Abstract
Purpose
The purpose of this study was to retrospectively evaluate the short-term clinical and radiological outcomes of total hip arthroplasty (THA) with short metaphyseal loading femoral stem.
Materials and Methods
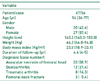
We retrospectively reviewed the records of 56 cases in 47 patients who had undergone THA with short metaphyseal loading femoral stem from April 2010 to December 2011. There were 20 males and 27 females. The mean age was 54 years (range, 26-77 years). The average follow up period was 4.6 years. Clinical results were evaluated by Harris hip scores (HHS) before the operation and at the last follow-up. Radiographic analysis was done by evaluating osteolysis, loosening, stress shielding, and alignement.
Results
The mean HHS significantly improved from 45 (range, 15-58) preoperatively to 98 (range, 85-100) at the last follow-up. In radiographic analyses, there was no evidence of osteolysis or loosening around the stems and the acetabuluar components. All cases showed rounding off of the calcar, grade 1 bone resorption of the proximal femur. With regard to implant alignment, 51 femoral component (91.1%) were in neutral position, and 5 (8.9%) were in varus position. There was 1 intraoperative fracture treated by cerclage wiring and no case was revised during follow-up period.
Successful long term results after total hip arthroplasty (THA) has led to a steady increase in primary THA in the past three decades1). With the increase of primary THA, a steady increase of revisional THA has also occurred because of limited long-term survival of primary THA2). The surgeon should always give consideration to the future revisional THA in their surgical planning, especially for those young and active patients. Many attempts had been made to improve and ease revisional THA3). Under this circumstance, short femoral stems have been designed to preserve metaphyseal cancellous bone stock by a more proximal fixation and leaves more bone stock for any subsequent revision4).
The first concept of the short stem was designed by Judet and Judet5) from 1940s. The long term results of the primary short stem on the base of the concept were not satisfactory6) because the implants might get the small anchoring surface area in the metaphysis without fixation at the greater trochanter7). Later model, the Mayo Conservative Hip (Zimmer, Warsaw, IN, USA) was designed to anchor the lateral proximal diaphysis to get the larger fixation area3). The implant has been in clinical use for over 20 years now and shows a 94% survival rate after 6.2 years78).
The Proxima™ stem (DePuy Synthes, Warsaw, IN, USA) is made of forged titanium alloy, with a Duofix™ HA (porous coating and hydroxyapatite; DePuy Synthes) surface coating. A lateral trochanteric flare was used in this prosthesis to load the corresponding area in the lower region of the greater trochanter, which assist in transmitting and an anatomic fit in the metaphysis with longitudinal slots for rotational stability9). Although the results of THA with a Proxima™ stem were promising410), there are only a few reports on the results of THA with a Proxima™ stem. The purpose of this study was retrospectively to evaluate the clinical and radiological results of the patients who underwent primary cementless THA using a Proxima™ stem. We hypothesized that the primary cementless THA using short metaphyseal loading femoral stem would yield satisfactory clinical and radiological outcomes without serious complications.
The ethics committee of Yonsei Sarang institution approved this protocol for the human procedures used in this study (YS) (16-D2-01).
From April 2010 to December 2011, 65 consecutive primary cementless THAs using a Proxima™ stem were performed by the single surgeon (YWC). The indication of short metaphyseal loading femoral stem included the patients who had achieved rigid fixation, regardless of the age. Any type of bone stock was acceptable if there was normal femoral morphology. Congenital hip dysplasia as well as acquired deformity of the proximal femur represented contraindications. Nine hips were not included because of follow-up loss or incomplete radiographic records. Consequently, 56 cases in 47 patients were included in this study and reviewed retrospectively. The detailed demographics of the patients were in Table 1.
A cementless Pinnacle™ acetabular component (DePuy Synthes) was used in all hips. These components were press fitted after the acetabulum had been underreamed by 1 mm. The cup sizes used ranged from 52 to 58 mm, and 36-mm Biolox delta™ liner (CeramTec, Plochingen, Germany) was used in all hips. All patients received a Proxima™ femoral component with a 36-mm Biolox delta™ ceramic head. The femoral neck was cut horizontally at a head-neck juncture to make a wider entrance for the stem. A "round-the-corner" technique was used for femoral broaching and implant insertion as described by Santori et al11). The round-the-corner technique is different from conventional surgical techniques and used to large trochanteric flare. At first, the broach must be inserted and hammered down in a 30° varus position until it is flush with the internal shoulder of the greater trochanter (Fig. 1). The broach is then gradually tilted in while progressing down the femoral metaphysis. When this movement is completed, alignment is checked using a dedicated guide. A torsional movement is applied on the broach in order to check rotational stability. The size of the femoral component selected matched the size of the largest broach used. The dimension of the coated component was 0.5 mm larger than that of the prepared metaphysis. The range of motion was checked in the operation field and the wound was closed with a suction drain.
Patients were allowed to stand on the second postoperative day. Partial weight bearing using crutches was recommended for 4 weeks postoperatively, thereafter full weight bearing with canes was allowed for two additional weeks. All patients were requested to visit at the hospital at 6 weeks, 3, 6, and 12 months postoperatively and yearly thereafter. Clinical and radiographic assessments were done at each visit. Clinical assessment was done using Harris hip score12). Thigh pain was evaluated as visual analogue scale (VAS).
