Abstract
We report transradial access (TRA) for emergency carotid artery stenting (CAS) as a useful alternative when the femoral artery cannot be accessed. A 63-year-old man arrived at our emergency room 30 minutes after left hemiplegia and loss of consciousness. Brain computed tomography (CT) anigograpy showed occlusion of the right interntal carotid artery (ICA) and CT perfusion revealed delayed time-to-peak in the territory of the middle cerebral artery. For, endovascular treatment, trans-femoral access (TFA) was attempted but failed due to occlusion of the abdominal aorta. So, we changed access route via radial artery and confirmed proximal ICA dissection. CAS was attempted via TRA and it was successfully performed. Final angiography showed recanalization of ICA and patient was clinically improved.
The classic treatment goal for carotid stenosis caused by atherosclerosis is inhibition of progression through medication and, most importantly, prevention of cerebral infarction. Carotid endarterectomy is the primary treatment method in cases of severe stenosis requiring surgical intervention. However, carotid artery stenting (CAS) has become an effective treatment in recent years due to technical development of protective embolic devices, carotid stents, and increased experience of endovascular surgeons.6) CAS has high clinical utility, especially in cases of acute infarction with major cerebrovascular occlusion, high-risk carotid endarterectomy, and elderly patients with underlying disease. Transfemoral access (TFA) is the basic and most popular route of vascular access for CAS but is not always be feasible. Here, we report transradial access (TRA) for emergency CAS due to abdominal aortic occlusion in the case of ICA dissection.
A 63-year-old man suffered from Lt. hemiplegia and loss of consciousness 30 minutes prior to visiting our emergency room. The patient had a 60 pack-year smoking history but was healthy with no other underlying disease. His Glasgow coma scale (GCS) was 6 and National Institutes of Health Stroke Scale (NIHSS) score was 25. Although brain computed tomography (CT) did not show abnormal high or low signal density, CT angiography and perfusion showed the occlusion of Rt. internal carotid artery (ICA) and marked time to peak delay in the territory of the middle cerebral artery (Fig. 1). Tissue plasminogen activator was injected through an intravenous line. Magnetic resonance diffusion weighted image did not show diffusion restriction and then the patient was transferred to the angiography suite for endovascular revascularization.
We punctured the Rt. femoral artery; however, we were unable to advance the guide wire. In addition, we could not identify the vascular structure of the femoral artery despite injection of angiographic contrast. We decided to change access route from femoral to radial artery. After adjusting the positioning and draping the patient, the Rt. radial artery was punctured, and a 7 cm, 6-Fr arterial sheath (RADIFOCUS® INNTRODUCER II; Terumo Medical Corp, Tokyo, Japan) was inserted. Radial angiography using a 100 cm, 5-Fr SIM2 diagnostic catheter (Terumo Medical Corp, Tokyo, Japan) confirmed the absence of vascular stenosis and collaterals from the ulnar artery to the palmar arch. Because of dual supply to the hand, TRA should be performed only in patients with a documented patent ulnar artery and palmar arch to avoid the ischemic complication. To determine why TFA failed, we performed an abdominal aortic angiogram. We identified an abdominal aortic occlusion just distal to the origin of the renal arteries (Fig. 2A). A tapered steerable 0.035" guidewire (RADIFOCUS® GUIDE WIRE M; Terumo Medical Corp, Tokyo, Japan) was then advanced to the Rt. external carotid artery (ECA), and a 100 cm, 5-Fr SIM2 diagnostic catheter was positioned at the Rt. common carotid artery (CCA) (Fig. 2B). After positioning of the 90 cm, 6-Fr guiding catheter (ENVOY® Guiding Catheter; Codman, Workingham, UK) at the Rt. proximal CCA, common carotid angiography revealed the dissection of Rt. ICA (Fig. 2C). A distal embolic protection device (EPD) (SpiderFX Embolic Protection Device; ev3, Plymouth, MN, USA) was deployed at the proximal site in petrous ICA using a 0.014" mirowire (Transend 300 guidewire with ICE Hydrophilic coating; Boston Scientific, Natick, MA, USA). A self-expanding carotid stent (5 mm × 30 mm, Cordis PRESISE® PRO Rx Nitinol Stent System; Cordis Corporation, FL, USA) was deployed at the cervical ICA. Final digital subtraction angiography (DSA) showed recanalization of the Rt. ICA (Fig. 2D), and the PED was removed. The time taken to reperfusion from occurring symptoms was 160 minutes. On completion of endovascular treatment, the patient was transferred to the intensive care unit. He was clinically improved immediately. NIHSS score was 12 at the 90-day follow-up.
