Abstract
Purpose
To evaluate the clinical implications of subsequent ultrasound (US) for incidental thyroid lesions (ITLs) detected on positron emission tomography/computed tomography (PET/CT) in patients with non-thyroidal cancer.
Materials and Methods
We retrospectively searched for ITLs in 2703 patients with non-thyroidal cancer on 3226 PET/CT examinations. We divided the patients into two groups: US-performed and US-not performed groups. Diagnostic performance of US in detecting malignancy was analyzed according to the PET/CT findings.
Results
The incidence of ITLs on PET/CT in patients with non-thyroidal cancer was 8.4% (226/2703). Death rate from disease and stage were not significantly different between the groups. The malignant rate of ITLs that had cytopathology was 39% (22/57). All malignancies were primary thyroid cancers except for one metastasis. Overall diagnostic performance of US was 87% sensitivity, 66% specificity, 66% positive predictive value (PPV), and 89% negative predictive value (NPV). The diagnostic performance of US according to the PET/CT findings was probable benign on PET/CT (n = 9): 100% specificity, 100% NPV; suspicious malignant on PET/CT (n = 22): 75% sensitivity, 90% specificity, 90% PPV, 75% NPV; and undetermined on PET/CT (n = 26): 100% sensitivity, 94% specificity, 91% PPV, 100% NPV.
Incidental thyroid lesions (ITLs) detected on 18F-fluorodeoxyglucose (18F-FDG) positron emission tomography/computed tomography (PET/CT) are defined as incidentally found abnormalities in the thyroid gland on 18F-FDG PET/CT in patients with non-thyroidal disease (1). 18F-FDG PET/CT is increasingly used to evaluate localization, stage of primary index tumors, and follow-up for primary and metastatic lesions in patients with various kinds of malignancies (2). The current widespread use of 18F-FDG PET/CT in patients with non-thyroidal malignancies has resulted in an increase in detection of ITLs. The strategy for managing these lesions is important for predicting patient prognosis and cost-effectiveness.
Ultrasound (US) and subsequent US-guided fine needle aspiration (US-FNA) are widely recommended for evaluating ITLs to enhance diagnostic accuracy (3). However, the question arises if such a strategy is sensible in patients with underlying malignancies and various PET/CT findings. When abnormal lesions of the thyroid gland are present on 18F-FDG PET/CT, patients with non-thyroidal malignancies are justified for further evaluation, as compared to the healthy screening population. Therefore, subsequent US or US-FNA could possibly be overused. Sensitivity and specificity of 18F-FDG PET/CT to differentiate malignancies from benign thyroid lesions have been reported to be 60-80% and 66-91%, respectively (2). Although the diagnostic value of 18F-FDG PET/CT and US for abnormal thyroid lesions has been reported in many studies (3, 4, 5), no report has evaluated the diagnostic value of subsequent US according to 18F-FDG PET/CT findings for ITLs, particularly in patients with non-thyroidal malignancies, which are frequently encountered in clinical practice.
The purpose of this study was to evaluate the clinical implications and value of subsequent US for ITLs detected on 18F-FDG PET/CT in patients with non-thyroidal cancer according to 18F-FDG PET/CT findings.
This retrospective study was approved by our Institutional Review Board, and the informed consent requirement was waived. A total of 3226 18F-FDG PET/CT examinations in 2703 patients with non-thyroidal cancer were performed between March 2006 and March 2008 at the nuclear medicine department of our institution. The patients underwent 18F-FDG PET/CT for cancer staging before treatment, detection of distant metastasis, and localization of a recurrent tumor.
Patients with ITLs detected on 18F-FDG PET/CT were divided into a US-performed group in which subsequent US was performed to evaluate thyroid lesions after 18F-FDG PET/CT, and a US-not performed group in which subsequent US was not performed. Subsequent US was determined at the clinician's discretion. The two groups were compared with regard to age, death rate from disease, and non-thyroidal cancer stage.
