This article has been
cited by other articles in ScienceCentral.
Abstract
Facial asymmetry can be classified into the rolling-dominant type (R-type), translation-dominant type (T-type), yawing-dominant type (Y-type), and atypical type (A-type) based on the distorted skeletal components that cause canting, translation, and yawing of the maxilla and/or mandible. Each facial asymmetry type represents dentoalveolar compensations in three dimensions that correspond to the main skeletal discrepancies. To obtain sufficient surgical correction, it is necessary to analyze the main skeletal discrepancies contributing to the facial asymmetry and then the skeletal-dental relationships in the maxilla and mandible separately. Particularly in cases of facial asymmetry accompanied by mandibular yawing, it is not simple to establish pre-surgical goals of tooth movement since chin deviation and posterior gonial prominence can be either aggravated or compromised according to the direction of mandibular yawing. Thus, strategic dentoalveolar decompensations targeting the real basal skeletal discrepancies should be performed during presurgical orthodontic treatment to allow for sufficient skeletal correction with stability. In this report, we document targeted decompensation of two asymmetry patients focusing on more complicated yaw-dependent types than others: Y-type and A-type. This may suggest a clinical guideline on the targeted decompensation in patient with different types of facial asymmetries.
Keywords: Facial asymmetry, Decompensation, Orthognathic surgery, Mandibular yaw
INTRODUCTION
Facial asymmetry is caused by many skeletal discrepancies in the cranium, maxilla, and mandible. Excluding the serious cranial variations observed in patients with syndromic deformities, facial skeletal compartments that are distorted in the vertical, transverse, and horizontal directions produce facial asymmetries with canting, translation, and yawing of the maxilla and/or mandible,
123 and these asymmetries can be categorized into several patterns. Out of the many reported classification systems for facial asymmetry,
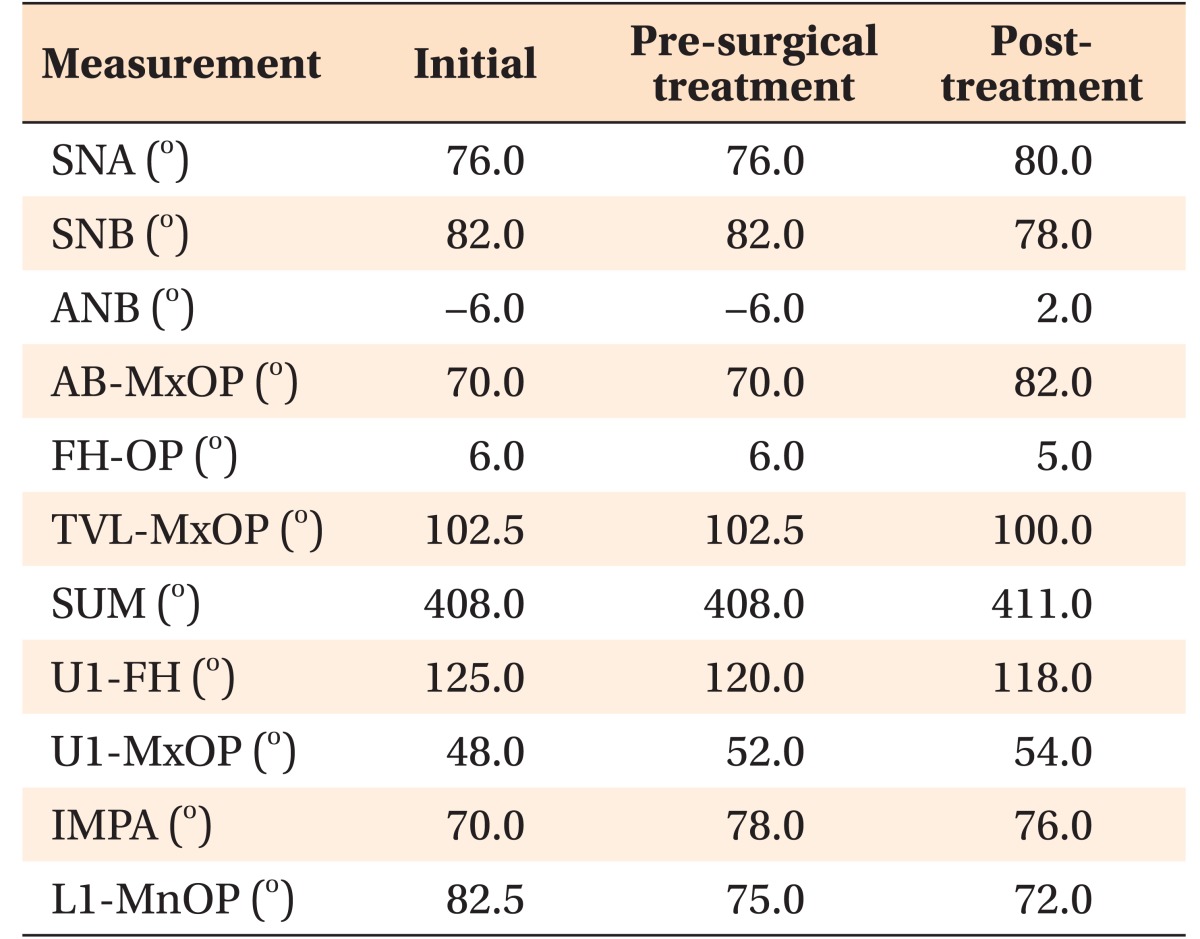
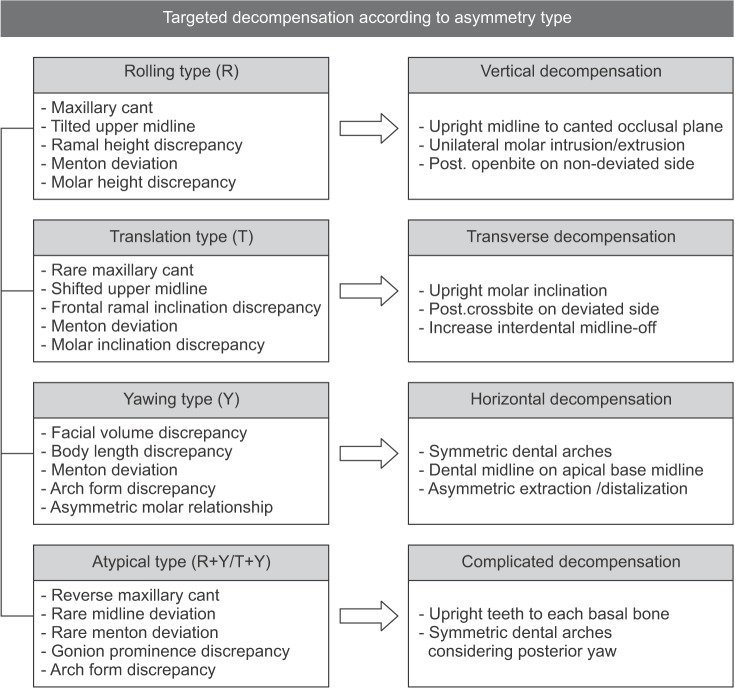
456 we applied a practical system for establishing the presurgical goals of orthodontic decompensation for maximum surgical correction as follows; rolling-dominant type (R-type), translation-dominant type (T-type), yawing-dominant type (Y-type), and atypical type (A-type) (
Figure 1).
