Abstract
Objective
To determine the physical activity (PA) behavior, needs and preferences for underserved, ethnically diverse women with a history of endometrial cancer (EC).
Methods
Women with a history of EC (41 non-Hispanic black, 40 non-Hispanic white, and 18 Hispanic) completed a needs assessment during their regular follow-up appointments at Montefiore Medical Center in Bronx, NY, USA. An 8-week pilot PA intervention based on the results of the needs assessment was conducted with 5 EC survivors.
Results
Mean body mass index (BMI) among the 99 respondents was 34.1±7.6 kg/m2, and 66% did not exercise regularly. Self-described weight status was significantly lower than actual BMI category (p<0.001). Of the 86% who were interested in joining an exercise program, 95% were willing to attend at least once weekly. The primary motivations were improving health, losing weight, and feeling better physically. Despite the high interest in participation, volunteer rate was very low (8%). However, adherence to the 8-week pilot PA intervention was high (83%), and there were no adverse events. Body weight decreased in all pilot participants.
Abdominal obesity and physical inactivity are primary risk factors for endometrial cancer [1]. Although a cancer diagnosis is often thought of as a "teachable moment," cross-sectional investigations have found that less than 35% of endometrial cancer survivors achieved the American College of Sports Medicine (ACSM) guidelines for physical activity [2] and that up to 50% were obese [3]. Endometrial cancer survivors are the least physically active out of all cancer survivor groups, with only up to 33% being regularly active, compared to 45% for all cancer survivors, and 53% for respondents without a history of cancer [4]. Although the rate of survival from endometrial cancer may be as high as 96%, survivors are likely to have the risk factors for metabolic syndrome [5] and be physically inactive, greatly increasing their risk of developing other related diseases such as cardiovascular disease, diabetes, and osteoarthritis, leading to greater risk of morbidity and mortality [5]. Quality-of-life and fatigue outcomes were significantly better in endometrial cancer survivors who achieved ACSM physical activity guidelines or had normal body mass index (BMI) in cross-sectional studies [6,7]. Furthermore, obesity may be associated with higher all-cause mortality among endometrial cancer survivors [8].
The impact of obesity and physical inactivity may be more pronounced among Latina and black endometrial cancer survivors, because they are approximately 50% more likely to be obese than white endometrial cancer survivors [9]. Because physical inactivity and the metabolic syndrome increase the risk for developing cardiovascular disease, diabetes, osteoarthritis, and endometrial cancer recurrence [10], underserved, ethnically diverse endometrial cancer survivors likely have a greater disease risk compared with white women. More research is needed to determine the health behavior practices and attitudes of underserved, ethnically diverse endometrial cancer survivors in order to develop effective evidence-based physical activity interventions.
Physical inactivity is a major risk factor for developing endometrial cancer [11], and most survivors maintain their inactive lifestyles, thereby further increasing their morbidity. Therefore, it is imperative that effective interventions be developed to increase physical activity in this group [12]. However, there is currently a paucity of data examining best practices for achieving these results among endometrial cancer survivors. This is particularly true for survivors from under-represented groups, who have an increased risk of endometrial cancer and related chronic diseases (cardiovascular disease, type 2 diabetes mellitus, etc.).
The aims of this study were: (1) to identify the prevalence and patterns of physical activity behavior of ethnically diverse endometrial cancer survivors; (2) to determine the physical activity programming preferences of the sample so that a culturally-tailored physical intervention could be developed; and (3) develop a pilot physical activity intervention based on the findings from the preliminary needs analysis (aims 1 and 2).
After Institutional Review Board approval, English or Spanish-speaking women with a history of endometrial cancer who were treated at Montefiore Medical Center from May to August 2010 were invited to complete a 10-minute confidential questionnaire in the doctor's office or over the phone at a more convenient time. The study was continued until 99 consecutive surveys had been completed.
A pilot 8-week physical activity intervention was developed from data collected from the needs assessment. Recruitment was limited to endometrial cancer survivors who spoke either English or Spanish and had either opted into a physical activity interest list maintained by the oncologists at Albert Einstein College of Medicine or had previously participated in one of the Bronx Oncology Living Daily fitness/nutrition programs. All participants received clearance to participate in the moderate-intensity physical activity program from their primary care provider.
Demographic information was collected via self-report. Medical information, including height and weight for the calculation of BMI, was collected from patient medical records. An 18-item questionnaire, available in English and Spanish, containing questions regarding exercise, diet, and smoking behaviors, was administered by in person or over the phone. Behavior change readiness and barrier self-efficacy were assessed using a survey adapted from Marcus et al. [13], which has shown test-retest reliability of rs=0.78 [14], and has been validated for use with African-American adults [15]. Self-assessment of weight was assessed using a question from the Body Satisfaction Scale from Berscheid et al. [16], which has been show to be a reliable (Cronbach's α=0.90 for body image) and valid (r=-0.63) measure of body image in a racially diverse sample [17]. A question regarding reasons for wanting to participate in physical activity was adapted from a survey by Smith for cancer survivors [18]. The remaining questions about the (1) types of exercise performed regularly, (2) preferred exercise programming, and (3) acceptable time commitment, were developed by the authors for this study.