US findings were analyzed for patients in the US-performed group who underwent surgery or sufficient clinical and radiologic follow-up of at least 1 year. We analyzed the diagnostic performance of US to detect malignancy as follows: sensitivity, specificity, positive predictive value (PPV) and negative predictive value (NPV), according to the 18F-FDG PET/CT findings.
All patients fasted for at least 6 hours prior to the 18F-FDG PET/CT examinations but were allowed to drink water. The 18F-FDG PET/CT scans were performed using a GE Discovery LS PET/CT scanner (GE Healthcare, Milwaukee, WI, USA). A whole-body CT scan was performed using a continuous spiral technique with an eight-slice helical CT that had a gantry rotation speed of 0.8 second. The acquisition protocol of the CT scan was as follows: 40-120 mAs adjusted by body weight, 140 kVp, a section slice width of 5 mm, and a table feed of 5 mm per rotation. Neither intravenous nor oral contrast agent was used. After the CT scan was obtained, PET imaging was obtained at 60 ± 5 minutes after intravenous injection of 370 MBq 18F-FDG. We reconstructed PET images using CT data for attenuation correction and image fusion and an ordered subset expectation maximization algorithm (28 subsets, two iterations) with Gaussian smoothing filter (full width at half maximum = 5.45 mm). The trans-axial images were scanned in a 128 × 128 matrix (pixel size = 4.29 × 4.29 mm) with a slice thickness of 4.25 mm. Commercial software (Xeleris, GE Healthcare, Milwaukee, WI, USA) was applied to exactly co-register the separate CT and PET scan data.
We divided 18F-FDG uptake into two patterns of focal: 18F-FDG uptake in less than a lobe of the thyroid gland or diffuse: 18F-FDG uptake in near or an entire thyroid gland. When we considered 18F-FDG uptake as abnormal on the visual analysis, we drew three-dimensional regions of interest to quantify the maximum standardized uptake value (SUVmax) normalized for body weight. ITLs were defined as an increase in 18F-FDG uptake on PET and/or an abnormal attenuated lesion on CT in any portion of the thyroid gland, regardless of a focal or diffuse pattern. A thyroid incidentaloma was defined as a focal lesion that revealed focal 18F-FDG uptake on PET or a nodule on CT. The 18F-FDG PET/CT findings were retrospectively classified into three categories of suspicious for malignant: unilateral/focal 18F-FDG uptake with SUVmax > 4.2; probably benign: bilateral/diffuse 18F-FDG uptake with SUVmax < 1.3 or no discernible thyroid nodule on CT; and undetermined: categorized into neither suspicious for malignant nor probably benign (6).
US examinations were performed using high-resolution US equipment (IU22; Philips Medical Systems, Bothell, WA, USA or HDI 5000; Advanced Technology Laboratories, Bothell, WA, USA) with 5-12 MHz linear array transducers by one of seven board-certified radiologists. US examinations included an evaluation of the whole thyroid gland and the lateral neck compartments (levels I, II, III, IV, or V). The US diagnosis was divided into "suspicious for malignant" and "probably benign". Suspicious for malignant US findings included taller-than-wide shape, infiltrative margin, microcalcifications, and marked hypoechogenicity (7). We diagnosed nodules as "suspicious for malignant" if there was one or more suspicious findings.
US-FNA was performed by radiologists. Using the freehand technique and direct US visualization, a 23-gauge needle tip was placed in the targeted lesion below the center of the transducer and was advanced to the lesion along the image plane. The aspirated material was placed on appropriately labeled glass slides, smeared, and fixed in 95% ethanol. The remainder of the material within the syringe was rinsed with ethanol for processing as a cell block. The slides were sent to the pathology department for analysis.
The statistical analysis was performed using SPSS software (SPSS Inc., Chicago, IL, USA). Patient age, sex, and staging of primary non-thyroid malignancy were analyzed by Pearson's chi-square test or the Wilcoxon rank-sum test, and 3 year mortality rates were analyzed by Pearson's chi-square test. The diagnostic performance of US was analyzed by McNemar's chi-square test. p values < 0.05 were considered significant. Numeric data are expressed as mean ± standard deviation.
