Abstract
Endometriosis is defined as the presence of endometrial tissue (glands and stroma) outside the uterus. About 1% of women with endometriosis have urinary tract implantations, and 84% of these cases involve the bladder. Abdominal partial cystectomy has been reported to treat urinary tract implantations, but laparoscopy has not previously been reported in Korea. We report a case of vesical endometriosis that was treated successfully with laparoscopic partial cystectomy.
Endometriosis is the presence of endometrial tissue outside the uterus; it is especially common in the pelvic cavity and the peritoneum. Among the many different implantation sites, bladder endometriosis is very rare, occurring in less than 1% of women with endometriosis. For many years, bladder endometriosis has been treated with abdominal partial cystectomy. Due to its rarity, few studies have been done to develop an improved treatment plan. However, since laparoscopy is currently the primary modality for the diagnosis and treatment of endometriosis, a few cases of laparoscopically treated bladder endometriosis have been reported abroad [1-3]. Such treatment has yet to be reported in Korea until now; we report a case of bladder endometriosis successfully managed with laparoscopic partial cystectomy.
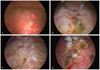
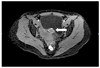
The patient visited a local hospital in Seoul due to dysuria during menstruation. She received six cycles of gonadotrophin-releasing hormone (GnRH) agonists, but her symptoms did not improve; thus, she referred to our outpatient clinic on December 11, 2010. Base on the results of a computed tomography (CT) scan, endometriosis was suspected, with a mass visualized on the posterior wall of the bladder. She was referred to the urology department for cystoscopy. The cystoscopy revealed a 3 cm mass on the posterior wall of the bladder. Transurethral resection of bladder was performed (Fig. 1) and the specimens were sent for frozen biopsy. The result was negative, but the final pathologic result revealed endometriosis. Therefore, the patient required further diagnostic laparoscopy and laparoscopic partial cystectomy.
Complete blood count (hemoglobin, 13.2 g/dL; white blood cell, 6,210/mm3; platelets, 225,000/mm3), chemistry, coagulation test, urinanalysis, cancer antigen (CA) 19-9 12.6, and CA 125 14.2 were all within normal range.
This was taken on December 13, 2010, showing a 3.1×1.6 cm-sized heterogeneous enhancing lesion on the posterior wall of the bladder (Fig. 2). On December 22, the follow-up CT showed that the lesion had decreased in size to 2.8×1.4 cm.
Focal wall thickening at the posterior wall of the bladder was noted, showing low signal intensity with high SI spots on T2WI (weighed image) and T1WI. Compared to the normal bladder wall, there was mild enhancement. A benign bladder tumor, rather than endometriosis, was suspected, and a differential diagnosis from leiomyoma, hemangioma, or neurofibroma was needed using the tissue biopsy from partial cystectomy.
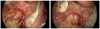
Under general anesthesia, diagnostic laparoscopy was done on March 28, 2011. Severe pelvic adhesions, including the rectum, the posterior vesical wall, and the uterus, were noted (Fig. 3). The bladder endometriosis was detected as a lesion of 1 cm that augmented to 3 cm on traction. The lesion was attached by well-vascularized dense adhesions to the uterine serosa. Further endometriotic lesions were seen on the bilateral sacrouterine ligament, the left part of the cul-de-sac infiltrating the rectum, and the sigmoid colon (endometriosis stage III). The uterus and both ovaries were grossly normal. On the right salpinx, a paratubal cyst of around 1×2 cm was found. The cyst was removed and a biopsy was done. The posterior vesical wall lesion was then marked by resectoscope, and prophylactic bilateral ureteral stent insertion was done. Laparoscopic partial cystectomy and adhesiolysis were done. All procedures were performed by Dr. KS Cho, a medical doctor from the urology department, with the assistance of gynecologists. Initially the vesicouterine peritoneal fold was opened transversely and the bladder was mobilized off the cervix and the upper vagina with sharp dissection to the level of the trigone. The scarred endometrial implant was then freed using Harmonic scalpel and scissors to excise the portion of bladder that was involved with endometriosis, together with the area of fibrotic bladder around it. This full thickness bladder resection came within 1 cm of the right ureteral orifice and extended into the right side of the trigone. The bladder was closed in three layers, using interrupted sutures with #3-0 and #2-0 Vicryl and a third running suture with #3-0 Vicryl. Closure was tested by instillation of methylene blue (150 mL). In addition, Interceed was left intraabdominally for adhesion prophylaxis. This turned out to have boundaries similar to the previous cystoscopically marked regions. The specimens were sent to the pathology department for frozen biopsy and the result was negative for malignancy. However, the final pathologic report revealed bladder endometriosis and a simple paratubal cyst on the right salpingeal lesion.
The patient was discharged four days after surgery with the Foley catheter in situ. On April 7, 2011, she came back to the hospital for a check-up; the cystography showed no dye extravasation from the bladder and the bilateral ureteral stents were in place. On April 21, 2011, the 24th postoperative day, her Foley catheter and the ureteral stents were removed. Her bone mineral density levels were within normal limits and she was eligible for three postoperative cycles of GnRH agonists followed by 6 months of oral progesterone therapy. With this surgical and medical treatment combination, she had no complications during the 12-month post-surgical follow-up.
Bladder endometriosis is a rare entity that involves the detrusor muscle and often affects the vesical wall transmurally [4]. There are a number of explanationhs regarding the pathogenesis of this disease, and the implantation of regurgitated endometrial cells is the most accepted theory. The bladder constitutes a privileged target for the implantation because it is located in the anterior cul-de-sac, which is a dependent portion of the pelvic cavity. The fact that bladder endometriosis is usually not observed in women with a retroverted uterus (because no dependent anterior cul-de-sac is present) supports this theory [5].