The goals of the 8-week pilot Physical Activity Intervention were to provide fitness instruction, while developing safe and appropriate exercises for middle-aged and older cancer survivors in the Bronx, and assess their relative level of adherence. The 8 consecutive weeks ran from mid-September to the mid-November. Classes were held once per week at the university recreation complex at a time and day that was determined based on input from the participants. Each 1-hour class included a warm-up, cardiovascular and resistance training with elastic bands, a cool-down and stretching. The exercise routine and musical playlist were modified weekly based on explicit participant feedback and subjective instructor assessment. Each exercise was instructed with options for increased or decreased intensity to maximize individualization of the workouts. The windows of the exercise room were blocked using fabric sheets in order to maintain privacy for the participants.
Height, weight and blood pressure measurements were taken prior to the exercise session during the 4th and 8th (last) weeks. Height was self-reported. Weight was measured using a Detecto Mechanical Weigh Beam Scale (Webb City, MO, USA). A physician who was not the primary care provider assessed seated resting blood pressure manually using an aneroid sphygmomanometer.
Data were input into SPSS ver. 22.0 (IBM Co., Armonk, NY, USA) for all analyses. Descriptive statistics were used to assess means and standard deviations, as well as frequencies and percentages for categorical data. A related-samples Wilcoxon Signed-Rank test was analyzed to assess differences in real and perceived body composition. Kruskal-Wallis and one-way analysis of variance (ANOVA) were used to determine differences between races/ethnicities for categorical demographic information and exercise preferences. One-way ANOVA were analyzed to determine difference between races/ethnicities for continuous data. Shapiro-Wilk tests were analyzed for normality and Levene statistics were analyzed to determine homogeneity of variances between groups.
Descriptive characteristics of the 99 women with history of endometrial cancer from the preliminary assessment are reported in Table 1. In brief, the mean±SD age of the participants was 64.4±10.1 years, time from diagnosis was 85.2±76.8 months (interquartile range, 9.6 to 57.9 months), and BMI was 34.1±7.6 kg/m2. There were no differences in age, time from diagnosis or BMI between ethnicities (p>0.20) (Table 1). In this sample, 41% self-identified as non-Hispanic black, 40% self-identified as non-Hispanic white, and 18% identified as Hispanic. Sixty-nine percent were raised in the United States; 24% were raised in Caribbean nations. Sixty-two percent of the respondents had graduated from high school or less, and 25% had graduated from college or more. There was a significant difference among ethnicities for education level (chi-square=6.65, p=0.036). Mann-Whitney tests, with Bonferroni adjustments, revealed that Hispanics had significantly lower educational level than non-Hispanic black women (p=0.009) and non-significantly lower education level than non-Hispanic white women (p=0.079). Fifty-nine participants had been diagnosed with hypertension, 42 with hypercholesterolemia, and 33 with type 2 diabetes mellitus. Twenty-six participants had two of the preceding conditions and another 18 had all three conditions.
Based on BMI classifications, 17% were overweight and 73% were obese, including 44% with BMI of 35 or higher. In comparison, when asked to describe their own weight status, 25% reported that they were "average or underweight," 29% indicated that they were only "slightly overweight," and 46% indicated they were "very overweight." There was a significant difference between respondents' self-reported weight status and actual BMI classification (p<0.001), with an average underestimation of almost one-second of a BMI classification.
More than half of participants (55%) were in either the contemplation or preparation stages of exercise behavior change (Table 2), and there were no significant difference between ethnic groups (p>0.20). Participants were very confident that they could overcome being in a bad mood to participate in an exercise program (65%), but progressively less confident about overcoming lack of time (49%), poor weather (48%), being on vacation (40%), and being tired (38%) (Table 3).
Walking was overwhelmingly the top choice (54%) when participants were asked which types of vigorous exercise they typically performed. The only other answers to generate more than 10% response were aerobic classes (13%), biking (12%), and weight training (10%). Swimming, dancing, yoga, running and gardening were all mentioned by less than 5% of the respondents. Only 16% of the respondents reported belonging to a gym or fitness club. Two-thirds did not exercise regularly post diagnosis.