Presurgical dentoalveolar decompensation should be strategically accomplished since skeletal discrepancies exhibit characteristic patterns according to different types of asymmetry, which may be disguised by differential dentoalveolar compensations.
5 The R-type asymmetry is characterized by a chin deviation and a maxillary midline that is tilted towards the deviated side. It is mostly associated with vertical discrepancies in the ramus and maxillary heights, which cause maxillary canting.
47 The different molar height between the sides is noticeable as a vertical compensation. The T-type asymmetry, which is also called mandibular body asymmetry, results in a chin deviation and a maxillary midline shift due to the lateral translation of the maxilla and/or mandible. This is mostly caused by distinctively different frontal ramus inclinations but not by discrepancies in ramus height and mandibular body height. The different molar inclinations between the sides result in transverse compensation, irrespective of maxillary canting. Accordingly, in the R-type asymmetry, vertical decompensation of the molar height to the level of the maxillary and mandibular transverse occlusal planes occurs, so that the molar height is parallel to each basal reference line. Meanwhile, in the T-type asymmetry, transverse decompensation of the molar inclinations occurs, so that the molar inclinations are more upright buccolingually.
68
In contrast, the Y-type asymmetry represents more complicated and confusing features of dentoalveolar compensation. It is characterized by a serious chin deviation due to the horizontal yawing of the maxilla and/or mandible to the same sides, which is accompanied by different body lengths and distances from the gonion to the midsagittal plane. Discrepancy can occur in the arch forms between the basal and dental arches, and it frequently appears in combination with the R-type or T-type asymmetry, which worsens chin deviation in one direction. In contrast, the A-type asymmetry consists of mandibular yawing that conceals the R-type or T-type asymmetry, which usually leads to reverse maxillary canting or shifting towards the opposite side of the mandibular deviation. Accordingly, chin deviation or maxillary midline deviation is rarely seen, and different anteroposterior prominences of the zygomas and gonions are noted in relation to the posterior yawing of the mandible. Horizontal decompensation of the distorted dental arch, so that it matches the basal arch in order to obtain proper correction of mandibular body yawing, would be the key for maximum corrections of the Y-type asymmetries. In particular, the A-type asymmetries require complicated decompensations to correct the asymmetric facial volumes and prominences, especially in the posterior facial area. The main principle of the dental decompensations suggested here is to position all of the teeth upright over each basal bone from a three-dimensional (3D) perspective in each type of facial asymmetry by applying targeted decompensation.
Although the surgery-first approach has been widely accepted in recent years for immediate esthetic improvement of skeletal discrepancies,
9 it has definite limitations in treating patients with facial asymmetries, especially when they have been diagnosed with the Y-type or A-type asymmetry accompanied by skeletal yawing. Targeted 3D decompensation is still necessary for sufficient surgical jaw movement and for maximum surgical stability, particularly in patients with such complicated facial asymmetry. In this comparative report of two cases affected by different types of mandibular yawing, we suggest a guideline for the application of targeted decompensation in patients with different types of facial asymmetries.
DIAGNOSIS AND ETIOLOGY
Case 1: Y-type asymmetry
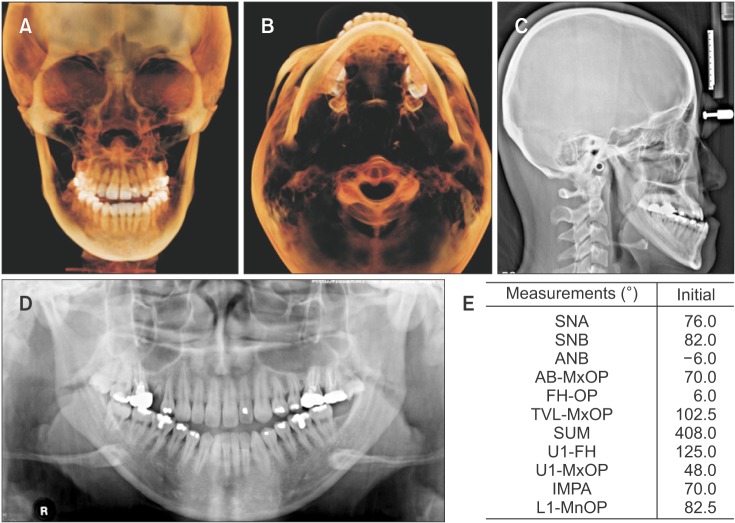
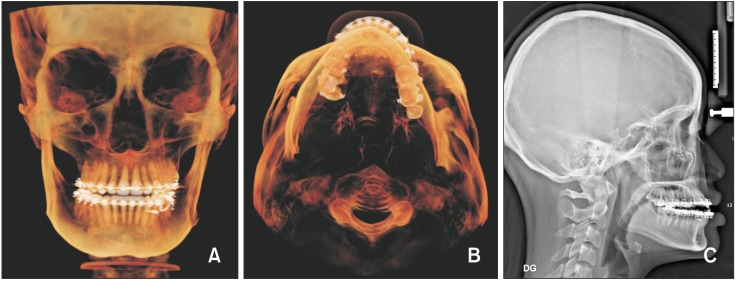
A 25-year-old woman with chief complaints of facial asymmetry and an anterior crossbite was diagnosed with a skeletal Class III hyperdivergent pattern with a Y-type skeletal asymmetry. Cephalometric and cone-beam computed tomography (CBCT) analyses (
Figure 2,
Tables 1 and
2) revealed a chin deviation to the left side in accordance with a mandibular yawing to the deviated side, with a longer mandibular body length on the right side and a longer distance from the right gonion to the midsagittal plane. Maxillary yawing to the deviated side was seen in the same direction as the mandibular yawing. The facial volume and width were more prominent on the right side than on the left because of the same directional anterior yawing of the maxilla and mandible. The maxillary incisors were tilted to the right, and the maxillary dental midline was deviated to the right from the apical base midline. The mandibular dental midline was shifted to the right side from the apical base midline. Intraoral examination revealed a Class III molar relationship, anterior crossbite, open bite, root rest of #15, extrusion of #17 and #27, very thin periotype, and midline discrepancy. Minor crowding and distorted dental arch forms with different anteroposterior molar positions in both dentitions were also observed (
Figure 3).