Standardized radiographs including anteroposterior and lateral hip radiographs were obtained at each follow-up. The radiologic evaluation was performed by comparing of the radiographs taken one day after operation with the last follow-up. Each acetabular component was evaluated for the presence and progression of radiolucent lines and osteolysis at the bone-implant interface by dividing acetabulum into Zone I, II, and III according to DeLee and Charnley13). A continuous radiolucent line above 2 mm in width at the bone-implant interface was accepted as radiographic evidence of impending failure according to the criteria of Dorr et al14). Acetabular migration was considered as movement >2 mm in the horizontal or vertical directions and change of inclination angle >5°15). Acetabular cup loosening was defined if migration could be demonstrated. Osteolysis was defined as a localized or cystic-like scalloped radiolucent lesion adjacent to the prostheses, if it was detected on follow-up radiographs but not observed in the immediate postoperative radiographs16).
The femoral morphology was determined in preoperative radiographs using Dorr's classification system17). The stem position in the anteroposterior plane was determined by deviation of the axis of the stem which was drawn at 130° angle with the axis of the stem neck from the axis of the femoral shaft because the neck-shaft angle of the stem is 130°10) (Fig. 2). Stem alignment was rated as normal if its deviation from the axis of the femoral shaft was 5° or less. A deviation of 6° to 10° was rated as "varus" or "valgus"; a deviation exceeding 10° was rated as "severe varus" or "severe valgus"18). The presence of radiolucent lines and osteolytic lesions around the femoral component (Gruen zones19) 1 and 7) was analyzed as well. Given the lack of distal stem in the short femoral components, region from the lower border of the lesser trochanter to the tip of the greater trochanter was defined as zone 1, and the region from the lower border of the lesser trochanter to femoral neck cut level was defined as zone 7 according to Kim et al10). Loosening of the femoral component was defined when there was a progressive axial subsidence of greater than 2 mm or a varus or valgus shift of greater than 2°20). Stem subsidence was evaluated by measuring the distance between the tip of the greater trochanter and the lateral flare of the stem as well as by measuring the distance between the most proximomedial part of the porous-coated surface of the stem and the upper border of the lesser trochanter10). Proximal femoral bone resorption was graded radiologically, with grade 1 indicating atrophy or rounding off of the calcar; grade 2, loss of density in the calcar region with preservation of the medial cortical wall to the level of the lesser trochanter; grade 3, loss of density in the calcar region with loss of the medial cortical wall to the level of the lesser trochanter; and grade 4, loss of bone density in the entire medial cortical wall distal to the level of the lesser trochanter21). Heterotopic ossification, if present, was graded according to the classification system of Brooker et al.22). Any intraoperative or postoperative complications were recorded. We defined the failure of the stem as the hip requires revision for any reasons. All statistical analyses were performed using PASW Statistics version 18.0 (IBM Co., Armonk, NY, USA), and paired t-tests were conducted for comparing the mean HHS preoperatively and at the last follow-up. P-values <0.05 were considered statistically significant. The survival analysis was performed by the Kaplan-Meier method.
The mean HHS was significantly improved from 45±9.0 (range, 15-58) preoperatively to 98±2.9 (range, 85-100) at the final follow-up (P<0.01). No patient had thigh pain during any follow-up period. No hip had a continuous radiolucent line above 2 mm in width at the bone-implant interface around the acetabular cup. There was no osteolysis around the acetular component and no migration of acetabular cups in the patients at final follow-up. The morphology of the proximal femur was Dorr type A in 54 (96.4%) of 56 hips and type B in 2 hips (3.6%). In the anteroposterior plane, 51 femoral components (91.1%) were in neutral position, and 5 (8.9%) were in varus position (Fig. 3). There was no femoral component had a deviation exceeding 10°. No hip had a radiolucent line around the porous-coated surface of the femoral component on either anteroposterior or lateral radiographs. There was no osteolysis around the femoral component. No hip had a progressive axial subsidence of the femoral component in excess of 2 mm or a varus or valgus shift of greater than 2°. At the latest evaluation, all hip showed only rounding off of the calcar, as grade 1 of proximal femoral bone resorption. No patient had heterotopic ossification. Four patients (7.1%) had a mild limp and 1 patient (1.8%) had a moderate limp. No hip had clicking sound or squeaking sound. One intraoperative fracture was treated by cerclage wiring and delayed weight bearing (Fig. 4). There was no other complication such as any infection, deep vein thrombosis or pulmonary embolism. There was no dislocation, ceramic crack, or periprosthetic fracture in all hips.
No revision was done to the acetabular cup or the femoral component during the follow-up periods. Therefore, the Kaplan-Meier method showed the survival rate of the acetabular cup and the femoral components is 100%.
The short femoral implants can be broadly categorized into three categories: the femoral neck implants, the stem engaging the lateral cortex, and the stem utilizing the lateral trochanteric flare9). The femoral neck implant is usually used for hip resurfacing. The Birmingham Mid Head Resection™ (Smith & Nephew Ltd., Warwick, UK) is a typical example23). The second type of stem engages the lateral cortex and the femoral neck prosthesis CTU™ (ESKA Implants, Lübeck, Germany) is a typical example24). The third stem is to use a large lateral flare to fix in the proximal metaphysis and the stem used in this study belongs to this type of stem. The rationale of this stem is supported by Walker et al.25) who suggested that the addition of a lateral flare to a cementless stem allows load transmission to the lower region of the greater trochanter and prevents axial migration, and allowed the design to limit stem length.
