Abstract
Purpose
To compare the postoperative complications and cost-effectiveness of simultaneous and staged bilateral total hip arthroplasty (THA), using a minimally invasive two-incision technique.
Materials and Methods
All 206 patients who underwent simultaneous or staged bilateral THA using a modified, minimally invasive two-incision between January 2004 and November 2009 were registered and divided into a simultaneous bilateral THA group (group A, 147 patients) and staged bilateral THA group (group B: 59 patients). Staged THA was performed on group B with interval of at least 2 months between the initial and second surgery. Clinical evaluations, amount of blood loss, need for transfusion, complications and costeffectiveness were compared.
Results
Perioperative morbidity rates were similar in the two groups (P=0.546) and overall complications were not significant between the groups. Average length of hospital stay was significantly shorter in group A than in group B (average 14.6 days vs. 25.3 days; P<0.001). Total medical cost was significantly higher in group B than in group A (average 9,236 US dollars vs. 11,163 US dollars). Patients in group A required more blood transfusions than those in group B (3.02 vs. 1.90 units; P=0.003), although blood loss in the two groups were similar (892 vs. 917 ml P=0.613).
Bilateral simultaneous total hip arthroplasty (THA) was first reported in 19711). The need for a simultaneous procedure is still debatable23456). Reported rates for performance of simultaneous bilateral THA vary from 13.5% to 50% according to the presence of co-morbidity, patient socioeconomic status, and surgeon experience178). The alleged benefits of simultaneous bilateral sequential THA as compared with staged bilateral THA performed as a staged operation include shorter hospitalization, operation and rehabilitation times, and greater cost-effectiveness7910). However, intraoperative blood loss and postoperative transfusion requirements are reportedly greater for simultaneous bilateral THA8). Other studies have reported rates of complications after simultaneous bilateral THA that are the same or lower than those after staged bilateral THA or unilateral THA7811). But, other studies have found that the rates of surgical site infection after simultaneous bilateral THA are higher than after unilateral or staged bilateral THA34). Thus, not surprisingly, discussion continues regarding the advantages and disadvantages of bilateral simultaneous versus staged procedures in terms of safety and cost effectiveness2345612).
We hypothesized that simultaneous bilateral THA is both safe and effective, as compared with staged bilateral THA. In order to prove this hypothesis, we evaluated the operation costs, preoperative and postoperative morbidities, mortalities and clinical outcomes in patients that had undergone simultaneous bilateral or staged THA.
Two hundred and six patients (157 men and 49 women; 412 hips) treated at our institution from January 2004 to November 2009 were retrospectively reviewed. The average age was 43.2±12.4 years (range, 17-79 years). Simultaneous bilateral THA was performed when both hips had symptomatic lesions and functional disabilities. Cases of femoral head osteonecrosis was included. However, patients with a co-morbidity increasing the risk of mortality, and patients with factors that prohibited early rehabilitations after simultaneous bilateral THAs were excluded. All operations were performed by one surgeon (T.R.Y.), who had previously performed more than 500 minimally invasive surgeries. The internal review board of our hospital approved the study protocol (IRB No. 2011-064) and informed consent was obtained from all patients.
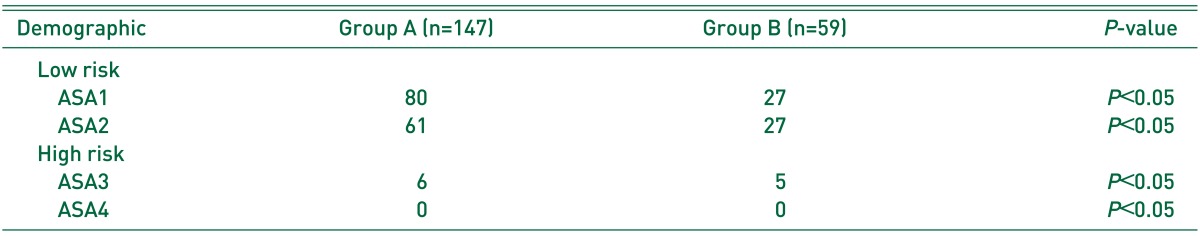
To compare simultaneous bilateral THA and staged THA, patients were allocated to one of two groups. Group A comprised 147 patients who underwent simultaneous bilateral THA. Group B comprised 59 patients who underwent staged bilateral THA. The two groups were dictated by the patients' choice of operation method. The groups were compared in terms of functional outcomes, complications, blood transfusion requirements and cost-effectiveness. In group B, patients were discharged after first THA and readmission for second THA. Times between the initial and second operations in group B were greater than 2 months (mean, 18.7±16.6 months). The two groups had similar demographics, body mass index values, and pre-operative American Society of Anesthesiologists (ASA) classification (Table 1, 2). Clinical evaluations were performed using preoperative and last follow-up Harris Hip Scores (HHS) and Western Ontario and McMaster Universities (WOMAC) scores. Patients were followed up at 1, 3, 6, and 12 months, and annually thereafter. Blood loss was determined by summing intraoperative suction drainage, soaked, and postoperative Hemovac® (Zimmer, Warsaw, IN, USA) drainage quantities. The usual Hemovac® drainage was under 100 ml. Needs for transfusion intraoperatively and postoperatively in wards were determined by hemoglobin (Hgb) level. A blood transfusion was performed in the following cases: Hgb level ≤7 g/dL, Hgb level ≤8 g/dL and patient with cardiovascular disease, Hgb level ≤8 g/dL and symptoms (chest pain, decreased orthostatic blood pressure or tachycardia unresponsive to fluids). Perioperative mortality was defined as death within 4 weeks of surgery. Thromboembolic prophylaxis was not routinely administered because the incidences of deep vein thrombosis and pulmonary embolism are low in Koreans131415). However, when patients had risk factors for thromboembolic disease, mechanical and chemophylatic prophylaxis (aspirin, low molecular-weight heparin) was performed as described by the American Academy of Orthopedic Surgeons16). Lower extremity venography was performed selectively when a patient complained of calf pain or swelling, and showed symptoms of deep vein thrombosis. When chest symptoms raised suspicion of a pulmonary theomboembolism, chest computed tomographic angiography was performed. The two groups were compared for complications that included infections, periprosthetic fractures, and dislocations.