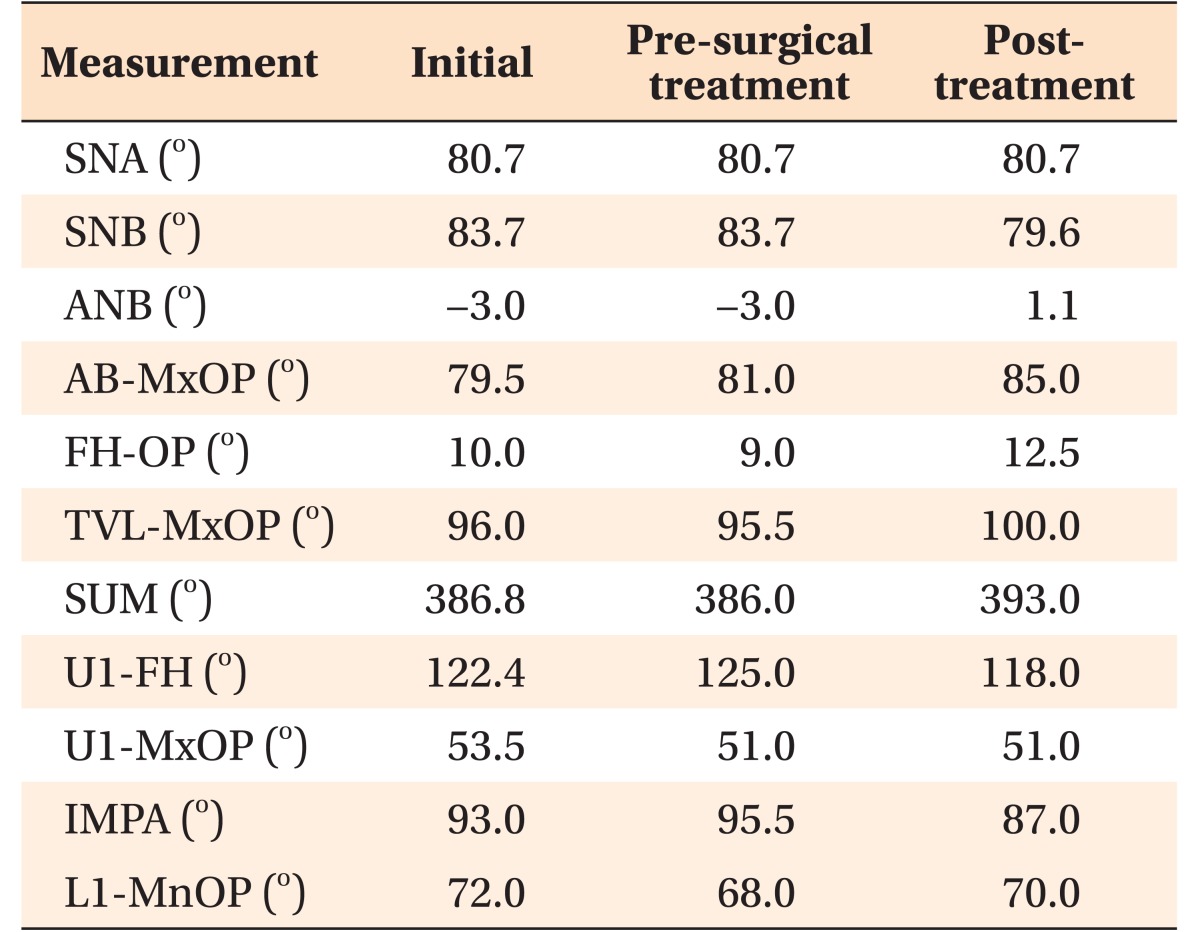
Case 2: A-type asymmetry
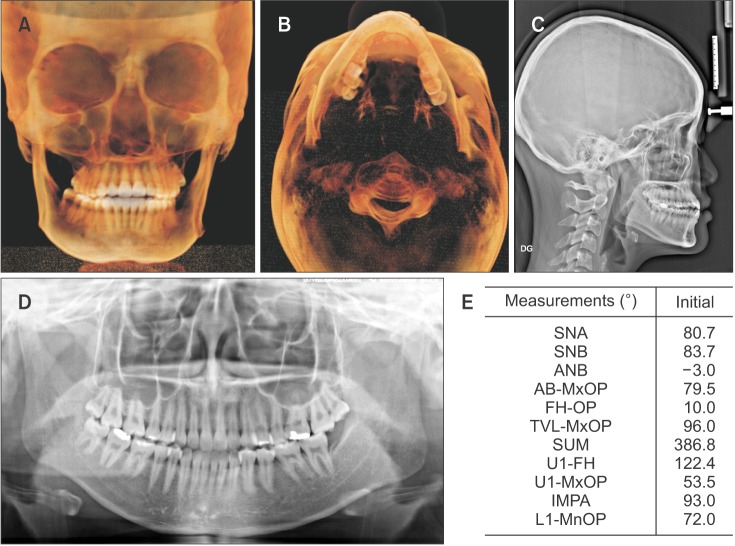
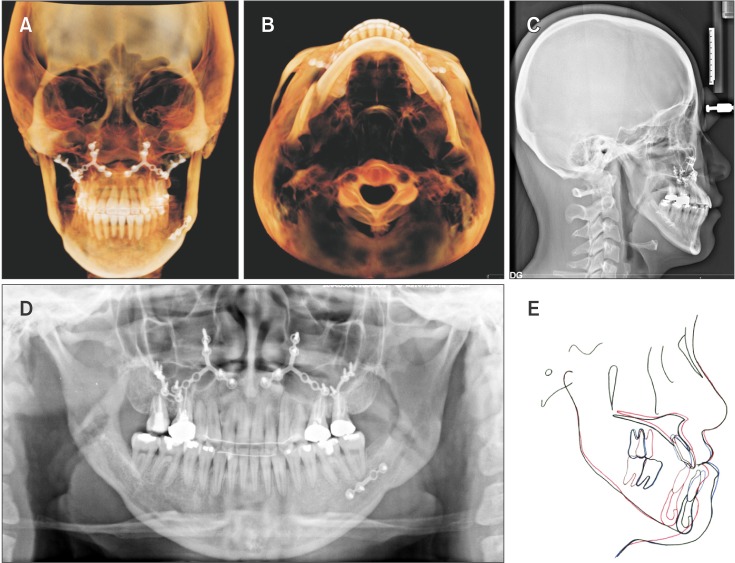
A 19-year-old woman with a chief complaint of different facial volumes and prominences was diagnosed with a skeletal Class III hypodivergent pattern with A-type skeletal asymmetry. Cephalometric and CBCT analyses (
Figure 4,
Tables 3 and
4) revealed that the mandible was translated to the right side in accordance with the different frontal ramus inclination, and a concomitant posterior yaw of the mandible to the left side was observed. Owing to the counterbalanced asymmetry pattern, the chin was not deviated to the right side to the same extent as the translated mandible. The facial volume and width were more prominent on the right side than on the left side. A maxillary transverse occlusal plane cant that was tilted towards the deviated side and was caused by a maxillary molar inclination discrepancy was seen. The buccally inclined maxillary right posteriors that were coupled with the lingually inclined mandibular right posteriors resulted in the transverse compensation of a positive buccal overjet on the deviated side. Intraoral examination revealed a Class III molar relationship, anterior edge-to-edge bite, asymmetric mandibular arch with lingual inclination of #45–47, and mild midline discrepancy, despite the severe skeletal discrepancy. Horizontal compensations of a slightly different mandibular molar position in the anteroposterior direction and a similar buccal overjet between the left and right sides were also seen (
Figure 5).