In this recent study, the clinical and radiological results of THA using a Proxima™ stem were satisfying during the mean follow-up of 4.6 years. The mean HHS was significantly improved from 45 preoperatively to 98 at the last follow-up. All patients in this study had no thigh pain and just proximal femoral bone resorption as grade 1 or none during the follow-up. This result is comparable with other studies using conventional cementless femoral stem2627) and is similar to other studies which reported on the results of THA using a Proxima™ stem410). Ghera and Pavan18) reviewed the clinical and radiological results of 65 hips underwent THA using the same stem used in this study with the mean follow-up of 1.7 years. The authors reported HHS was improved from 51 preoperatively to 91 at the last follow-up and there was no thigh pain in any patients. They revealed stress shielding of grade 1 in 49 cases and grade 2 in 16 regrading to proximal femoral bone resorption on radiographic analysis. No signs of periprosthetic osteolysis were detected in the study. Kim et al.10) reported similar results of 144 hips who underwent THA using the same stem with a mean follow-up of 4.5 years. The authors reported no discernible sites of resorption or only slight rounding off of osteomized neck. Those finding suggest optimal load transmission to the proximal metaphysis and good mechanical stability of the stem at early the follow-up. The pattern of proximal bone remodeling also reflects the reproduction of a physiological transmission of loads, compressive as well as torsional. Theoretically, the patients who underwent THA with short stems should tend to have less proximal femoral bone resorption and thigh pain because the rationale of short stem is to give load transfer to the proximal metaphysis and avoid distal fixation. Kim et al.10) reported bone marrow density around the same stem used in this study was slightly lower than the baseline value but preserved than around acetabular component. Their finding suggested a lower level of bending stiffness and allowing a physiologic load transfer in the short stem was accomplished.
Whether stable fixation of the short stem can be confirmed without diaphyseal fixation is one of the concerns related to short stem. In a biomechanical study by Westphal et al.28), the proximal-fitting short metaphyseal stem could achieve adequate stem stability when cortical contact was achieved or when the bone quality was good. Santori et al.29) reported significant initial stability of their custom-made short femoral stem similar to the proximal-fitting short metaphyseal stem in the clinical report. Their study validated the assumption that torsional loads can be controlled without the diaphyseal portion of the stem and that neck preservation combined with lateral flare support. In our case series, stable fixation was observed in all cases on the last radiographs.
Kim et al.10) proposed the proximal-fitting short metaphyseal stem could be used for the patients with a deformed femur or an obliterated femoral canal, which would make conventional THA difficult, in the clinical study used the same stem to this study. In our study, 17 of all patients (36.2%) were over 60 years old without Dorr type C morphology of the proximal femur. Those patients over the age of 60 years showed good stability of the short stem without osteolysis around the stem. Usage of the proximal-fitting short metaphyseal stem should be allowed for the older patients if they have good bone quality or morphology of the femur.
The varus position of the stem was observed in 5 of 56 cases (8.9%) but the angle of varus was less than 10° in all cases. Toth et al.4) reported that the position of neutral, varus and severe varus were observed in 31 (75.6%), 8 (19.5%), and 2 (4.9%) of 41 cases at mean 1.7 year follow-up, respectively when they defined a >5° deviation as varus or valgus and a >5° deviation as severe varus or severe valgus in the clinical report used the same stem of this study. Kim et al.10) evaluated the result after THA using the same stem. They reported neutral and varus position were 136 (94.4%) and 8 (5.6%) of 144 hips, respectively, when they defined neural position within 3° deviation. These results were not different as compared with conventional THA26). The main factors of the varus position are the improper entry hole position and inadequate hit force during the round-the-corner broaching. A correct entry hole gives more chance to allow the stem in the center of the medullary canal. To make a correct entry is easier in old patients because the bone is weaker than young patients. Therefore, more attention is needed to make a entry hole in the young patients. Femoral morphology may also affect the implant alignment because the greater trochanter is more medially or laterally positioned in some patients. In the former case, the entry hole should be more lateral because the femoral diaphyseal axis crosses the lateral position of femoral neck base. In the latter case, the entry hole should be more medial. If the round-the-corner movement of the broach is not properly accomplished, the axis of the stem will be malaligned. Until the surgeon has proper experience, the use of fluoroscopy is advisable.
There are some limitations in this study. First, it was a non-comparative and retrospective design. Second, the relatively short-term follow-up period (4.5 years) is noted. We believe that a long-term follow-up period of 10 years or longer is necessary for the assessment of THA using the short stem. However, this study can be considered to be of significance, because some study reported cementless femoral stem produced good late clinical result if there were no stability problem in less than 2 years30). The stable femoral stem at 4.6 year after the operation can maintain the long-term stable fixation of the femoral component.
In summary, the clinical and radiological results of this study were comparable with the other studies using conventional cementless femoral stem. The short metaphyseal loading femoral stem could be used for the patient over the age of 60 years if they have good bone quality or morphology of the femur.
Figures and Tables
Fig. 1
The round-the-corner broaching technique. The broach is first inserted in about 20° to 30° varus position to avoid damaging the greater trochanter and the abductor muscles if a conventional technique is used. Then, the broach is straightened while progressing down.