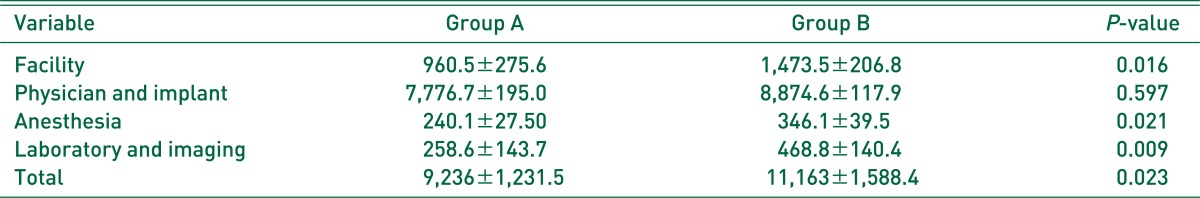
Total medical costs were calculated from the day of admission to discharge from hospital. All fees for plain radiographs, laboratory tests, surgery, anesthesia, and consultations were included. Governmental medical insurance payment was not included.
The surgical technique has been previously detailed17). All operations used a modified two-incision minimally invasive surgical technique. This technique enables access to the hip joint because it uses intermuscular and internervous planes while minimizing damage to the muscles and tendons around the hip joint so blood loss was minimized. The first incision was made anteriorly, and the first femoral neck osteotomy was performed through this anterior approach at the mid-cervical level with the primary aim of mobilizing the femur. Femoral neck osteotomy was revised to the level required for appropriate insertion and seating of the femoral stem. The acetabulum was then prepared by removing the overhanging soft tissue, including some portion of the joint capsule and the labrum. After exposure of the acetabulum, reaming was performed. The posterior skin incision was placed at the posterolateral aspect of the hip with the hip flexed, and the joint capsule was reached by inter-muscular dissection between fibers of the piriformis and gluteus medius. Under direct visualization, the joint capsule was incised on the posterosuperior aspect of the hip joint. After preparing the proximal femur with a rasp, the size of the femoral component was determined by fluoroscopy and the femoral component was inserted. With an appropriately-sized trial implant in situ, a trial reduction was performed and leg length was evaluated both clinically and fluoroscopically. The hip was the put through a full range of motion to assess stability before the appropriately-sized implant was inserted. Subcutaneous adductor tenotomies were performed in selective patients found to have intraoperative abduction tightness. A negative suction drain was then placed in the joint through the anterior incision. The posterior and anterior joint capsules, fascia lata, and subcutaneous tissue were repaired layer-by-layer and the skin was closed. In all cases, cementless, ceramic-on-ceramic-bearing THA (M/L taper stem; Zimmer) was performed using Delta PF acetabular sockets (Lima-LTO, San Daniele del Friuli, Italy).
Postoperative rehabilitation protocol included placing an abduction pillow between the legs to prevent dislocation with an elastic stocking and limb mobilization to prevent deep vein thrombosis. Quadriceps strengthening exercises and sitting bedside were allowed on the day of the surgery as tolerated. Mobilization was recommended with tolerable weight bearing on the day after surgery.
SPSS for Windows Release ver. 17.0 (Chicago, IL, USA) was used for analysis. The independent t-test was used to compare the postoperative blood transfusion requirement, blood losses, HHS and WOMAC scores between the two study groups. Chi-square analysis was used to evaluate the ASA grade difference between two groups and incidences of complications. Significance was accepted for a P-value <0.05.
All 206 patients were followed-up. Mean follow-up was 34.4±20.2 months (range, 12.3-112.6 months). The postoperative HHS and WOMAC score showed no significant difference between the group A and group B (96.4 vs. 94.8 and 17.8 vs. 19.2, respectively).
Mean total blood losses were similar in group A and group B (926.4±341.2 ml and 978.0±389.3 ml, respectively). In group B, mean blood loss was 489.0±194.6 ml at each stage. In terms of the total amount of blood loss, no significant difference was found between group A and group B (P=0.612). Regarding mean transfusion amount, 3.02±2.63 units (1 unit of packed red blood cells, 320 ml) of packed red blood cells were transfused in group A and 1.90±2.15 units in group B, which was significant (P=0.003). Two patients from group B had large volume of transfusion (12 units and 14 units) because of underlying liver cirrhosis. No complications resulting from blood transfusion, such as urticaria, dyspnea, or shock, were encountered.
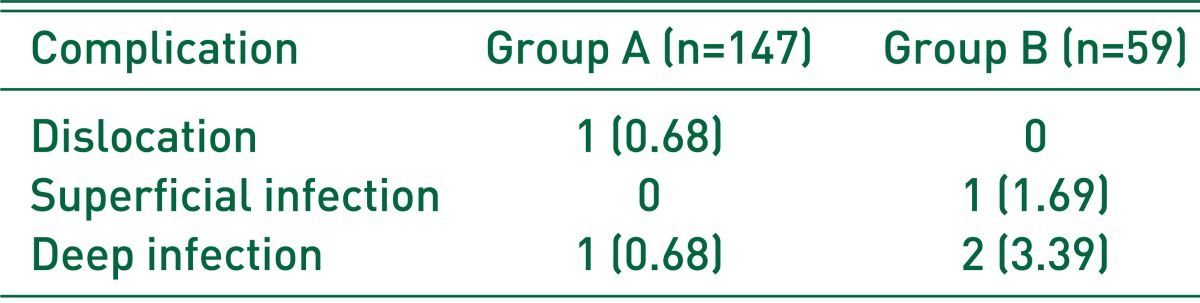
Perioperative morbidity rate of patients were similar in the two groups and no mortality occurred during followup. One case (0.68%) of deep infection and one case (0.68%) of dislocation occurred postoperatively in group A. In group B, there was one case (1.69%) of postoperative deep infection and two cases (3.39%) of postoperative superficial infection. No patient experienced fat embolism or pulmonary thromboembolism (Table 3).