TREATMENT OBJECTIVES AND ALTERNATIVES
Case 1
Presurgical orthodontic goals in this case highlighted horizontal decompensation of the maxillary and mandibular arches. In brief, we planned sagittal decompensation of the incisors' inclinations for correcting the skeletal Class III relationship in order to retract the maxillary incisors by extracting the second premolars and to procline the mandibular incisors by anterior decrowding. Simultaneously, we planned distal uprighting of the mandibular left posteriors in order to create the space for anterior crowding, more on the left side than on the right, by shifting the mandibular dental midline to the left side after alignment. In the transverse aspect, buccal uprighting of the mandibular canine and premolars, rather than the molars, was required on the left side to increase the negative buccal overjet. The focus of decompensation was to position all the tilted teeth upright on each basal bone for restoring the symmetry of the distorted dental arches to be consistent with that of the basal arch form.
The surgical objectives were as follows: correction of facial asymmetry and chin deviation, advancement of the maxilla, surgical steepening of the occlusal plane, asymmetric setback of the mandible, and reduction of facial height.
Case 2
The main presurgical orthodontic goal was to correct the buccolingual inclination and mesiodistal position of the posterior teeth simultaneously to the direction of restoring the distorted dental arches such that they matched the basal arch form. We planned buccal uprighting of the mandibular right posteriors and palatal uprighting of the maxillary right posteriors in order to create buccal crossbite on the mandibular translated side (right). Moreover, we planned on progressively increasing the negative buccal overjet (from the canine to the second molar) on the right side to allow for a symmetric mandibular dental arch form. In addition, distal uprighting of the mandibular left posterior teeth with lingual movement of the molars was needed. The feature that distinguished Case 2 the most from Case 1 was that dental midline discrepancy would not increase after presurgical orthodontic treatment and the posterior part of the dental arch would be the target of decompensation. Sagittal decompensation of the maxillary and mandibular incisors and vertical decompensation of molar heights were not critically required in this case.
The surgical objectives included the correction of facial asymmetry with improvement of posterior facial volume, surgical steepening of the occlusal plane, asymmetric mandibular setback, and improvement of facial balance.
TREATMENT PROGRESS
Case 1
To restore the ideal axial inclinations of the maxillary incisors, we extracted the maxillary second premolars and closed the differential space between the left (moderate anchorage) and right sides (maximum anchorage). Asymmetric Class II intermaxillary elastics were applied to reveal the real dental midline discrepancy as well as to increase the negative overjet. A miniscrew was implanted between the mandibular left first and second molars to apply distal and buccal forces on the mandibular left posterior teeth (
Figures 6,
7, and
Table 2).
Maxillary Le Fort I with mandibular bilateral sagittal split ramus osteotomy (BSSRO) was performed. Maxillary extraction space closure was completed during the postsurgical orthodontic treatment.
Case 2
On the mandibular translated side (right), we used crisscross up-and-down elastics with a Class II vector for not only extrusive uprighting of the posteriors to create the buccal crossbite but also to create mesial movement of the mandibular posteriors to match the dental arch with the basal arch form. On the left side, however, up-and-down cross elastics were applied for lingual movement of the mandibular posteriors and for increasing the buccal overjet. An open coil spring was used between the mandibular first premolar and first molar for distal uprighting of the molars. Concomitantly, a miniscrew was implanted between the mandibular canine and first premolar for maintaining the dental midline under the application of the open coil spring and asymmetric Class II intermaxillary elastics (
Figures 8,
9, and
Table 4).
Maxillary Le Fort I with malar augmentation was performed on the left side, and mandibular BSSRO with additional mandibular border shaving was performed on the right side.
RESULTS
Case 1
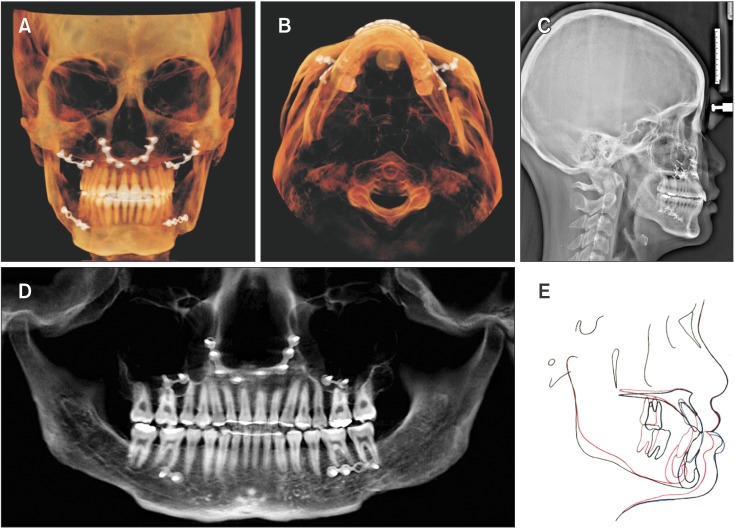
The total treatment period was 30 months, and the post-treatment photographs and CBCT images showed successful results, including improvement of the facial asymmetry and prognathic chin. In brief, sufficient correction of the sagittal intermaxillary relationship and reduction of the mandibular facial height were achieved. The comparison of the initial and final axial CBCT images indicated anterior yawing correction of the maxilla and mandible in the same direction brought about by the presurgical horizontal decompensation. A Class II molar relationship with ideal overjet and overbite were achieved, and the facial midline coincided with the maxillary dental midline and mandibular dental midline (
Figures 10,
11, and
Table 2).
Case 2
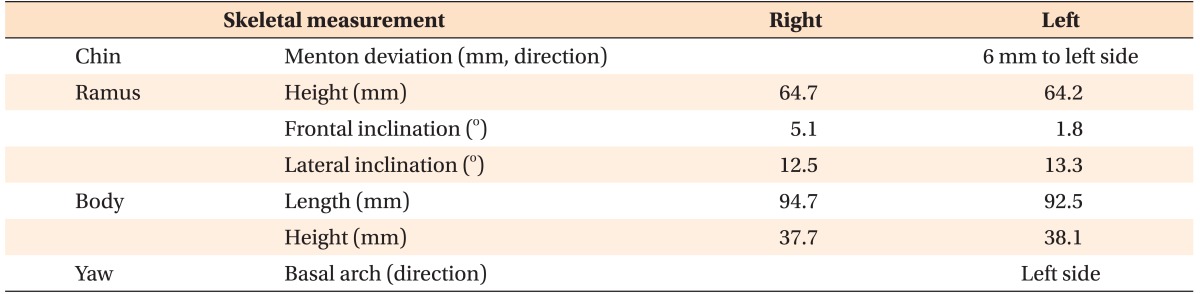
The total treatment period was 20 months. Mandibular symmetry and balanced facial volume were accomplished following the bimaxillary orthognathic surgery. The post-treatment axial CBCT images indicated sufficient yawing correction of the mandible due to targeted horizontal decompensation in the posterior teeth. The post-treatment frontal CBCT images showed improvement of the posterior facial volume and width, regardless of the unchanged frontal ramus inclination. The symmetric antero-posterior mandibular molar position, restoration of the distorted mandibular dental arch, ideal overjet and overbite, and favorable interdigitation were achieved (
Figures 12,
13, and
Table 4).
