Abstract
Purpose
The objective of this study was to compare the outcomes of surgical mini-implant placement when potential mini-implant sites were scanned using a lower-dose 180° acquisition protocol versus a conventional 360° acquisition protocol.
Materials and Methods
Ten dentate human skulls were used to provide sites for potential mini-implant placement. The sites were randomly divided into 2 groups: 360° and 180° cone-beam computed tomography (CBCT) acquisition protocols. A small-volume 180° CBCT scan and a 360° CBCT scan of each site were acquired using a Morita Accuitomo-170 CBCT machine and then a mini-implant was placed. A follow-up 360° CBCT scan was done as a gold standard to evaluate the location of the mini-implant and root perforation. Two raters evaluated the scans.
Results
Ninety-eight percent of the mini-implants placed did not perforate any root structure. Two percent of the sites had an appearance suggestive of perforation. On a Likert scale, both raters agreed that their subjective evaluation of the diagnostic quality of the protocols, ability to make and read measurements of the sites, and preferences for the specified diagnostic task were comparable. The Cohen kappa showed high inter-rater and intra-rater agreement.
Mini-implants, also known as temporary anchorage devices or mini-screws, are an alternative method for orthodontic anchorage that has become increasingly popular in orthodontics over the last few years.12 This trend has gained significant popularity owing to the ease of placement and removal of these devices, along with their low cost and minimal requirements for patient compliance.12 A mini-implant in this context can be defined as a device fixed to bone in order to reinforce or eliminate the need for dental anchorage. It is subsequently removed once the optimal positioning of the desired teeth is obtained. In situations where patients exhibit loss of teeth and/or periodontal support, mini-implants can contribute to the success of a treatment that would not be possible using traditional forms of anchorage.3 Mini-implants are increasingly being used when the teeth and supporting structures lack adequate quantity and quality, as often seen in cases pertaining to adult orthodontics. Additionally, they may be used when extra-oral devices are impractical, worries about aesthetics are a factor, or the likelihood of patient compliance is low.4 The benefits of using mini-implants over traditional orthodontic anchorage methods include the resistance to reactive orthodontic forces provided by close bone contact.5 However, the surgical placement of these mini-implants is critical to the success of treatment. It has been suggested that the safest area to place a mini-implant is between the maxillary second premolar and first molar and the mandibular first and second molar,6 but several important anatomical structures are located within these recommended areas. Factors that should be considered for the placement of mini-implants are soft tissue status and anatomy and, more importantly, inter-radicular distance, location of the inferior alveolar nerve, buccal and lingual/palatal bone thickness, and sinus morphology.378 If the placement of mini-implants is not carefully performed, several risks can arise. These include root resorption, local bony or soft tissue infections, greater palatine nerve damage in the palate, inferior alveolar or mental nerve damage in the mandible, and perforation of the nasal cavity or maxillary sinus.39 Therefore, for a thorough understanding of the anatomic structures associated with potential mini-implant sites, an effective treatment plan that takes the above factors into consideration is necessary. Although no firm protocols have been established for the imaging and placement of mini-implants, the current method seems to be either blind placement or placement with the use of periapical radiographs.10 In a previous study conducted by Landin et al.,10 it was demonstrated that placing these implants blind or with the help of a periapical radiograph resulted in the occurrence of root perforation in 50% and 60% of cases, respectively. Their study demonstrated that 2-dimensional imaging provided insufficient information regarding the inter-radicular space, root morphology, thickness of cortical bone, and position of the inferior alveolar nerve. Furthermore, their study revealed that 3-dimensional (3-D) information obtained using small-volume cone-beam computed tomography (CBCT) was superior for preventing root perforation during the surgical placement of mini-implants. CBCT provides a 3-D view of the area of interest and aids in the precise placement of the mini-implant. While 3-D imaging has gained significant popularity and is being increasingly used in clinical dentistry, the ionizing radiation dose remains a serious concern. This is more serious in pediatric and adolescent patients, as they are a more vulnerable population group. An easy solution for reducing the radiation dose would be to reduce the values of the exposure parameters. However, doing so would pose the challenge of reduced image resolution. The key is to establish a balance between reduced radiation exposure and resolution so that there is no compromise in the diagnostic quality. In this study, we explored the diagnostic efficacy of a CBCT acquisition protocol that images the area of interest by going around the head 180° as compared to the conventional method of going around the area of interest 360°. The key feature of this protocol is that it images the patient by only scanning the posterior aspect of the skull, and then advanced filtered back projection algorithms are used to produce a composite 360° image. This reduces the total number of basis projections acquired and also avoids direct X-ray exposure to the eyes and the thyroid gland, which tend to have a higher radiosensitivity weighting factor. This protocol significantly reduces the total effective dose delivered. The objective of this study was to evaluate this modified CBCT acquisition protocol that only uses a 180° rotation with a reduced number of basis projections to acquire 3-D information about the imaged area.