The total medical cost was 9,236 US dollars in group A and 11,163 US dollars in group B (Table 4). The 20% higher total costs in group B was significant (P<0.05).
Mean hospital stay was greater in group A than in group B (mean 14.6±8.1 days vs. 12.6±4.8 days) from admission to discharge. Total mean hospital stay was significantly greater in group B (mean 25.3±9.8 days, P<0.05). During hospital stay, postoperative rehabilitation was performed as scheduled.
The safety of simultaneous bilateral THA remains debatable because of concerns about higher mortality rates and delayed postoperative rehabilitations23456). However, it is difficult to determine which patients should undergo simultaneous bilateral THA because the incidences of postoperative complications like postoperative infections, deep vein thrombosis, and fat embolism have not been well reported in the contexts of physical status, medical co-morbidities, and postoperative rehabilitation.
Nevertheless, several studies have described the outcomes of simultaneous bilateral THA. Kim et al.8) compared 978 patients that underwent simultaneous bilateral sequential THA with 1,666 patients that underwent unilateral THA at a mean follow-up of 10.5 years and 9.8 years, respectively, but found no significant differences between the two groups in terms of postoperative complications. Berend et al.7) concluded that simultaneous bilateral THA has advantages in younger patients even with possible increased risk of pulmonary complications. In this study, comparisons of bilateral THA in terms of simultaneous versus staged-operations revealed no significant difference in mortality and complications.
In this study, the time between first and second THA was more than 2 months in the staged procedure (mean 18.6±16.2 months). However, the optimal time has not been determined. Aghayev et al.18) reported good outcomes for a 6-month delay for staged THA, and concluded that a delay longer than 6 months increases the rate of complications. More research needed about optimal period.
In a previous study, we also reported good results for bilateral simultaneous THA using a two-incision, minimally invasive technique5). Unique characteristics of the anterolateral approach with muscle sparing and eventual decrease of the dislocation rate, compared with the posterolateral approach, may be the explanation. Furthermore, despite the longer time required for the two-incision, minimally invasive THA, our complication rates for simultaneous bilateral and staged-bilateral THA were acceptably low.
Group A required more blood transfusions than group B (3.02 vs. 1.90 units), which is similar to prior findings, in which simultaneous bilateral THA had a greater transfusion requirement19). We attribute this difference to the fact that simultaneous bilateral THA can easily surpass the threshold Hgb level that prompts blood transfusion. The present and previous results highlight that patients with compromised Hgb levels should not be selected for simultaneous bilateral THA, and blood transfusion should be carefully performed for those patients.
Korean governmental medical insurance policy results in a longer hospital stay for patients with THA, since postoperative rehabilitation is also begun. Thus, the shorter hospital stays required for simultaneous THA and early rehabilitation contribute to reduce costs, which offers a means of reducing medical cost burdens in bilaterally symptomatic hip patients. Presently, performing simultaneous bilateral THA in bilaterally symptomatic patients lessened medical costs by 20%.
The limitation of this study was the low mortality during the study period, since patient selection involved preoperative consultation from internal medicine doctors and anesthesiologists, and because the prevalence of disease was markedly different from Western countries. Patients judged to be at high risk during the consultations (ASA 3 or 4) had their operations delayed or where exempt from this study. These facts could have lowered the mortality. The all patients included in this study had avascular necrosis of the femoral head, which is predominantly encountered hip joint disease in Korea. The disease is the main reason for THA (about 80%), more than degenerative hip joint osteoarthritis1920). This can also lower the mortality rate, since the patients are usually young and healthy, except for the affected hip joints, and because a high level of activity can be expected after rehabilitation. For other age and disease patients groups, markedly different rates of mortality and complications would be expected.
Simultaneous bilateral THA compares favorably with staged THA in terms of outcomes, complications, and cost-effectiveness. If simultaneous bilateral minimal invasive two-incision THA was performed by skilled surgeon, that is a good option in terms of low complication rates and socioeconomic cost. However, simultaneous bilateral THA should be carefully performed for the patients with compromised Hgb level.
References
1. Jaffe WL, Charnley J. Bilateral Charnley low-friction arthroplasty as a single operative procedure. A report of fifty cases. Bull Hosp Joint Dis. 1971; 32:198–214. PMID: 5128234.
2. Alfaro-Adrián J, Bayona F, Rech JA, Murray DW. One- or two-stage bilateral total hip replacement. J Arthroplasty. 1999; 14:439–445. PMID: 10428224.