DISCUSSION
Yaw-dependent facial asymmetries were successfully corrected in two cases by using bimaxillary orthognathic surgeries after presurgical targeted decompensations. Owing to the more complicated and confusing skeletal-dental characteristics in the Y-type asymmetry, it is important to analyze first the 3D skeletal discrepancies that contributed to the facial asymmetry and then the skeletal-dental relationships in the maxilla and mandible separately on CBCT images. Moreover, the direction and amount of dental decompensations could be established only after considering the possible ranges of teeth movements within the alveolar housing.
The patient in Case 1, who was diagnosed with a Y-type asymmetry and skeletal Class III hyperdivergent pattern, received presurgical orthodontic treatment that focused on horizontal decompensation. The main factor in the facial asymmetry was the mandibular yawing to the left side with a longer right mandibular body, which resulted in chin deviation to the yawing side. Maxillary yawing in the same direction was manifested by the more prominent facial volume and wider facial width on the right than on the left. The goal of the targeted decompensation in this patient was to upright all of the tilted teeth onto each basal bone in order to restore the symmetry of the distorted dental arches with the basal arch form and to upright the dental midline to coincide with the apical base midline. This horizontal decompensation exposed hidden interarch discrepancies that showed greater negative overjet on the deviated side in the canine and premolar areas than in the molar area in addition to greater anterior crossbite. The decompensation resulted in favorable correction of the facial asymmetry concomitant with the Class III sagittal discrepancy. If a patient with a Y-type asymmetry has compensated anteroposterior molar positions showing symmetric molar relationships between the sides, which was unlike the present case, then unilateral distalization of the mandibular posterior teeth on the deviated side or unilateral protraction of the mandibular posteriors on the non-deviated side should be performed to achieve the required amount of surgical setback or advancement of the mandible. Asymmetric biomechanics are usually applied to decompensate for the dental arch discrepancies, and asymmetric premolar extraction can be used in cases with severe crowding.
The patient in Case 2 was categorized as having an A-type asymmetry and mixed skeletal discrepancies composed of mandibular translation to the right side in the frontal view and mandibular yawing towards the opposite side of the translation in the axial view. Establishing the goal of the preoperative decompensation might be confusing because the chief complaint of this patient was different facial volumes and prominences in the posterior facial area, including the gonion, between the sides; in addition, neither a chin deviation nor midline shift on the anterior face, which is usually noticeable in other types of asymmetry, was observed. Moreover, the compensatory movements that had occurred in the three dimensions masked the real discrepancies. The goal of the targeted decompensation in this patient was to apply the principles of both transverse and horizontal decompensations simultaneously because of the mixed skeletal discrepancies. For the transverse decompensation, the posterior crossbite was increased on the right side more in the molar area than in the premolar area because of obtaining a mandibular arch symmetry by buccal uprighting and concomitant mesial movement of the right mandibular posterior teeth for horizontal decompensation. Consequently, the Class III molar relationship was aggravated on the right side with no remarkable change of the mandibular dental midline in order to perform the maximum correction of the posterior yawing of the mandible along with mandibular setback. As such, another A-type asymmetry comprising a combination of R-type and Y-type asymmetries could be treated with both vertical and horizontal decompensations that target the basal skeletal discrepancies.
The targeted decompensations conducted to correct facial asymmetries should be balanced with corrections of sagittal and vertical skeletal malocclusions. In some challenging cases with anatomical limitations, such as thin alveolar housing and symphysis inhibiting sufficient dental decompensation, segmental osteotomies can be applied to expand the range of decompensation for successful surgical correction of the facial asymmetry.
10
CONCLUSION
Achieving dental decompensation during the presurgical orthodontic treatment is indispensable for maximizing surgical correction of facial asymmetry. Based on the principle of targeted decompensation from a 3D perspective, presurgical orthodontic treatment should be strategically planned in accordance with the characteristic facial asymmetry types.
Figure 1
Characteristic and targeted decompensation according to facial asymmetry types.
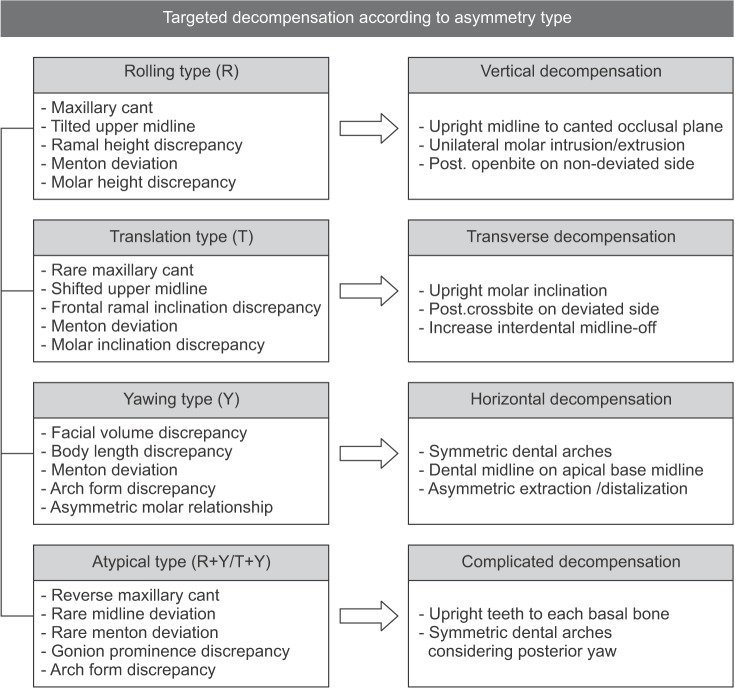
Figure 2
Pretreatment cephalometric and cone-beam computed tomography analyses of a patient (Case 1) with a yawing-dominant type asymmetry. A, Three-dimensional volume-rendering frontal image; B, axial image; C, lateral cephalograph; D, panoramic radiograph; E, cephalometric measurements.
Refer to
Table 2 for the definitions of each measurement.
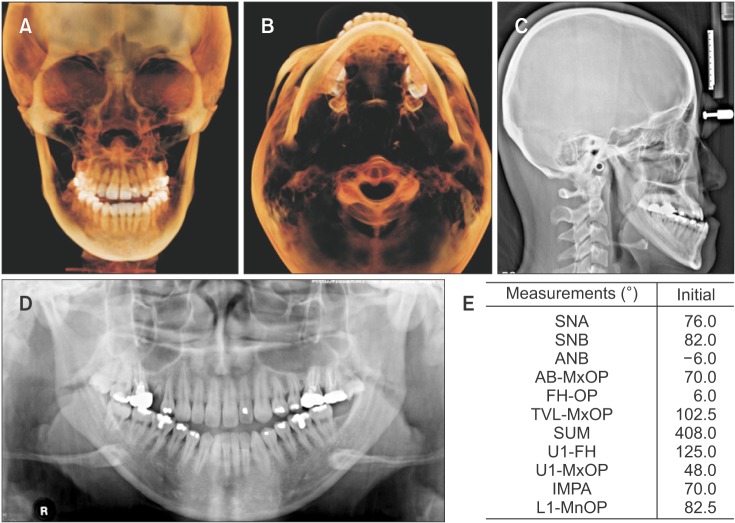
Figure 3
Pretreatment photographs of a patient (Case 1) with a yawing-dominant type asymmetry.

