Abstract
Blunt injury to the carotid artery is rare but may produce a devastating outcome. Dissection of the internal carotid artery is the most frequent cause of trauma related cerebral infarction, whereas post-traumatic middle cerebral artery dissection (MCAD) has rarely been encountered clinically. We report a case of cerebral infarction who suggested post-traumatic MCAD. The patho-physiology, clinical presentation, and treatment options of trauma induced MCAD are discussed.
The development of hemiparesis and other focal cerebral signs in patients with head trauma often suggests intracranial hemorrhages or cerebral contusions. However, these signs are occasionally related to traumatic occlusion of the carotid and cerebral arteries.2) Arterial dissection is one form of traumatic vascular injury and usually followed by intramural bleeding with the formation of a hematoma in the dissected space.5,9) In clinical practice, middle cerebral artery dissection (MCAD) is an extremely rare clinical entity. Etiologies, clinical manifestations, natural history and prognosis of MCAD remain poorly understood.5) In this report, we describe a case of suggestive MCAD after an assault who present cerebral infarction.
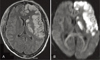
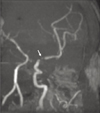
A drunken 49-year-old man was admitted via an emergency department because of mental change. His family stated that the patient had been attacked by an unknown man. On presentation to the emergency department, he was confused and lethargic. General examination revealed bruising and swelling on the nose. The patient's neck, pulmonary, cardiac, abdominal, and back examination were unremarkable. Initial brain CT and biochemical evaluation was normal except nasal bone fracture (Figure 1). 5 hours after presentation, he was noted to have right side hemiparesis that ability to move against gravity only. Follow-up head CT revealed hypo attenuated lesions in the right basal ganglia area (Figure 2). Brain MRI and MRA performed at the second day of admission. MRI of brain showed that recent multiple infarctions over the left caudate nucleus, internal capsule and fronto-parietal lobe (Figure 3). MRA of the intracranial arteries revealed that severe segmental narrowing of the proximal left M1 segment. This finding was assumed to be a dissection process left middle cerebral artery (Figure 4). The patient was received conservative care with acetile salicilic acid. After two weeks of follow-up, the neurological deficiencies were partially improved. After a three-month treatment, the patient underwent regular follow-up in the outpatient department. The patient maintained intact awareness but remained a rightside hemiparetic state.
The pathogenesis of posttraumatic occlusions of the cerebral artery can be divided into four types of lesions: emboli from the cervical portion of the carotid artery, vasospasm, traumatic dissection, and posttraumatic thrombosis.4) Traumatic dissection is the major cause of posttraumatic occlusions of the cerebral artery.2) Cerebral vasospasm after blunt head trauma is an important secondary posttraumatic insult and frequently occurs a few days after the initial injury.2,4,8)
Traumatic internal carotid artery dissection (TICAD) is common cause of cerebral ischemic stroke in young adults, accounting for approximately 20%.12) Risk factors for TICAD include vigorous physical exercise, blunt head and neck trauma, penetrating neck injury and skull-base fracture.12)
Post-traumatic MCAD has rarely been encountered clinically. The exact mechanism of blunt head injury cause dissection of MCA is not clear.2,5) Some authors have suggested that the impact of the MCA, particular to the M1 segment against the sphenoid ridge causes a force that stretches the internal elastic lamina beyond the limit of its extensibility causes the rupture, which resulted in a post-traumatic dissection.2,5,9)
Typical angiographic findings of MCAD that are similar to those observed with TICAD may demonstrate an irregular stenosis, an intimal flap, double lumen sign, or the combination of adjacent stenosis and dilatation, pseudoaneurysm and even total occlusion.3,5,7) However, angiographic demonstration of an intimal flap, false lumen, or pseudoaneurysm is relatively uncommon. Segmental stenosis of the involved vessel segment is the most common angiographic finding as our case.5)
With the increasing use of noninvasive diagnostic methods, clinical recognition of ICA dissection is increasing.1,11) Almi et al1) reported 1095 patients admitted to an intensive care unit after closed head trauma showed an incidence of bilateral carotid artery dissection of 0.73%.
There was still no consensus for the treatment of TICAD or MCAD because controlled studies are lacking.3,5) Current therapeutic options include observation, anticoagulants, antiplatelet agents, and surgery.3,6,11) Generally, first-line therapy for TICAD has routinely consisted of anticoagulation therapy.11) But, Piepgras et al.10) speculated that anticoagulation maybe harmful in these patients for fear of hemorrhagic transformation or even dissection process progression.
MCAD lesion can follow minimal head trauma, which should be suspected in patients with delayed neurologic symptoms in the absence of intracranial hemorrhage. Injured and sedated patients without abnormalities on initial CT scan might benefit from frequent neurological re-examination. Further study needs to be determined the optimal treatment in traumatic MCAD patients also.
Figures and Tables
References
1. Alimi Y, Di Mauro P, Tomachot L, Albanese J, Martin C, Alliez B, et al. Bilateral dissection of the internal carotid artery at the base of the skull due to blunt trauma: incidence and severity. Ann Vasc Surg. 1998; 12:557–565.

2. Bunai Y, Nagai A, Nakamura I, Akaza K, Ohya I. Posttraumatic thrombosis of the middle cerebral artery. Am J Forensic Med Pathol. 2001; 22:299–302.

3. de Borst GJ, Slieker MG, Monteiro LM, Moll FL, Braun KP. Bilateral traumatic carotid artery dissection in a child. Pediatr Neurol. 2006; 34:408–411.

4. Hollin SA, Sukoff MH, Silverstein A, Gross SW. Post-traumatic middle cerebral artery occlusion. J Neurosurg. 1966; 25:526–535.

5. Lin CH, Jeng JS, Yip PK. Middle cerebral artery dissections: differences between isolated and extended dissections of internal carotid artery. J Neurol Sci. 2005; 235:37–44.

6. Lin JJ, Chou ML, Lin KL, Wong MC, Wang HS. Cerebral infarct secondary to traumatic carotid artery dissection. Pediatr Emerg Care. 2007; 23:166–168.

7. Liu WP, Ng KC, Hung JJ. Carotid artery injury with cerebral infarction following head and neck blunt trauma: report of a case. Yale J Biol Med. 2005; 78:151–156.
8. Martin NA, Doberstein C, Zane C, Caron MJ, Thomas K, Becker DP. Posttraumatic cerebral arterial spasm: transcranial Doppler ultrasound, cerebral blood flow, and angiographic findings. J Neurosurg. 1992; 77:575–583.

9. Mobbs RJ, Chandran KN. Traumatic middle cerebral artery occlusion: case report and review of pathogenesis. Neurol India. 2001; 49:158–161.
10. Piepgras DG, McGrail KM, Tazelaar HD. Intracranial dissection of the distal middle cerebral artery as an uncommon cause of distal cerebral artery aneurysm. Case report. J Neurosurg. 1994; 80:909–913.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download