The incidence of ITLs detected on 18F-FDG PET/CT examinations was 8.4% (226 of 2703 patients with non-thyroidal cancer) (Fig. 1). Among the 226 patients, 82 (36%) showed diffuse 18F-FDG uptake, and 144 (64%) had focal lesions with or without 18F-FDG uptake. The incidence of thyroid incidentaloma (focal lesion) on 18F-FDG PET/CT was 5.3% (144/2703).
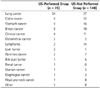
Of the 226 patients with ITLs, the US-performed group was composed of 78 (35%) and the US-not performed group was comprised of 148 (65%). The US-performed group included 27 males and 51 females (mean age, 59.9 ± 11.8 years; range, 33-82 years). The US-not performed group was 40 males and 108 females (mean age, 56.6 ± 11.6 years; range, 14-82 years). The age of patients in the US-performed group was significantly older than that in the US-not performed group (p = 0.037), but sex and stage of non-thyroidal malignancies were not significantly different between the two groups (Table 1). The 3-year mortality rate between US-performed group (26%, 20/78) and US-not performed group (32%, 47/148) was not significantly different (p = 0.421). Table 2 shows the origin of the primary non-thyroidal cancers with ITLs.
Of the 78 patients in the US-performed group, 57 had cytopathological results. Thirteen patients underwent total thyroidectomy for primary thyroid cancers, and the remaining 44 patients underwent US-FNA with clinical and radiologic follow-up. The final cytopathological results revealed malignant thyroid cancers (n = 22; papillary carcinoma: 20, medullary carcinoma: one, metastasis: one) and benign lesions (n = 35; nodular hyperplasia: 22, lymphocytic thyroiditis: four, cyst: two, others: seven). The malignant rate in the US-performed group that had cytopathology was 39% (22/57). All malignancies were primary thyroid cancers except for one metastasis arising from esophageal cancer. Of the 57 lesions with final cytopathological results, the SUVmax of malignant lesions (mean: 7.62 ± 5.22, range: 1.7-24) was significantly higher than that of benign lesions (mean: 4.05 ± 2.58, range: 1.0-12.9) (p = 0.001).
The diagnostic performance of subsequent US in all ITLs with cytopathological results revealed 86.4% (19/22) sensitivity, 71.4% (25/35) specificity, 65.5% (19/29) PPV, and 89.3% (25/28) NPV to detect malignancy (Table 3). Of probable benign lesions assessed by PET/CT (n = 9), US revealed 100% (9/9) specificity and 100% (9/9) NPV and had complete agreement with the final result. Four of nine lesions revealed diffuse and bilateral 18F-FDG uptake, and five lesions revealed focal low attenuated nodules without 18F-FDG uptake, which presented an SUVmax < 2.9 in all cases (Figs. 2, 3). Of the suspicious malignant lesions assessed by PET/CT (n = 22), US revealed 75% (9/12) sensitivity, 90% (9/10) specificity, 75% (9/12) PPV, and 90% (9/10) NPV. Of 22 patients, 21 revealed focal 18F-FDG uptake in unilateral lobes. The other patient, who had metastasis from esophageal cancer, revealed multifocal 18F-FDG uptakes in bilateral lobes. Mean SUVmax was 7.75 (range, 2.7-24). Of the undetermined lesions assessed by PET/CT (n = 26), US revealed 100% (10/10) sensitivity, 94% (15/16) specificity, 91% (10/11) PPV, and 100% (15/15) NPV, corresponding to excellent agreement with the final results (kappa value = 0.92).