Figure 4
Pretreatment cephalometric and cone-beam computed tomography analyses of a patient (Case 2) with an atypical type asymmetry. A, Three-dimensional volume-rendering frontal image; B, axial image; C, lateral cephalograph; D, panoramic radiograph; E, cephalometric measurements.
Refer to
Table 2 for the definitions of each measurement.
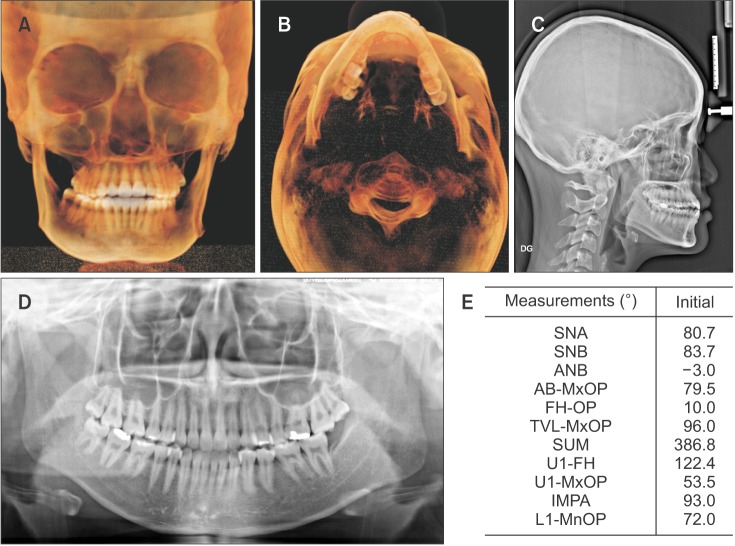
Figure 5
Pretreatment photographs of a patient (Case 2) with an atypical type asymmetry.

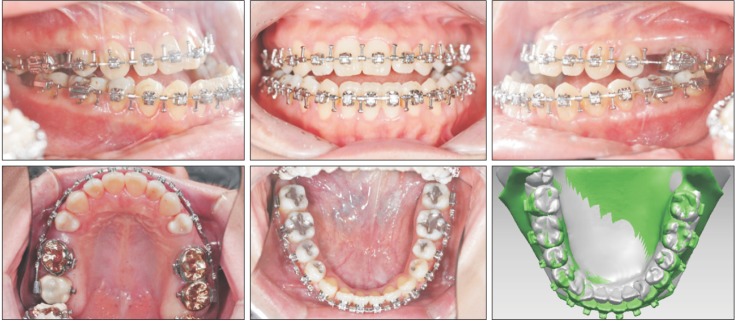
Figure 6
Presurgical intraoral photographs of a patient (Case 1) with a yawing-dominant type asymmetry, and three-dimensional superimposition of the initial and presurgical mandibular models. Gray color, initial mandibular model; green color, pre-surgical mandibular model.
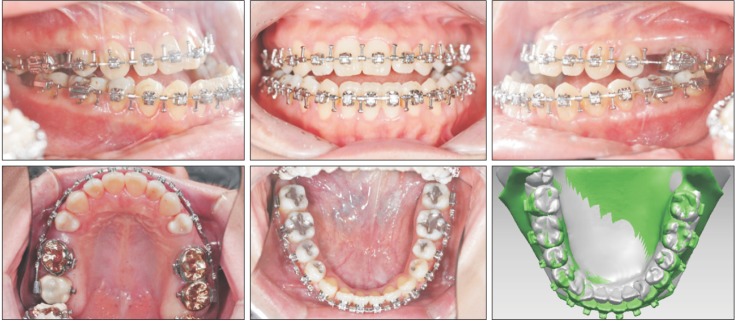
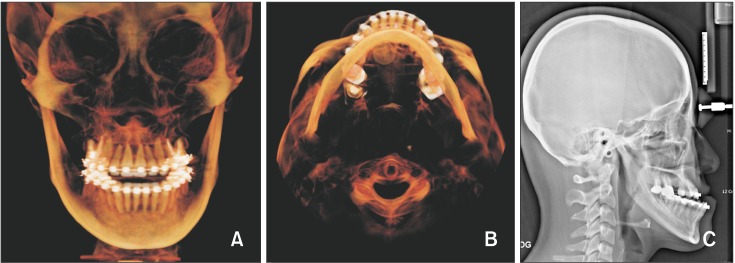
Figure 7
Presurgical three-dimensional volume-rendering frontal (A,) axial images (B,) and lateral cephalograph (C) of a patient (Case 1) with a yawing-dominant type asymmetry.
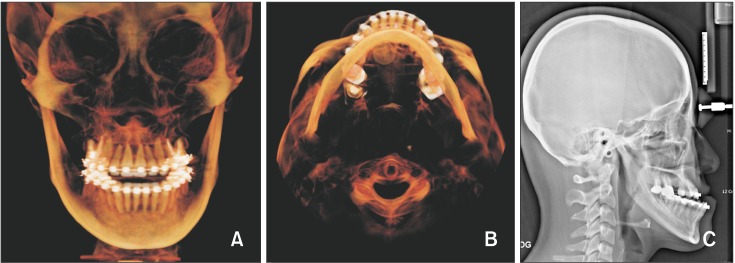
Figure 8
Presurgical intraoral photographs of a patient (Case 2) with an atypical type asymmetry, and three-dimensional superimposition of the initial and presurgical mandibular models. Gray color, initial mandibular model; green color, presurgical mandibular model.

Figure 9
Presurgical three-dimensional volume-rendering frontal (A,) axial images (B,) and lateral cephalograph (C) of a patient (Case 2) with an atypical type asymmetry.
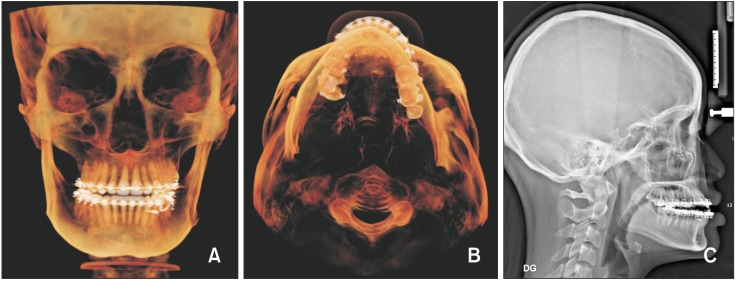
Figure 10
Post-treatmet cephalometric and cone-beam computed tomography images of a patient (Case 1) with a yawing-dominant type asymmetry. A, Three-dimensional volume-rendering frontal image; B, axial image; C, lateral cephalograph; D, panoramic radiograph; E, superim-position (black color, initial; blue color, presurgical; red color, post-treatment).