3. Ritter MA, Randolph JC. Bilateral total hip arthroplasty: a simultaneous procedure. Acta Orthop Scand. 1976; 47:203–208. PMID: 1274544.

4. Ritter MA, Stringer EA. Bilateral total hip arthroplasty: a single procedure. Clin Orthop Relat Res. 1980; 149:185–190. PMID: 7408301.
5. Ritter MA, Vaughn BK, Frederick LD. Single-stage, bilateral, cementless total hip arthroplasty. J Arthroplasty. 1995; 10:151–156. PMID: 7798095.

6. Salvati EA, Hughes P, Lachiewicz P. Bilateral total hipreplacement arthroplasty in one stage. J Bone Joint Surg Am. 1978; 60:640–644. PMID: 681382.

7. Berend ME, Ritter MA, Harty LD, et al. Simultaneous bilateral versus unilateral total hip arthroplasty an outcomes analysis. J Arthroplasty. 2005; 20:421–426. PMID: 16124956.
8. Kim YH, Kwon OR, Kim JS. Is one-stage bilateral sequential total hip replacement as safe as unilateral total hip replacement? J Bone Joint Surg Br. 2009; 91:316–320. PMID: 19258605.

9. Huotari K, Lyytikäinen O, Seitsalo S. Hospital Infection Surveillance Team. Patient outcomes after simultaneous bilateral total hip and knee joint replacements. J Hosp Infect. 2007; 65:219–225. PMID: 17275961.