The incidence of ITLs detected on 18F-FDG PET/CT for patients with non-thyroid cancer was 8.4%, which was similar to the 9% reported in a previous study that investigated both focal and diffuse 18F-FDG uptake lesions in thyroid gland (3). The incidence of thyroid incidentalomas (focal lesions) was 5.3% in our study, which was slightly higher than the 1.2-4.3% in other reports in both patients with malignancies and healthy subjects (8, 9, 10, 11). It seemed that this difference resulted from the population in the present study, which included only patients with nonthyroidal malignancies, and previous studies. The prevalence of thyroid incidentalomas detected on 18F-FDG PET/CT in patients with suspected or known cancer (4.1%) was higher than that in healthy subjects (2.6%) (6). Rheingold et al. (12) suggested that a history of malignancy could be one of the major risk factors for developing another kind of malignancy. The reason that the incidence of thyroid incidentalomas in the present study was relatively higher was due to the population of only patients with primary malignancies, compared to including healthy subjects.
In the present study, the incidence of malignant ITLs detected on 18F-FDG PET/CT was 22 (39%) of 57 patients who had final cytopathology. Other investigations revealed that it ranges from 27% to 72% (4, 6, 9, 11, 13, 14, 15). Most of the 22 patients with malignancies had primary thyroid carcinomas (20 papillary carcinomas and one medullary carcinoma), but the other one had metastasis arising from esophageal cancer. Most malignant nodules detected on 18F-FDG PET/CT were well-differentiated papillary carcinomas, as reported by Deandreis et al. (5) and Pagano et al. (16). Our study had no discrepancies to previously reported studies, although the healthy population was excluded in the present study.
Most researchers evaluate focal or diffuse uptake, unilateral or bilateral uptake, and the SUVmax value to distinguish malignant from benign disease for ITLs on 18F-FDG PET/CT (4, 11, 13, 16). ITLs detected by PET/CT had diffuse or focal 18F-FDG uptake patterns. The diffuse uptake pattern is more frequently benign disease, such as thyroiditis, nodular goiter, or Grave's disease (16). Focal uptake of thyroid incidentalomas is clinically more significant due to its high risk of malignancy, including primary thyroid cancer and metastasis (6, 9, 14, 15). The risk of malignancy was extremely low (1.4%) in patients with diffuse or bilateral uptake on PET scans, while focal or unilateral uptake revealed a higher risk (15%) of malignancy (11). In the present study, 21 primary thyroid cancers of 22 ITLs proven to be malignant had focal uptake (unilateral uptake in 18 patients and bilateral in three patients). The other of the 22 lesions was a metastasis arising from esophageal cancer, which presented as diffuse and bilateral uptake in the thyroid gland, although US suggested bilateral aggressive masses. Because all primary thyroid cancers revealed focal uptake, we excluded primary thyroid cancers from incidental thyroid lesions with diffuse and bilateral uptake. However, diffuse and bilateral uptake should be handled vigilantly in patients with non-thyroid cancer because this finding can indicate metastasis.
Because the mean SUVmax value of malignant lesions was higher than that of benign lesions in the current study, we purport that the SUVmax value can help distinguish malignant lesions from benign. Cohen et al. (9) reported that the average SUVmax in malignant lesions (6.92 ± 1.54) was higher than that in benign lesions (3.37 ± 0.21). In another study, the diagnostic accuracy of SUVmax using a 4.2 cut-off value was 69.5%, without adding other imaging findings (3). In contrast, the SUVmax between benign and malignant thyroid nodules was not significantly different in one study, although the average SUVmax of the malignant thyroid lesions was higher than that of benign thyroid lesions (4).
The American Thyroid Association guidelines recommend that diagnostic thyroid US should be performed for thyroid incidentalomas detected on 18F-FDG PET/CT (17). According to the recommendations with consensus among the American Association of Clinical Endocrinologists, Associazione Medici Endocrinologi, and the European Thyroid Association Medical guidelines, a US evaluation should be conducted because of uncertain risk of malignancy of thyroid incidentaloma (18). However, subsequent US had no additional diagnostic value for ITLs with probable benign findings on 18F-FDG PET/CT in our study.
Of 26 patients with undetermined findings on 18F-FDG PET/CT, the diagnostic performance of US showed excellent agreement with the final cytopathological results. The probability (13.2%) of malignancy was much lower than when the US findings appeared benign, as compared with significantly higher probability (75.5%) of malignance when the US findings were suspicious for malignant (4). Therefore, subsequent US can provide additional diagnostic value when ITLs have undetermined findings on 18F-FDG PET/CT.