Ten dentate human skulls, obtained from the Department of Anatomic Sciences at the University of Connecticut School of Dental Medicine, were used to provide 20 maxillary and 20 mandibular sites for potential mini-implant placement. The criterion for selecting the skulls was that the skulls had the first and second molars in the mandibular arch, the first molars, and the second premolars in the maxillary arch. To simulate the presence of soft tissue at the site, a rubber dam sheet, measuring 10 cm×10 cm with modeling wax on its surface, approximately 1 mm in thickness, was taped to the potential anchorage site prior to any imaging. An 8-mm self-tapping IMTEC Ortho Implant (3M Europe N.V./S.A. Diegem, Brussels, Belgium) with a modified buttress thread form was used as the mini-implant.
Implant sites were imaged using a 360° rotational acquisition CBCT protocol and a 180° rotational acquisition CBCT protocol. To reduce artifacts from metal, any springs/screws in the skulls were removed prior to radiographic imaging. CBCT images were acquired using a single CBCT machine, Accuitomo-170 (J Morita Corp., Kyoto, Japan), with the standard exposure parameters (90 kVp, 10 mA) with a 40 mm×40 mm focused field of view (approximately 3-4 teeth) for the 360° acquisition. The acquisition time for the 360° scan was 19.8 seconds. The low-dose scans were obtained with 60 kVp and 2 mA. The acquisition time for this protocol was 9 seconds. Following acquisition, 3-D image volumes were reconstructed using i-Dixel reconstruction software (J Morita Corp., Kyoto, Japan) provided by the manufacturer. A follow-up post-implant placement 360° CBCT scan served as the gold standard to evaluate the final implant location and whether any root perforation was present.
To simulate soft tissue depth and to serve as a bleeding point for mini-implant placement as in real-life clinical situations, 1 mm of a modelling compound (Play-Doh, Hasbro Inc., Cincinnati, OH, USA) was evenly placed on both arches of each skull from the alveolar crest to the apex of the root in each of the 4 quadrants (Fig. 1). The implant sites were chosen to be in previously identified safe zones, between the second premolar and first molar in the maxilla and the first and second molar in the mandible.6 For every quadrant in each skull, 2 CBCT scans (a 360° and 180° rotation) were made with a small field of view (40×40 mm) using the CBCT machine. To maintain control over the location and standardization of the scans, they were taken consecutively per site, only changing the acquisition protocol of the scanner to the low-dose protocol. A sample size of 20 sites (5 maxillary and 5 mandibular sites for each arch) per group was evaluated, for a total of 40 sites. The sites were randomly divided into 2 groups, corresponding to the 360° and 180° CBCT acquisition protocols.
In the first group, at each maxillary and mandibular site, a conventional 360° CBCT scan was used to assess the potential anchorage site prior to mini-implant placement (Fig. 2). Post-processing reconstruction was done to evaluate the area of interest 3-dimensionally (Fig. 3). Using the measurement tool in the i-Dixel reconstruction software (J Morita Corp., Kyoto, Japan), the exact midroot location and inter-radicular space were found (Fig. 4). In the axial view, the inter-radicular space was re-measured and the potential mini-implant placement site was determined (Fig. 5). The path of insertion was determined based on the axial view and a measurement from the buccal cortical plate to the lingual cortical plate. A bleeding point was marked on the simulated Play-Doh to indicate the location of mini-implant placement (Fig. 6). An 8-mm mini-implant was placed approximately mid-root between the first and second molars in the mandibular arch and between the first molar and second premolars in the maxillary arch (Fig. 7). A round bur (0.9-mm diameter) with a high-speed contra-angle hand piece was used by a single operator to perform the osteotomies. A follow-up 360° CBCT exam was done as a gold standard to evaluate the mini-implant placement and root perforation (Fig. 8). In the second group, the low-dose acquisition protocol was used to plan mini-implant placement, and a follow-up 360° CBCT scan was done after placement to evaluate the mini-implant location and root perforation.
One board-certified oral and maxillofacial radiologist and a board-certified orthodontist analyzed the images to assess the proximity and/or perforation of root structures, the inferior alveolar nerve canal, and the maxillary sinus by the mini-implant. The images were displayed on a radiology workstation powered by a HP Pavilion ZE 2000 computer (HP Inc., Palo Alto, CA, USA) and a 20-inch dual-monitor display with a resolution of 1600×900 pixels (HP Compaq LA2205wg, Palo Alto, CA, USA). The viewing conditions (room lighting and display monitor settings) were standardized. Examiners were allowed to manipulate the density, contrast, and magnification to simulate actual radiological practice. Prior to starting the image analysis, both examiners were calibrated using a set of 6 images selected from the experimental data set. Each examiner analyzed the images independently. Analyses were done twice, with at least 2 weeks between the sessions. The statistical analysis was conducted using GraphPad (Prism Version 7, La Jolla, CA, USA). The main objective was to evaluate the statistical significance of our results to identify trends that were not due to chance alone. The interexaminer reliability was calculated using the Cronbach alpha. The sensitivity and specificity of the 2 different scanning protocols (180° and 360°) for visualizing the sinus pathology were recorded as percentages and compared with the McNemar test. The statistical significance between the 2 imaging protocols was calculated using the 2-tailed Student t test. Forty sites were examined for root perforation in the maxilla and the mandible.