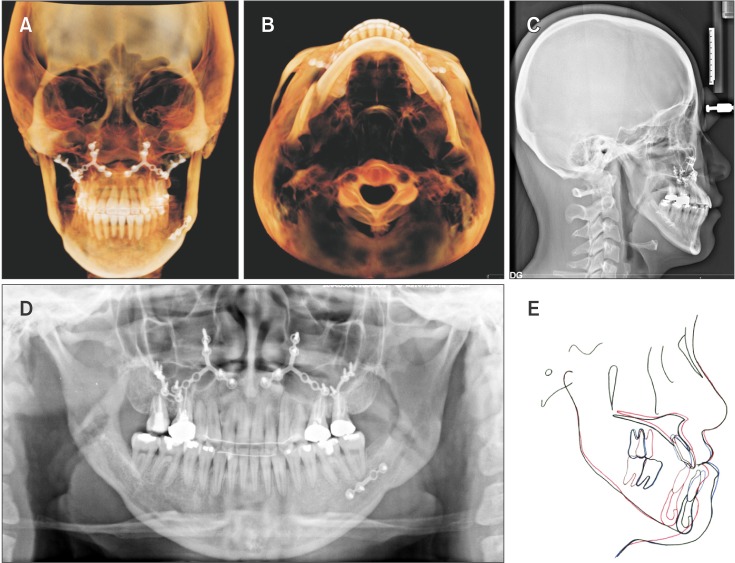
Figure 11
Post-treatment photographs of a patient (Case 1) with a yawing-dominant type asymmetry.

Figure 12
Post-treatmet cephalometric and cone-beam computed tomography images of a patient (Case 2) with an atypical type asymmetry: A, Three-dimensional volume-rendering frontal image; B, axial image; C, lateral cephalograph; D, panoramic radiograph; E, superimposition (black color, initial; blue color, presurgical; red color, post-treatment).
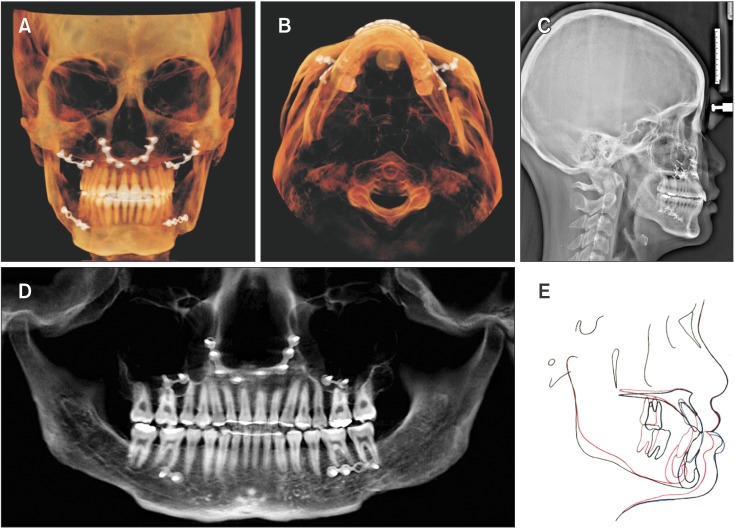
Figure 13
Post-treatment photographs of a patient (Case 2) with an atypical type asymmetry.

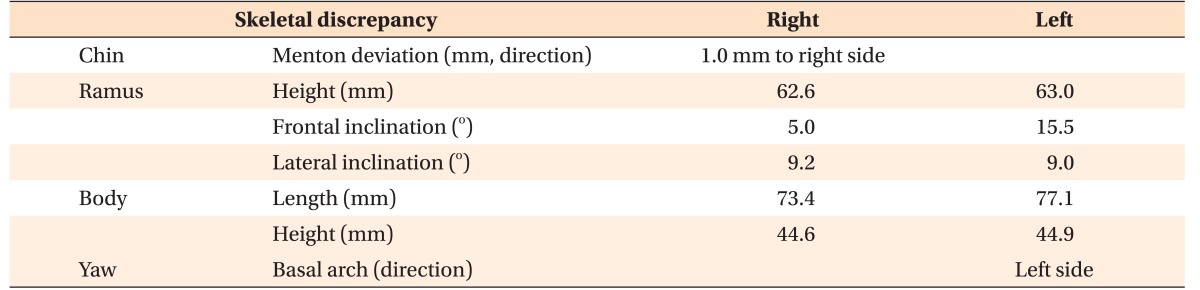