CAS is a reasonable alternative to carotid endarterectomy. When performed by experienced endovascular surgeons, the stability and effectiveness of CAS are well established.2)7) In particular, CAS has high efficacy in acute ischemic stroke accompanied by carotid artery stenosis or dissection. TFA remains the basic and popular vascular route for CAS; however, it can increase the risk for embolic complication in severe aorto-iliac stenosis and, in some cases, might not be feasible for a number of reasons. Thus, under special circumstances, it might be necessary to use TRA, the efficacy and safety of which have been demonstrated in cardiovascular interventions.4)5)
The brachial artery courses down the medial aspect of the arm to the antecubital fossa and then typically bifurcates into the ulnar and radial artery. These two arteries form the palmar arch. The radial artery is usually palpated in the styloid process of radius. The mean diameter of right radial artery was 2.3 mm.1) The Rt. radial artery is the primary access route because most operators are right-handed and typically stand on the right side of the patient. In addition, navigation of the aortic arch through the Rt. radial artery is easier than through the Lt. In cases where the angle of the Rt. subclavian artery and Rt. CCA is less than 45 degrees, contralateral TRA reduces kinking of the guiding catheter and is safer because it reduces device entrapment and fracture.
In performing TRA, it is important to verify arterial pumping after puncture, followed by insertion of the mini guide wire and subsequent replacement with a 7 cm, 6-Fr or 7-Fr arterial sheath. When the pumping is unclear or if resistance of the guide wire is noted, it is safer to insert the sheath after confirming whether the mini guide wire is positioned in the normal arterial path through fluoroscopy. In addition, a cocktail solution containing 200 micrograms of nitroglycerin can be injected into the radial artery to prevent vasospasm. However, if vasospasm occurs, it is necessary to wait for approximately 5 to 10 minutes after administering the cocktail. Omitting this process increases the risk of radial artery dissection.
A 6-Fr or 7-Fr guiding catheter (ENVOY® Guiding Catheter; Codman, Workingham, UK) is the most common device used in this procedure. If a 7-F guiding catheter is used, angiography is necessary to verify the status of the radial artery after inserting a 6-F guiding catheter. In addition, it is safer to replace the 6-Fr catheter with a 7-Fr catheter after a period of time. Lastly, after placing the guiding catheter in the carotid bifurcation adjacent to the CCA, stability should be verified, similar to TFA.
Through the brachial artery and the subclavian artery, a tapered steerable 0.035" guidewire is sometimes placed in the right common carotid artery directly at the brachiocephalic bifurcation. This is rarely possible if the angulation of the subclavian artery and the right common carotid artery is not tortuous severely. In the aortic cusp, a 0.035" guidewire is looped prior to placing a 100-cm, 5-Fr SIM2 diagnostic catheter in the same loop. After removing the guide wire, a unique U shape of the SIM2 5F catheter is formed in the ascending aorta. At this time, by rotating the catheter slowly in a clockwise direction, a twisted U shape is created. By then slowly pulling the catheter back, the orifice of the brachiocephalic artery can be entered. While the catheter is pulled back and slowly rotated in a counterclockwise direction, the catheter tip can be entered into the CCA. After entering the 0.035" guide wire into the ECA, the SIM2 5F catheter can be slowly placed in the CCA. Likewise, by slowly advancing the guiding catheter, it can be placed in the common carotid artery in most cases without difficulty. Lt. CAS is also possible using the same method; however, due to excessive tension, the wire might be pushed through the aortic arch when entering the guiding catheter. In that case, one can replace a tapered steerable 0.035" guide wire with a long 0.035'' extra stiff guide wire (Amplatz SuperStiff Guidewire, Boston Scientific, Natick, MA, USA), which makes it easier to position the guiding catheter due to the stronger supporting force. Of course, in cases of a bovine aortic arch, it might be easier to directly engage with the guiding catheter.
