Abstract
Placenta accreta during the first trimester of pregnancy is rare. Only a few cases of placenta accreta manifesting as a uterine mass have been published. Most patients with placenta accreta present with vaginal bleeding during or after pregnancy. This report describes a patient with placenta accreta that caused vaginal bleeding three years after a first trimester abortion. The patient had regular menstruation for three years after the abortion. Initially endometrial cancer or a uterine myoma with degeneration was suspected. This is the first report of a placenta accreta detected as a uterine mass long after a first trimester abortion with delayed vaginal bleeding.
Placenta accreta is defined as abnormal adherence of the placenta to the uterus. It is subclassified into placenta accreta vera, placenta increta, and placenta percreta based on the depth of penetration of the placental tissue into the uterine wall [1]. The presentation of a placenta accreta after a dilatation and curettage is extremely rare; however, retained placental tissue and a hematoma can become entrapped in the myometrium. This condition is clinically significant because it can cause not only post-evacuation bleeding, but also can mimic an unusual uterine mass lesion.
We describe a woman who was diagnosed with placenta accreta after undergoing a hysterectomy due to heavy vaginal bleeding during curettage which manifested as uterine mass three years after dilatation and curettage for a first trimester abortion.
A 41-year-old gravida 4 para 2 with a history of 1 Cesarean section and 3 dilatation and curettages presented with a complaint of vaginal bleeding. Her cycles were regular initially and became irregular 1 year ago. She was diagnosed with premature menopause at a private clinic and sought evaluation at our hospital. She had 1 full-term vaginal delivery 18 years ago and 1 Cesarean section due to a breech presentation 9 years ago. Several years ago before the Cesarean section, she underwent a dilatation and curettage. Three and six years after the uneventful Cesarean section, she underwent a dilatation and curettage at a local clinic for pregnancies estimated to be about 5 weeks gestation.
Pelvic examination revealed a slightly enlarged uterus. Vaginal ultrasonography revealed a 7.8 × 6.6 × 4.1 cm well-defined complex solid and cystic mass in the uterine wall and there was no vascular flow in the lesion (Fig. 1). All laboratory finding was not remarkable. Serum level of estradiol, prolactin, lutenizing hormone, and follicular stimulating hormone (FSH) were 25.42 pg/mL, 4.8 ng/mL, 32.54 mIU/mL, and 66.13 mIU/mL, respectively. Serum level of β-human chorionic gonadotrophin (β-hCG) was 0.27 mIU/mL. The endometrial line was not visualized. Based on the history and sonographic findings, the differential diagnosis included an endometrial cancer or a uterine myoma with degeneration.
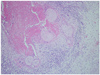
A diagnostic dilatation and curettage was performed. Friable tissue was recovered and frozen section revealed benign tissue. After evacuation, heavy uterine bleeding continued, and the blood pressure was 70/50 mm Hg, and the pulse rate was 130 beats per minute. An emergency hysterectomy was recommended with consent of the family. At the time of surgery, the uterine surface was shown to be smooth and there were no abnormal findings in the abdominal and pelvic cavity. Her vital signs recovered after transfusion of four units of packed red cells and two units of fresh frozen plasma. A total abdominal hysterectomy and incidental appendectomy were performed. The hysterectomy specimen showed a 9.0×6.0 cm red-brown mass adherent to the myometrium. The histopathlogic examination revealed a retained placenta accreta without atypical trophoblastic cells (Fig. 2). Her postoperative condition remained stable and she had a favorable progress. She was discharged 6 days later.