It is important to suspect vesical endometriosis when a patient has catamenial urinary symptoms, such as frequency, urgency, painful micturition, or vesical tenesmus. Symptoms usually appear to overlap with those of urinary tract infections, overactive bladder, interstitial cystitis and other similar diseases in women in which diagnosis is often delayed [6].
Several imaging studies are used for diagnosis, and pelvic ultrasonography can be the initial approach. The disease entity is viewed as a heterogeneous, hyperechoic, intraluminal, and usually conical vegetation, which protrudes from the posterior vesical wall or the dome. MRI and CT scans may confirm the ultrasonographical findings, but they are not known to add much more different or precise information to ultrasonography and cystoscopy [7,8].
In this case, using the cystoscopic approach, a solid mass with a hyperemic appearance and typical bluish, slightly raised cysts were seen on the surface. Biopsy of the lesion and the pathologic finding of the endometrial glands confirmed the diagnosis. But even if the results were negative, the diagnosis is not excluded. Transurethral resection is usually not recommended as a definite treatment because attempting to completely eradicate the transmural lesion may perforate the bladder [9].
Bladder endometriosis has two treatment options: medical and surgical. Surgical treatment is the definitive treatment for endometriosis since medical treatment is considered to be palliative and the recurrence rate is higher when the treatment is discontinued. However, because the main goal of treating bladder endometriosis is controlling symptoms, medical treatment is also highly effective and it is not always necessary to perform surgery. In this case, the patient was initially on a medical therapy (six cycles of GnRH agonists), but she experienced no symptom improvement. As we can learn from this case, when treatment is not satisfactory, physicians should consider the next option-surgical eradication.
In the past, abdominal surgery was the treatment of choice, but due to improvements in laparoscopic technology, laparoscopic partial cystectomy is becoming the new standard of treatment for bladder endometriosis. It has several advantages, such as allowing enhanced visualization of the pelvic anatomy for the adequate excision of all lesions, less bleeding, shortened operative time and hospital stay, a major reduction in postoperative pain, and decreased risk of postoperative morbidity [10]. Concomitant cystoscopy can be useful for better defining the margins of the endometriotic lesion to be resected, as demonstrated in this case [11].
In conclusion, when patients with bladder endometriosis do not experience satisfying effects with medical therapy, clinicians should move on to further evaluation and surgical treatment when it is needed. Further, with today's developing laparoscopic skills, we need to be up-to-date in treating even the rare cases, such as bladder endometriosis, with laparoscopy. There are a few cases reported to have been successfully treated with laparoscopic partial cystectomy around the world, but none were previously reported in Korea. Thus, we report one case in which a patient was satisfied with the result of laparoscopic partial cystectomy.
Figures and Tables
Fig. 1
(A) Cystoscopy reveals dark elevated lesions on the posterior wall of the bladder. (B) Resection of the lesions. (C) Resection in progress. (D) Final resectied lesions.
References
1. Prager M, Wilson T, Krüger K, Ebert AD. Laparoscopic extramucosal partial bladder resection in a patient with symptomatic deep-infiltrating endometriosis of the bladder. J Minim Invasive Gynecol. 2012. 19:113–117.
2. Kovoor E, Nassif J, Miranda-Mendoza I, Wattiez A. Endometriosis of bladder: outcomes after laparoscopic surgery. J Minim Invasive Gynecol. 2010. 17:600–604.
3. Walid MS, Heaton RL. Laparoscopic partial cystectomy for bladder endometriosis. Arch Gynecol Obstet. 2009. 280:131–135.
4. Berlanda N, Vercellini P, Carmignani L, Aimi G, Amicarelli F, Fedele L. Ureteral and vesical endometriosis. Two different clinical entities sharing the same pathogenesis. Obstet Gynecol Surv. 2009. 64:830–842.
5. Vercellini P, Frontino G, Pisacreta A, De Giorgi O, Cattaneo M, Crosignani PG. The pathogenesis of bladder detrusor endometriosis. Am J Obstet Gynecol. 2002. 187:538–542.
6. Bogart LM, Berry SH, Clemens JQ. Symptoms of interstitial cystitis, painful bladder syndrome and similar diseases in women: a systematic review. J Urol. 2007. 177:450–456.
7. Balleyguier C, Chapron C, Dubuisson JB, Kinkel K, Fauconnier A, Vieira M, et al. Comparison of magnetic resonance imaging and transvaginal ultrasonography in diagnosing bladder endometriosis. J Am Assoc Gynecol Laparosc. 2002. 9:15–23.
8. Kinkel K, Frei KA, Balleyguier C, Chapron C. Diagnosis of endometriosis with imaging: a review. Eur Radiol. 2006. 16:285–298.
9. Aldridge KW, Burns JR, Singh B. Vesical endometriosis: a review and 2 case reports. J Urol. 1985. 134:539–541.
10. Granese R, Candiani M, Perino A, Venezia R, Cucinella G. Bladder endometriosis: laparoscopic treatment and follow-up. Eur J Obstet Gynecol Reprod Biol. 2008. 140:114–117.
11. Seracchioli R, Mannini D, Colombo FM, Vianello F, Reggiani A, Venturoli S. Cystoscopy-assisted laparoscopic resection of extramucosal bladder endometriosis. J Endourol. 2002. 16:663–666.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download