Table 1
Skeletal measurements for mandibular asymmetry in a patient (Case 1) with a yawing-dominant type asymmetry
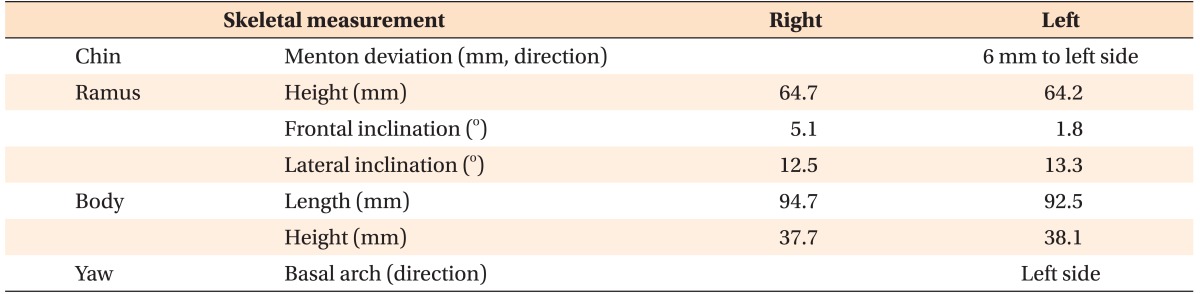
Table 2
Lateral cephalographic analysis in a patient (Case 1) with a yawing-dominant type asymmetry
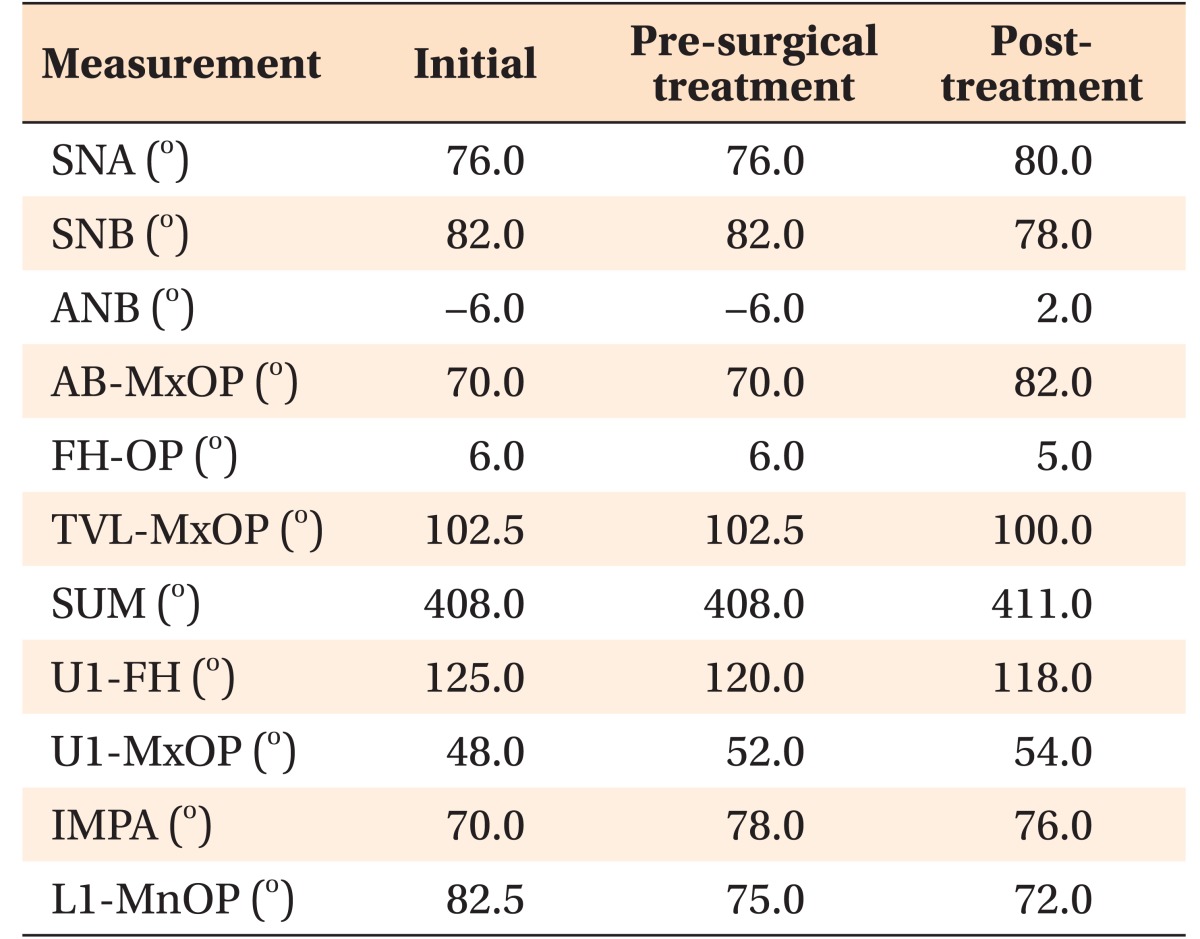
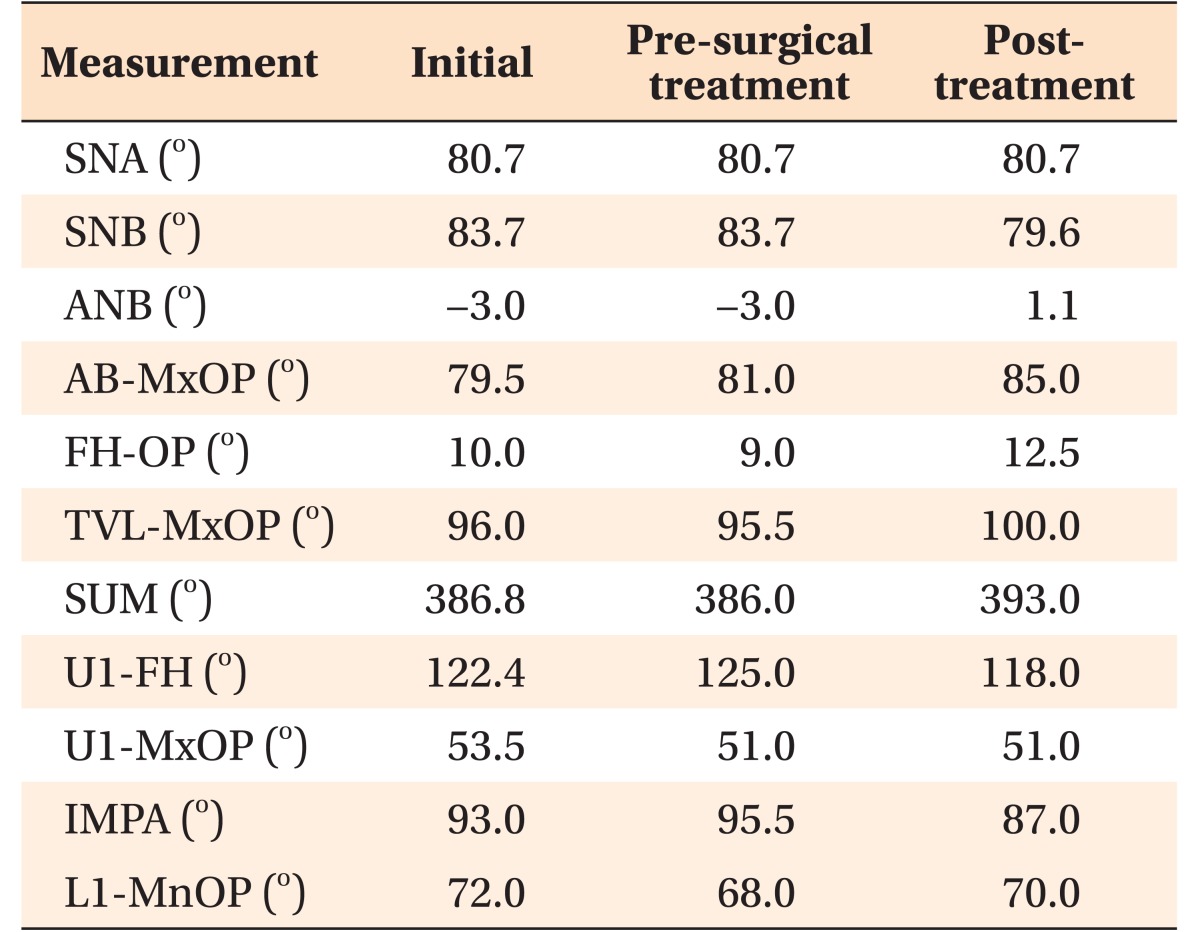
Table 3
Skeletal measurements for mandibular asymmetry in a patient (Case 2) with an atypical type asymmetry
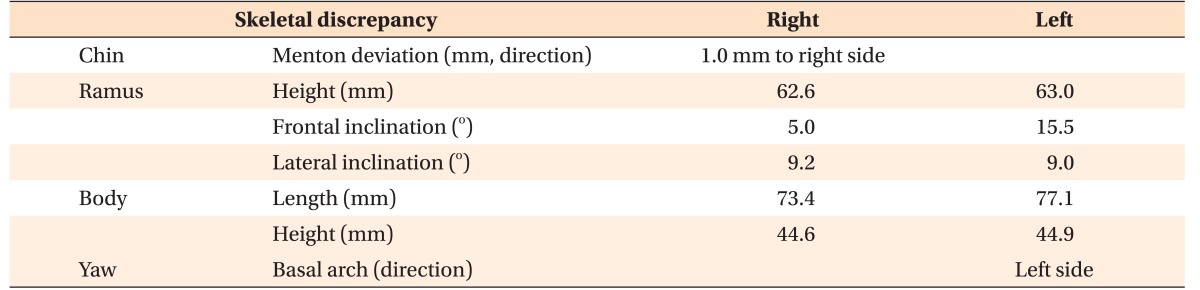
Table 4
Lateral cephalographic analysis in a patient (Case 2) with an atypical type asymmetry





 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download