There are several limitations in this study. First, this study had selection bias to evaluate diagnostic performances of 18F-FDG PET/CT and US because only patients who underwent US-FNA or surgery were included. Second, the 3-year survival rate between US-performed and US-not performed groups may not have been sufficient to evaluate long-term mortality rates of the patients. Third, we could not define criteria for subsequent US indications in this study because the 18F-FDG PET/CT and the US results were retrospectively analyzed. Large prospective studies will need to solve the limitations of the present study.
In conclusion, ITLs detected on 18F-FDG PET/CT did not affect patient prognosis whether US was performed or not. Because subsequent US has no additional diagnostic value in ITLs with probable benign findings on 18F-FDG PET/CT, it may be unnecessary for ITLs with benign findings on PET/CT.
Figures and Tables
Fig. 1
Flow chart of the participants in the study.
Note.-F/U = follow-up, LT = lymphocytic thyroiditis, MTC = medullary thyroid carcinoma, NH = nodular hyperplasia, PET/CT = positron emission tomography/computed tomography, PTC = papillary thyroid carcinoma, US-FNAB = ultrasound-guided fine needle aspiration, 18F-FDG = 18F-fluorodeoxyglucose

Fig. 2
A 59-year-old female with sarcoma in the right pulmonary artery. The 18F-FDG PET/CT reveals a 2 cm low-attenuated nodule (arrowhead) with no uptake in the left lower thyroid lobe (A). Ultrasonograms show a smooth solid and cystic nodule (arrows) in the inferior pole of the left thyroid gland, which was diagnosed as a probably benign nodule (B: axial scan, C: longitudinal scan). Nodular hyperplasia was confirmed by US-guided fine needle aspiration.
Note.-PET/CT = positron emission tomography/computed tomography, US = ultrasound, 18F-FDG = 18F-fluorodeoxyglucose

Fig. 3
A 47-year-old female with lung cancer. The 18F-FDG PET/CT reveals a 1 cm low-attenuated nodule (arrowhead) with mild uptake (SUV: 4.1) in the right thyroid lobe, which was diagnosed as a undetermined lesion (A). A 0.7 cm irregular hypoechoic nodule (arrow) with several microcalcifications is demonstrated on ultrasound, which was considered suspicion for malignancy (B: axial scan, C: oblique scan). Papillary thyroid carcinoma was confirmed by total thyroidectomy.
Note.-PET/CT = positron emission tomography/computed tomography, SUV = standardized uptake value, 18F-FDG = 18F-fluorodeoxyglucose

Table 1
Comparison of Clinical Characteristics of the Patients with Abnormal Thyroid Lesions on PET/CT between US-Performed Group and US-Not Performed Group

References
1. Shetty SK, Maher MM, Hahn PF, Halpern EF, Aquino SL. Significance of incidental thyroid lesions detected on CT: correlation among CT, sonography, and pathology. AJR Am J Roentgenol. 2006; 187:1349–1356.
2. Bae JS, Chae BJ, Park WC, Kim JS, Kim SH, Jung SS, et al. Incidental thyroid lesions detected by FDG-PET/CT: prevalence and risk of thyroid cancer. World J Surg Oncol. 2009; 7:63.
3. Kang BJ, O JH, Baik JH, Jung SL, Park YH, Chung SK. Incidental thyroid uptake on F-18 FDG PET/CT: correlation with ultrasonography and pathology. Ann Nucl Med. 2009; 23:729–737.
4. Kwak JY, Kim EK, Yun M, Cho A, Kim MJ, Son EJ, et al. Thyroid incidentalomas identified by 18F-FDG PET: sonographic correlation. AJR Am J Roentgenol. 2008; 191:598–603.
5. Deandreis D, Al Ghuzlan A, Auperin A, Vielh P, Caillou B, Chami L, et al. Is (18)F-fluorodeoxyglucose-PET/CT useful for the presurgical characterization of thyroid nodules with indeterminate fine needle aspiration cytology? Thyroid. 2012; 22:165–172.