Fig. 2
The stem position in the anteroposterior plane was determined by deviation of the axis of the stem (white dotted line) which was drawn at 130° angle with the axis of the stem neck from the axis of the femoral shaft (white solid line) because the neck-shaft angle of the stem is 130°.

Fig. 3
Anteroposterior radiographs showed the neutral position (A) and the varus position of the stem (B).

References
1. Kurtz S, Mowat F, Ong K, Chan N, Lau E, Halpern M. Prevalence of primary and revision total hip and knee arthroplasty in the United States from 1990 through 2002. J Bone Joint Surg Am. 2005; 87:1487–1497.

2. Ulrich SD, Seyler TM, Bennett D, et al. Total hip arthroplasties: what are the reasons for revision? Int Orthop. 2008; 32:597–604.

3. Morrey BF. Short-stemmed uncemented femoral component for primary hip arthroplasty. Clin Orthop Relat Res. 1989; (249):169–175.

4. Tóth K, Mécs L, Kellermann P. Early experience with the Depuy Proxima short stem in total hip arthroplasty. Acta Orthop Belg. 2010; 76:613–618.
5. Judet J, Judet R. The use of an artificial femoral head for arthroplasty of the hip joint. J Bone Joint Surg Br. 1950; 32-B:166–173.

6. Fink B, Wessel S, Deuretzbacher G, Protzen M, Ruther W. Midterm results of "thrust plate" prosthesis. J Arthroplasty. 2007; 22:703–710.