The overall interexaminer reliability values (Cronbach alpha) were 96% for the 180° rotational acquisition. The interexaminer reliability for the 360° imaging protocol was 98%. We also examined root perforation, and found that 98% of the mini-implants placed did not perforate any root structure and that 2% of the sites had an appearance suggestive of perforation. This was challenging to determine, as the area in question was very close to the root and possibly in the periodontal ligament space. Both evaluators also examined root resorption and found no statistically significant difference (P>.05) between the 2 imaging protocols in the detection of root resorption. The overall specificity was 100% for both acquisition protocols. On a Likert scale, both raters agreed that although there was a slight reduction in the overall resolution of the 180° rotational acquisition, there were no concerns regarding the diagnostic capabilities of either acquisition protocol. Their subjective evaluations of the diagnostic quality of the protocols, the ability to make and read measurements of the sites, and preferences for the specified diagnostic task were comparable. The 360° imaging protocol for this specific diagnostic task was not found to be superior to the 180° rotational acquisition.
Three-dimensional visualization of the area of interest is advantageous for performing many surgical procedures in areas close to several critical structures, the perforation of which may lead to unwanted complications. Root perforation and resorption is a major concern when placing mini-implants, as estimating the amount of inter-radicular distance and gauging the quality of bone is very challenging, especially if the procedure is performed without any preoperative imaging or using a 2-dimensional imaging method. Three-dimensional imaging can solve this issue to a large extent, but the radiation dose remains a concern. A critical balance must be struck by reducing the dose while not compromising the quality of the image for the diagnostic task at hand. CBCT machines deliver a significantly lower radiation dose than conventional multi-slice medical CT.1112 While CBCT is considered a low-dose imaging modality in 3-D imaging, it delivers a dose higher than that of intraoral periapical or panoramic imaging. CBCT scanners traditionally acquire the scan with a 360° sweep around the patient. Next-generation scanners now offer the ability to scan using a 180° rotation. The evolution of newer acquisition protocols allowed for imaging the entire head with only a 180° rotation, because during post-processing, advanced algorithms reconstruct the scanned volume.13 The 180° acquisitions have a significantly lower number of basis projections, which helps in dose reduction.141516 Furthermore, the 180° sweep focuses on the back of the head, thus sparing the more radiosensitive organs in the front, such as the eyes and the thyroid gland.11 Typically, when there are fewer basis projections, the image quality is slightly poorer, so our study evaluated whether this drop in the number of basis projections with this modified protocol had any effect on the observers' ability to reliably evaluate the potential implant site. We found that the reduced number of projections did not affect our ability to evaluate the potential mini-implant sites. An additional advantage to having a fewer number of basis projections is that it also slightly reduces the amount of scatter artifacts that come from metallic structures in the field of view, such as metallic restorations, implants, and orthodontic wires and brackets. While optimizing the field of view and reducing the number of basis projections reduce the radiation dose delivered, reducing the total tube current can also contribute to a significant dose reduction. The challenge of reducing the tube current too much is that doing so results in a significant increase in the contrast-to-noise ratio, which can compromise the diagnostic quality of the image. In this study, we reduced the tube current to 2 mA in the 180° scans, as compared to the normal acquisition technique of 60-80 kVp and 8-10 mA, to further reduce the dose. Despite this reduction, the images were still found to be of sufficient diagnostic quality. While a conventional 360° rotational scan with a higher tube current and smaller voxel size may be necessary for detecting the extent of pathological lesions, the evaluation of fractures, the assessment of smaller arthritic changes, or other tasks that need high resolution and low image noise, for tasks such as evaluating inter-radicular distance, root morphology, and distance from critical structures such as the inferior alveolar nerve canal and the maxillary sinus, a 180° scan may be able to provide the necessary information. Another advantage of this acquisition technique is that it reduces the total acquisition time to 9 seconds, as compared to 17.5 seconds with a traditional 360° acquisition format. Furthermore, it also reduces the total reconstruction time and file size.
In conclusion, in this ex vivo study, we found that the 180° rotational acquisition protocol was as effective as the conventional 360° rotational acquisition protocol for the preoperative evaluation of potential mini-implant sites.
Figures and Tables
Fig. 2
A. Preoperative 360° small volume cone-beam computed tomography (CBCT) rotational scan of the mini-implant placement site. B. Preoperative 180° rotational small-volume CBCT scan of the mini-implant placement site.
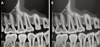
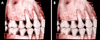
Fig. 3
A. Preoperative volumetric rendering of the 360° small-volume cone-beam computed tomography (CBCT) scan of the mini-implant placement site. B. Preoperative volumetric rendering of the 180° small-volume CBCT scan of the mini-implant placement site.
Acknowledgements
The authors would like to acknowledge the support of Mr. Tom Casso from the Department of Anatomic Sciences for providing us the specimens and for his unconditional support.
References
1. Upadhyay M, Yadav S, Patil S. Mini-implant anchorage for en-masse retraction of maxillary anterior teeth: a clinical cephalometric study. Am J Orthod Dentofacial Orthop. 2008; 134:803–810.