10. Jewett BA, Collis DK. Sequential bilateral total hip replacement during the same hospitalization. Clin Orthop Relat Res. 2005; 441:256–261. PMID: 16331012.

11. Ritter MA, Harty LD, Davis KE, Meding JB, Berend M. Simultaneous bilateral, staged bilateral, and unilateral total knee arthroplasty. A survival analysis. J Bone Joint Surg Am. 2003; 85-A:1532–1537. PMID: 12925634.
12. Tsiridis E, Pavlou G, Charity J, Tsiridis E, Gie G, West R. The safety and efficacy of bilateral simultaneous total hip replacement: an analysis of 2063 cases. J Bone Joint Surg Br. 2008; 90:1005–1012. PMID: 18669954.
13. Kim YH, Kim VE. Factors leading to low incidence of deep vein thrombosis after cementless and cemented total knee arthroplasty. Clin Orthop Relat Res. 1991; 273:119–124. PMID: 1959258.
14. Kim YH, Oh SH, Kim JS. Incidence and natural history of deep-vein thrombosis after total hip arthroplasty. A prospective and randomised clinical study. J Bone Joint Surg Br. 2003; 85:661–665. PMID: 12892186.
15. Kim YH, Suh JS. Low incidence of deep-vein thrombosis after cementless total hip replacement. J Bone Joint Surg Am. 1988; 70:878–882. PMID: 3392086.

16. Johanson NA, Lachiewicz PF, Lieberman JR, et al. American academy of orthopaedic surgeons clinical practice guideline on prevention of symptomatic pulmonary embolism in patients undergoing total hip or knee arthroplasty. J Bone Joint Surg Am. 2009; 91:1756–1757. PMID: 19571100.
17. Diwanji SR, Park KS, Yoon TR, Seo HY, Wie JS. Bilateral simultaneous two-incision minimally invasive total hip arthroplasty. J Orthop Sci. 2009; 14:517–524. PMID: 19802662.

18. Aghayev E, Beck A, Staub LP, et al. Simultaneous bilateral hip replacement reveals superior outcome and fewer complications than two-stage procedures: a prospective study including 1819 patients and 5801 followups from a total joint replacement registry. BMC Musculoskelet Disord. 2010; 11:245. PMID: 20973941.

19. Kang JS, Park S, Song JH, Jung YY, Cho MR, Rhyu KH. Prevalence of osteonecrosis of the femoral head: a nationwide epidemiologic analysis in Korea. J Arthroplasty. 2009; 24:1178–1183. PMID: 19640674.
20. Kim HA, Koh SH, Lee B, et al. Low rate of total hip replacement as reflected by a low prevalence of hip osteoarthritis in South Korea. Osteoarthritis Cartilage. 2008; 16:1572–1575. PMID: 18558502.

Table 1
Preoperative Demographic Data of Simultaneous vs. Staged Operations in Bilateral THA
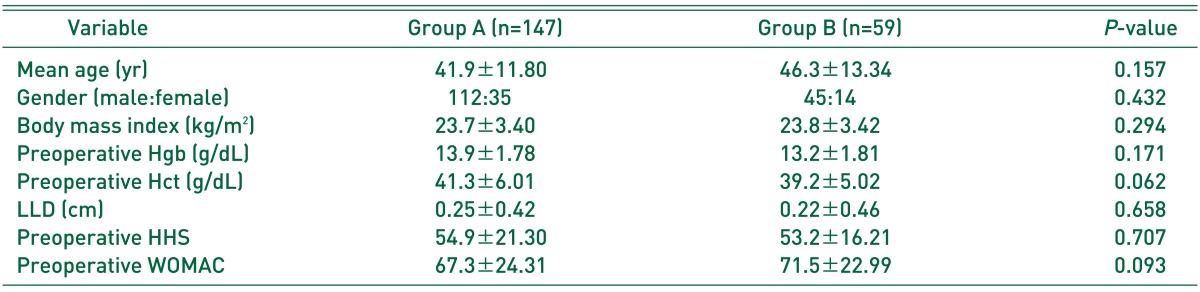
Values are presented as mean±standard deviation or number only.
Group A: simultaneous bilateral THA group, group B: staged bilateral THA group.
THA: total hip arthroplasty, Hgb: hemoglobin, Hct: hematocrit, LLD: leg length discrepancy, HHS: Harris Hip Scores, WOMAC: Western Ontario and McMaster Universities Scores.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download