7. Fottner A, Schmid M, Birkenmaier C, Mazoochian F, Plitz W, Volkmar J. Biomechanical evaluation of two types of short-stemmed hip prostheses compared to the trust plate prosthesis by three-dimensional measurement of micromotions. Clin Biomech (Bristol, Avon). 2009; 24:429–434.

8. Morrey BF, Adams RA, Kessler M. A conservative femoral replacement for total hip arthroplasty. A prospective study. J Bone Joint Surg Br. 2000; 82:952–958.
10. Kim YH, Kim JS, Joo JH, Park JW. A prospective short-term outcome study of a short metaphyseal fitting total hip arthroplasty. J Arthroplasty. 2012; 27:88–94.

11. Santori N, Lucidi M, Santori FS. Proximal load transfer with a stemless uncemented femoral implant. J Orthop Traumatol. 2006; 7:154–160.

12. Harris WH. Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty. An end-result study using a new method of result evaluation. J Bone Joint Surg Am. 1969; 51:737–755.

13. DeLee JG, Charnley J. Radiological demarcation of cemented sockets in total hip replacement. Clin Orthop Relat Res. 1976; (121):20–32.

14. Dorr LD, Absatz M, Gruen TA, Saberi MT, Doerzbacher JF. Anatomic Porous Replacement hip arthroplasty: first 100 consecutive cases. Semin Arthroplasty. 1990; 1:77–86.
15. Martell JM, Pierson RH 3rd, Jacobs JJ, Rosenberg AG, Maley M, Galante JO. Primary total hip reconstruction with a titanium fiber-coated prosthesis inserted without cement. J Bone Joint Surg Am. 1993; 75:554–571.

16. Tanzer M, Maloney WJ, Jasty M, Harris WH. The progression of femoral cortical osteolysis in association with total hip arthroplasty without cement. J Bone Joint Surg Am. 1992; 74:404–410.

17. Dorr LD, Faugere MC, Mackel AM, Gruen TA, Bognar B, Malluche HH. Structural and cellular assessment of bone quality of proximal femur. Bone. 1993; 14:231–242.

18. Ghera S, Pavan L. The DePuy Proxima hip: a short stem for total hip arthroplasty. Early experience and technical considerations. Hip Int. 2009; 19:215–220.

19. Gruen TA, McNeice GM, Amstutz HC. "Modes of failure" of cemented stem-type femoral components: a radiographic analysis of loosening. Clin Orthop Relat Res. 1979; (141):17–27.
20. Kim YH, Kim JS, Oh SH, Kim JM. Comparison of porous-coated titanium femoral stems with and without hydroxyapatite coating. J Bone Joint Surg Am. 2003; 85-A:1682–1688.

21. Engh CA Jr, Claus AM, Hopper RH Jr, Engh CA. Long-term results using the anatomic medullary locking hip prosthesis. Clin Orthop Relat Res. 2001; (393):137–146.

22. Brooker AF, Bowerman JW, Robinson RA, Riley LH Jr. Ectopic ossification following total hip replacement. Incidence and a method of classification. J Bone Joint Surg Am. 1973; 55:1629–1632.
23. McMinn DJ, Daniel J, Pradhan C, Ziaee H. Avascular necrosis in the young patient: a trilogy of arthroplasty options. Orthopedics. 2005; 28:945–947.

24. Thomas W, Lucente L, Mantegna N, Grundei H. ESKA (CUT) endoprosthesis. Orthopade. 2004; 33:1243–1248.
25. Walker PS, Culligan SG, Hua J, Muirhead-Allwood SK, Bentley G. Stability and bone preservation in custom designed revision hip stems. Clin Orthop Relat Res. 2000; (373):164–173.

26. Yoo JH, Kim SG, Han CD, Oh HC, Yoon HK. Cementless total hip arthroplasty using VerSys fiber metal midcoat stem: a minimum 3-years follow-up. J Korean Hip Soc. 2010; 22:45–51.

27. Kim YH, Oh SH, Kim JS. Primary total hip arthroplasty with a second-generation cementless total hip prosthesis in patients younger than fifty years of age. J Bone Joint Surg Am. 2003; 85-A:109–114.

28. Westphal FM, Bishop N, Honl M, Hille E, Püschel K, Morlock MM. Migration and cyclic motion of a new short-stemmed hip prosthesis--a biomechanical in vitro study. Clin Biomech (Bristol, Avon). 2006; 21:834–840.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download