and intestinal obstruction. Genome Announc. 2015; 3:pii: e00531-15.
3. LiPuma JJ, Dulaney BJ, McMenamin JD, Whitby PW, Stull TL, Coenye T, et al. Development of rRNA-based PCR assays for identification of Burkholderia cepacia complex isolates recovered from cystic fibrosis patients. J Clin Microbiol. 1999; 37:3167–3170. PMID: 10488171.
4. Elsendoorn A, Robert R, Culos A, Roblot F, Burucoa C. Catabacter hongkongensis bacteremia with fatal septic shock. Emerg Infect Dis. 2011; 17:1330–1331. PMID: 21762611.
5. Smith K, Pandey SK, Ussher JE. Bacteraemia caused by Catabacter hongkongensis. Anaerobe. 2012; 18:366–368. PMID: 22710415.
6. Lau SK, Fan RY, Lo HW, Ng RH, Wong SS, Li IW, et al. High mortality associated with Catabacter hongkongensis bacteremia. J Clin Microbiol. 2012; 50:2239–2243. PMID: 22518872.
7. Torri A, Delbianco F, Baccarini FD, Fusari M, Bertini S, Congestrì F, et al. First report of sepsis due to Catabacter hongkongensis in an Italian patient. New Microbes New Infect. 2015; 9:54–55. PMID: 26862436.
Fig. 1
Macroscopic and microscopic appearance of the isolate. (A) They grew on sheep blood agar as non-hemolytic, white, pinpoint colonies after 48-72 hr of anaerobic incubation at 37℃. (B) Microscopic examination of the isolate showed gram-positive coccobacilli (Gram stain, ×1,000).
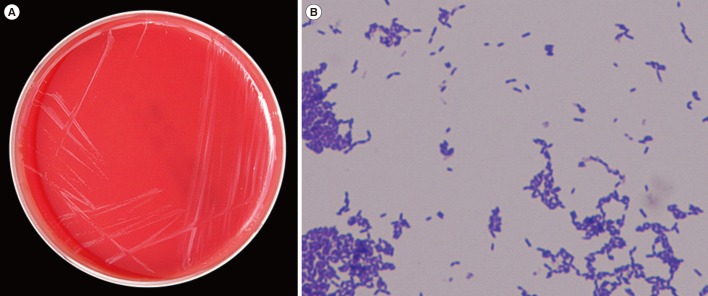
Table 1
Summary of clinical findings and microbial characteristics of Catabacter hongkongensis causing bloodstream infections from the literature
| No. | Age/Sex | Location | Diagnosis/Underlying disease | Blood culture bottle (days to positive culture) | Treatment | Outcome | Susceptibility (MIC, µg/mL) [S or R] | Reference | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Surgery | Medicine | VAN | PEN | CEF | MET | |||||||
| 1 | 48/M | Hong Kong | Partial small bowel obstruction with secondary sepsis/CKD | AN (Day 3) | No | Cefuroxime & Metronidazole | Recovered | 2 [S] | 0.75 [S] | >32 [R] | <0.016 [S] | [1] |
| 2 | 39/M | Hong Kong | Acute appendicitis with perforation | AN (Day 3) | Yes | Cefuroxime & Metronidazole | Recovered | 2 [S] | 0.5 [S] | >32 [R] | <0.016 [S] | [1] |
| 3 | 74/M | Canada | Fever post exchange of biliary stent/plasmacytoma | NS | No | Ciprofloxacin | Recovered | 2 [S] | 4 [R] | >32 [R] | <0.016 [S] | [1] |
| 4 | 66/F | Canada | Fever, sepsis syndrome/metastatic cancer of the lung | AN (Day 5) | No | Cefuroxime & Ciprofloxacin | Died | 2 [S] | 4 [R] | >32 [R] | <0.016 [S] | [1] |
| 5 | 52/M | France | Intestinal perforation peritonitis, septic shock | AN (Day 3) | Yes | Amoxicillin-clavulanate & gentamicin | Died | <0.016 [S] | 2 [R] | >32 [R] | <0.016 [S] | [4] |
| 6 | 47/M | New Zealand | Acute appendicitis with perforation/ Perineal abscess | AN (Day 4) | No | Cefuroxime & Metronidazole, Amoxicillin-clavulanate | Recovered | - | 4 [R] | - [S] | - [S] | [5] |
| 7 | 91/F | Hong Kong | Sepsis, liver abscess/suspected GIT malignancy | AN (Day 3) | No | Ticarcillin-clavulanate & gentamicin | Died | 0.75–1.0 [S] |
< 0.016- 0.032 [S] |
> 32 [R] | < 0.016 [S] | [6] |
| 8 | 21/M | Hong Kong | Acute gangrenous perforated appendicitis | AN (Day 3) | No | Cefuroxime & metronidazole | Recovered | 0.75-1.0 [S] |
< 0.016- 0.032 [S] |
> 32 [R] | < 0.016 [S] | [6] |
| 9 | 81/F | Hong Kong | Sepsis/metastatic colon cancer | AN (Day 3) | No | Amoxicillin-clavulanate, piperacillin-tazobactam | Died | 0.75-1.0 [S] |
< 0.016- 0.032 [S] |
> 32 [R] | < 0.016 [S] | [6] |
| 10 | 76/M | Hong Kong | Acute calculous cholecystitis | AN (Day 3) | No | Cefuroxime & metronidazole | Recovered | 0.75-1.0 [S] |
< 0.016- 0.032 [S] |
> 32 [R] | < 0.016 [S] | [6] |
| 11 | 81/F | Hong Kong | Infected tumor/metastatic colon cancer | AN (Day 3) | No | Cefuroxime & metronidazole | Died | 0.75-1.0 [S] |
< 0.016- 0.032 [S] |
> 32 [R] | < 0.016 [S] | [6] |
| 12 | 55/M | Italy | Septic shock | AN (Day 4) | No | Vancomycin & Meropenem | Recovered | 0.75 [S] | - | - | ≤ 0.16 [S] | [7] |
| 13 | 77/M | South Korea | Acute cholecystitis | AN (Day 3) | Yes | Cefodizime & Metronidazole | Recovered | 0.5–0.75 [S] | > 32 [R] | > 32 [R] | - [S] | This report |
Abbreviations: AN, anaerobic bottle; MIC, minimum inhibitory concentration; CEF, cefotaxime; CKD, chronic kidney disease; GIT, gastrointestinal tract; MET, metronidazole; NS, not specified; PEN, penicillin; R, resistant for the agents on the basis of the CLSI clinical breakpoints for anaerobes; S, susceptible for the agents on the basis of the CLSI clinical breakpoints for anaerobes; VAN, vancomycin.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download