6. Choi JY, Lee KS, Kim HJ, Shim YM, Kwon OJ, Park K, et al. Focal thyroid lesions incidentally identified by integrated 18F-FDG PET/CT: clinical significance and improved characterization. J Nucl Med. 2006; 47:609–615.
7. Moon WJ, Baek JH, Jung SL, Kim DW, Kim EK, Kim JY, et al. Ultrasonography and the ultrasound-based management of thyroid nodules: consensus statement and recommendations. Korean J Radiol. 2011; 12:1–14.
8. Chen YK, Ding HJ, Chen KT, Chen YL, Liao AC, Shen YY, et al. Prevalence and risk of cancer of focal thyroid incidentaloma identified by 18F-fluorodeoxyglucose positron emission tomography for cancer screening in healthy subjects. Anticancer Res. 2005; 25:1421–1426.
9. Cohen MS, Arslan N, Dehdashti F, Doherty GM, Lairmore TC, Brunt LM, et al. Risk of malignancy in thyroid incidentalomas identified by fluorodeoxyglucose-positron emission tomography. Surgery. 2001; 130:941–946.
10. Kim SJ, Kim BH, Jeon YK, Kim SS, Kim IJ. Limited diagnostic and predictive values of dual-time-point 18F FDG PET/CT for differentiation of incidentally detected thyroid nodules. Ann Nucl Med. 2011; 25:347–353.
11. Are C, Hsu JF, Schoder H, Shah JP, Larson SM, Shaha AR. FDG-PET detected thyroid incidentalomas: need for further investigation? Ann Surg Oncol. 2007; 14:239–247.
12. Rheingold SR, Neugut AI, Meadows AT. Secondary cancers: incidence, risk factors, and management. In : Kufe DW, Holland JF, Frei E, editors. Cancer medicine. 6th ed. Hamilton, ON: BC Decker;2003. p. 2623.
13. de Geus-Oei LF, Pieters GF, Bonenkamp JJ, Mudde AH, Bleeker-Rovers CP, Corstens FH, et al. 18F-FDG PET reduces unnecessary hemithyroidectomies for thyroid nodules with inconclusive cytologic results. J Nucl Med. 2006; 47:770–775.
14. Kang KW, Kim SK, Kang HS, Lee ES, Sim JS, Lee IG, et al. Prevalence and risk of cancer of focal thyroid incidentaloma identified by 18F-fluorodeoxyglucose positron emission tomography for metastasis evaluation and cancer screening in healthy subjects. J Clin Endocrinol Metab. 2003; 88:4100–4104.
15. Kim TY, Kim WB, Ryu JS, Gong G, Hong SJ, Shong YK. 18F-fluorodeoxyglucose uptake in thyroid from positron emission tomogram (PET) for evaluation in cancer patients: high prevalence of malignancy in thyroid PET incidentaloma. Laryngoscope. 2005; 115:1074–1078.
16. Pagano L, Samà MT, Morani F, Prodam F, Rudoni M, Boldorini R, et al. Thyroid incidentaloma identified by 18F-fluorodeoxyglucose positron emission tomography with CT (FDG-PET/CT): clinical and pathological relevance. Clin Endocrinol (Oxf). 2011; 75:528–534.
17. American Thyroid Association (ATA) Guidelines Taskforce on Thyroid Nodules and Differentiated Thyroid Cancer. Cooper DS, Doherty GM, Haugen BR, Kloos RT, Lee SL, et al. Revised American Thyroid Association management guidelines for patients with thyroid nodules and differentiated thyroid cancer. Thyroid. 2009; 19:1167–1214.
18. Gharib H, Papini E, Paschke R, Duick DS, Valcavi R, Hegedüs L, et al. American Association of Clinical Endocrinologists, Associazione Medici Endocrinologi, and EuropeanThyroid Association Medical Guidelines for Clinical Practice for the Diagnosis and Management of Thyroid Nodules. Endocr Pract. 2010; 16:Suppl 1. 1–43.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download