When performing Rt. CAS, if the guiding catheter is being pushed into the proximal brachiocephalic artery, it can be engaged in a retrograde manner with the Rt. CCA. In other words, as the guiding catheter is sequentially advanced for three points consisting of the brachiocephalic artery, aortic cusp, and Rt. CCA, it can be used to form a loop in the aortic cusp (Fig. 3). This approach can be considered when the stability of the catheter is compromised due to excessive tension during a direct engagement technique. A usual guiding catheter is commonly used in this technique; however, if the patient is taller than 165 cm, it might be necessary to use a longer catheter.
EPDs and stents are deployed according to conventional methods using a road mapping system (Siemens AXIOM-Artis VB35D, Berlin, Germany). During TRA, it is important to not only visually verify placement with fluoroscopy, but also for the operator to be sensitive to excessive resistance while manipulating the instrument, because the guiding catheter is positioned at a severe angle compared to TFA in most cases. Pre-dilation and post-dilation with a balloon can be used in some cases. Final extra- and intracranial angiography is performed after the EPD is recaptured.
After approximately three minutes of manual compression, the puncture site can be closed with a "figure-X" bandage, which can be removed the following morning. If there are no abnormal findings on post-procedural CT and/or MR. At this time, early ambulation of the patient should be encouraged, and the patient can resume an unrestricted diet.
While TRA can be a more efficient technique compared to TFA, it has several shortcomings. First, access from the radial artery to the common carotid artery can be difficult because of the vascular anatomy. Possible difficulties when performing Lt. CAS include an aortic arch with an parallel angle between the Rt. brachiocephalic trunk and Lt. proximal CCA, as well as a short distance between these arteries. In rare cases, TRA can fail. Therefore, it is necessary to increase the operators' technical proficiency by performing transradial DSAs. Second, the distal part of the guiding catheter is advanced to a considerable depth in proximal CCA to ensure the stability of the catheter. As such, transradial CAS is less applicable in proximal common carotid lesions and severe ostial common carotid lesions. Third, a small-diameter system should be used in TRA. In the past, only large-bore catheters for TFA were available; however, recent advances in technology have eliminated this difficulty. Indeed, most carotid stents are available in a 5-6 Fr-diameter, and most EPDs are available in 6-7 Fr-diameter. By fully understanding the mechanisms of instruments used in cardiovascular interventions, it is possible to increase safety and success rates. Lastly, one should be cautious about manipulation of instruments in the guiding catheter when there is a severe angle relative to the TFA during retrograde engagement, as fracture of the EPD wire can occur in such cases.3)
Transradial CAS is a successful alternative to Transfemoral approach in patients with abdominal aortic occlusion. However, because TRA is infrequently used as an endovascular procedure, operator unfamiliarity is a significant concern. Thus, it is important for surgeons to become familiar with the instruments and techniques of Transradial approach prior to conducting the procedure.
References
1. Ashraf T, Panhwar Z, Habib S, Memon MA, Shamsi F, Arif J. Size of radial and ulnar artery in local population. J Pak Med Assoc. 2010; 10. 60(10):817–819. PMID: 21381609.
2. Brott TG, Hobson RW 2nd, Howard G, Roubin GS, Clark WM, Brooks W, et al. Stenting versus endarterectomy for treatment of carotid-artery stenosis. N Engl J Med. 2010; 7. 363(1):11–23. PMID: 20505173.