2. Upadhyay M, Yadav S, Nagaraj K, Patil S. Treatment effects of mini-implants for en-masse retraction of anterior teeth in bialveolar dental protrusion patients: a randomized controlled trial. Am J Orthod Dentofacial Orthop. 2008; 134:18–29.e1.

3. Bonnick AM, Nalbandian M, Siewe MS. Technological advances in nontraditional orthodontics. Dent Clin North Am. 2011; 55:571–584.

4. McCabe P, Kavanagh C. Root perforation associated with the use of a miniscrew implant used for orthodontic anchorage: a case report. Int Endod J. 2012; 45:678–688.

5. Papageorgiou SN, Zogakis IP, Papadopoulos MA. Failure rates and associated risk factors of orthodontic miniscrew implants: a meta-analysis. Am J Orthod Dentofacial Orthop. 2012; 142:577–595.e7.

6. Poggio PM, Incorvati C, Velo S, Carano A. “Safe zones” a guide for miniscrew positioning in the maxillary and mandibular arch. Angle Orthod. 2006; 76:191–197.
7. Brisceno CE, Rossouw PE, Carrillo R, Spears R, Buschang PH. Healing of the roots and surrounding structures after intentional damage with miniscrew implants. Am J Orthod Dentofacial Orthop. 2009; 135:292–301.

8. Hembree M, Buschang PH, Carrillo R, Spears R, Rossouw PE. Effects of intentional damage of the roots and surrounding structures with miniscrew implants. Am J Orthod Dentofacial Orthop. 2009; 135:280.e1–280.e9.

9. Cope JB. Temporary anchorage devices in orthodontics: a paradigm shift. Semin Orthod. 2005; 11:3–9.

10. Landin M, Jadhav A, Yadav S, Tadinada A. A comparative study between currently used methods and small volume-cone beam tomography for surgical placement of mini implants. Angle Orthod. 2015; 85:446–453.

11. Pauwels R, Beinsberger J, Collaert B, Theodorakou C, Rogers J, Walker A, et al. Effective dose range for dental cone beam computed tomography scanners. Eur J Radiol. 2012; 81:267–271.

12. Ludlow JB, Davies-Ludlow LE, White SC. Patient risk related to common dental radiographic examinations: the impact of 2007 International Commission on Radiological Protection recommendations regarding dose calculation. J Am Dent Assoc. 2008; 139:1237–1243.
13. Scarfe WC, Farman AG. What is cone-beam CT and how does it work? Dent Clin North Am. 2008; 52:707–730.

14. Lennon S, Patel S, Foschi F, Wilson R, Davies J, Mannocci F. Diagnostic accuracy of limited-volume cone-beam computed tomography in the detection of periapical bone loss: 360° scans versus 180° scans. Int Endod J. 2011; 44:1118–1127.





 PDF
PDF ePub
ePub Citation
Citation Print
Print








 XML Download
XML Download