Placenta accreta is characterized by placental villi attaching to the uterine myometrium without intervening decidual membrane. Risk factors of placenta accreta include multiparity, placenta previa, a scarred uterus following a Cesarean section, prior dilatation and curettage, and miscarriage [2]. Severe adhesions of placenta accreta, increta, and percreta are very rare before 20 weeks gestation and rarer still in the first trimester. Most placenta accretas show clinical manifestations, such as bleeding, uterine rupture, invasion of the bladder, and uterine inversion [3]. Placenta accreta usually presents with vaginal bleeding during difficult placental removal in the third trimester. Severe forms of placenta accreta, such as placenta increate, may complicate first and early second trimester pregnancy losses, causing profuse post-curettage hemorrhage. Our case also showed heavy uterine bleeding during curettage and it is thought to be caused by the placenta accreata. Although there are several reports of placenta accreta during or after first trimester pregnancy termination [4-8], cases with retained placenta accreta for a long time without any symptoms have not been reported. Most previous reports involved a placental abnormality diagnosed during curettage in the first trimester, in that hysterectomy was required. Our patient had regular menstrual cycles after the last dilatation and curettage, so placenta accreta was not suspected initially. Her serum FSH level was 66.13 mIU/mL and it suggests that this isn't complication of recent pregnancy but complication of past pregnancy. Moreover, her serum ß-hCG level was within normal range. Because she presented with vaginal bleeding associated with a solid uterine mass, endometrial cancer or a uterine myoma with degeneration were the initial diagnoses. There is one reported case of placenta increta detected as a solid uterine mass after a first trimester dilatation and curettage [5]; however, the interval between the dilatation and curettage and the detection of the uterine mass was just 2 weeks in the prior case. This is the first report of a placenta accreta detected several years after a first trimester pregnancy termination with delayed vaginal bleeding.
With extensive involvement of the placenta accreta and deep myometrial invasion, such as placenta increta, hemorrhage becomes profuse as delivery of the placenta is attempted. Successful treatment depends on immediate blood replacement therapy and prompt hysterectomy. In the past, the most common form of conservative management was manual removal of as much of the placenta as possible and packing of the uterus. But, conservative treatment is probably appropriate only for partial placenta accreta in which bleeding is minimal. Alternative measures include uterine or internal iliac artery ligation or angiographic embolization [9].
In conclusion, placenta accreta may present after a first trimester pregnancy termination and also may present as a solid uterine mass mimicking endometrial cancer or a uterine myoma. If clinical manifestations, such as vaginal bleeding, do not occur immediately after pregnancy termination, the diagnosis of a placental abnormality may be difficult.
Figures and Tables
References
1. Breen JL, Neubecker R, Gregori CA, Franklin JE Jr. Placenta accreta, increta, and percreta: a survey of 40 cases. Obstet Gynecol. 1977. 49:43–47.
2. Read JA, Cotton DB, Miller FC. Placenta accreta: changing clinical aspects and outcome. Obstet Gynecol. 1980. 56:31–34.
3. Haynes DI, Smith JH, Fothergill DJ. A case of placenta increta presenting in the first trimester. J Obstet Gynaecol. 2000. 20:434–435.
4. Arredondo-Soberon F, Sabella V, Garza-Leal J, Valente PT. Placenta accreta during the first trimester of pregnancy: a case report. Ginecol Obstet Mex. 1995. 63:279–281.
5. Ju W, Kim SC. Placenta increta after first-trimester dilatation and curettage manifesting as an unusual uterine mass: magnetic resonance findings. Acta Radiol. 2007. 48:938–940.
6. Haider P. Placenta percreta in early gestation. J Pak Med Assoc. 1990. 40:274–275.
7. Gist RS, Vuong V, Brody S, Rees P, Landry AD. Placenta increta occurring in a blighted ovum. South Med J. 1996. 89:545–547.
8. Woolcott RJ, Nicholl M, Gibson JS. A case of placenta percreta presenting in the first trimester of pregnancy. Aust N Z J Obstet Gynaecol. 1987. 27:258–260.
9. Kayem G, Davy C, Goffinet F, Thomas C, Clement D, Cabrol D. Conservative versus extirpative management in cases of placenta accreta. Obstet Gynecol. 2004. 104:531–536.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download