3. Fang CC, Jao YT, Wu CJ. Filter wire fracture during transradial carotid stenting. Int J Cardiol. 2014; 9. 176(2):e66–e69. PMID: 25112545.

4. Louvard Y, Lefevre T, Allain A, Morice M. Coronary angiography through the radial or the femoral approach: The CARAFE study. Catheter Cardiovasc Interv. 2001; 2. 52(2):181–187. PMID: 11170325.

5. Mann T, Cubeddu G, Bowen J, Schneider JE, Arrowood M, Newman WN, et al. Stenting in acute coronary syndromes: a comparison of radial versus femoral access sites. J Am Coll Cardiol. 1998; 9. 32(3):572–576. PMID: 9741495.

6. Pieniazek P, Musialek P, Kablak-Ziembicka A, Tekieli L, Motyl R, Przewlocki T, et al. Carotid artery stenting with patient- and lesion-tailored selection of the neuroprotection system and stent type: early and 5-year results from a prospective academic registry of 535 consecutive procedures (TARGET-CAS). J Endovasc Ther. 2008; 6. 15(3):249–262. PMID: 18540694.
7. Silver FL, Mackey A, Clark WM, Brooks W, Timaran CH, Chiu D, et al. Safety of stenting and endarterectomy by symptomatic status in the Carotid Revascularization Endarterectomy Versus Stenting Trial (CREST). Stroke. 2011; 3. 42(3):675–680. PMID: 21307169.

Fig. 1
CT angiography and perfusion showed the occlusion of Rt. ICA and marked time to peak delay in the territory of the middle cerebral artery. ICA = internal carotid artery.

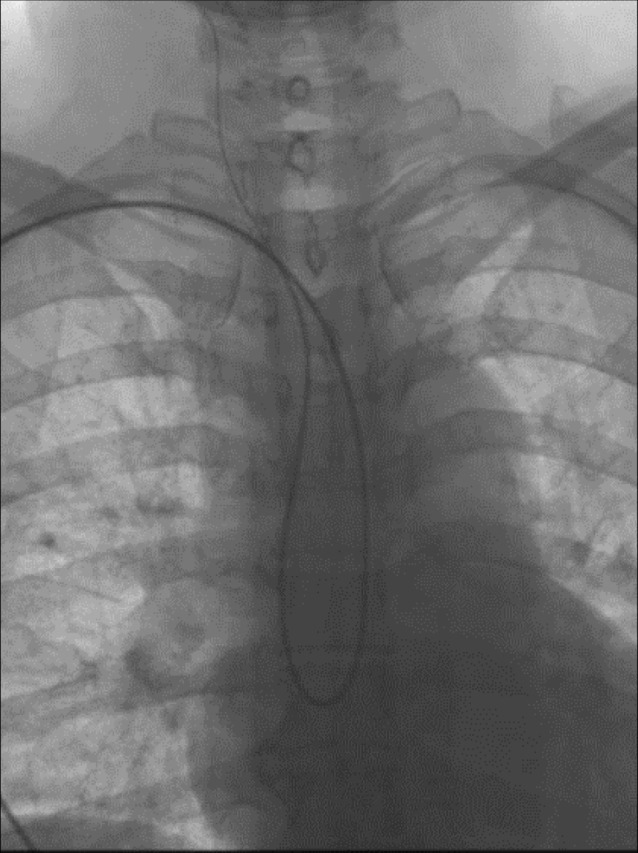
Fig. 2
(A) An abdominal aortic angiogram showed an abdominal aortic occlusion just distal to the origin of the renal arteries. (B) A 100 cm, 5-Fr SIM2 diagnostic catheter was positioned at the Rt. CCA (C) After positioning of the 90 cm, 6-Fr guiding catheter at the Rt. proximal CCA, common carotid angiography revealed an dissection of the Rt. ICA. (D) A self-expanding carotid stent was deployed at the cervical ICA. Final DSA showed recanalization of the Rt. ICA. CCA = common carotid artery; ICA = interntal carotid artery; DSA = digital subtraction angiography.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download