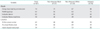
If a physical activity, or physical activity plus nutrition, program were offered at the Montefiore Einstein Center for Cancer Care, 66% indicated they would definitely be interested and another 20% said they might be interested. Of the 13 participants who provided reasons for not being likely to participate, the explanations were either living too far away (n=8) or not having enough time (n=5). When asked which kind of exercise program they would prefer, respondents responded the most to group classes lead by an instructor, but were also highly receptive to several other options as well (Table 4). Participants also reported a willingness to attend frequent sessions of an exercise program: 28% responded that they would attend once per week and 67% would attend 2 to 3 sessions per week. When asked about primary reasons for wanting to participate in an exercise program, improving overall health (48%), losing weight (26%), and feeling better physically (21%) were the most common responses. Available responses that received the least responses were improving stamina (3%), reducing recurrence (4%), being doctor recommended (4%), and feeling better emotionally (5%).
Sixty-six endometrial cancer survivors who had expressed interest in possibly participating in a physical activity program were asked to join the physical activity pilot program, which was offered once per week on a weekday morning for 8 weeks. Seventeen endometrial cancer survivors (26%) verbally agreed to participate, but only five actually attended a class. The primary stated reasons for non-participation among volunteers were either inability/unwillingness to obtain physician clearance or that the available class time was inconvenient. Because of the low enrollment, participation was opened to all female cancer survivors, and three non-endometrial cancer patients enrolled.
Five of the eight pilot participants were survivors of endometrial cancer, two were breast cancer survivors, and one had had chordoma. Six women with a history of cancer (four non-Hispanic black, two non-Hispanic white) were able to begin the program on the first day. Two Hispanic cancer survivors joined during the 3rd and 4th weeks; they attended 2 and 1 classes, respectively. Although no compensation other than a pedometer and resistance band was offered, adherence was 83% among the six participants who began the program on the first week, indicating a high level of enthusiasm and commitment in this population once the initial barriers to physical activity have been overcome. There were no adverse events or injuries that precluded continued participation.
Prior to class on the 4th and 8th weeks, respectively, during the period in which the physical activity routine had been mostly stabilized, body weight and blood pressure were assessed. BMI and resting systolic blood pressure at baseline were 34.2±7.6 kg/m2 and 123±10 mmHg, respectively. Body mass decreased by 1.0±0.8 kg (95% confidence interval [CI], -0.3 to 2.3; p=0.10), and each of the participants lost weight (range, 0.1 to 2.2 kg). Systolic blood pressure decreased by 5±10 mmHg (95% CI, -8 to 18; p=0.10).
The major strength of this study is that, to our knowledge, it is the first to assess the exercise behavior and preferences of ethnically diverse women with a history of endometrial cancer. The primary novel findings from this study were: (1) This ethnically diverse sample of endometrial cancer survivors from Bronx, NY had much higher rates of obesity (73%) than previously reported in studies of more educated, primarily Caucasian endometrial cancer survivors, suggesting that this population may have an elevated need for a physical activity intervention to reduce chronic disease risk. (2) Endometrial cancer patients significantly underestimated their weight category pointing to a potential barrier to motivation for behavior change in this urban population. (3) Although the sample reported a strong intention to begin a physical activity program, actual participation in a weekly intervention was very low, indicating that physical activity interventions for ethnically diverse endometrial cancer survivors need to assess and identify significant barriers to exercise to be successfully adopted. (4) The physical activity intervention, which included aerobic and resistance training, was safe and effective for those participants who were able to overcome the initial barriers to exercise.
The findings of this study are different from other exercise programs for endometrial cancer in that the sample population in this study was more ethnically and socioeconomically diverse than previous reports. Only 40% of the sample was non-Hispanic White, compared to 74% to 94% in previous studies [3,7,19]. The sample may not have been representative of the Bronx as a whole, which is 53% Hispanic, 30% non-Hispanic black, and 11% non-Hispanic white, but is representative of the neighborhoods surrounding Albert Einstein College of Medicine, which contain relatively higher percentages of non-Hispanic white and black populations [20]. Education level also indicated a very socioeconomically diverse sample. There was the same percentage of respondents that had graduated from college (25%) as those who had not completed high school. The percentage that not attended any college (62%) was also much higher in this study than in other investigations of endometrial cancer survivors (26% to 48%) [7,19,21]. This ethnically and socioeconomically diverse sample population was also more obese than previous studies of endometrial cancer survivors. In the current study, only 10% of respondents had a BMI <25 and 73% of respondents were obese. In contrast, other cross-sectional surveys of endometrial cancer survivors have found 28% to 29% of respondents with BMI <25 and 38% to 54% obesity [3,6,21,22].
Additionally, there was a significant difference in actual and perceived body composition, with more obese women considering themselves average or slightly overweight. This is consistent with previous studies showing that women regularly under-assess their body composition, particularly among Hispanic [23] and non-Hispanic black [24], older, and low socioeconomic subpopulations [25], which is similar to the sample of this study. It has been well established that non-Hispanic black women tend to believe that women can be attractive and healthy at overweight or obese body compositions [23] compared to non-Hispanic white women. Since the rates of obesity are high in the Bronx, and even higher in the communities surrounding the location of the study [20], women may underestimate their body composition because of social comparison processes. Since weight misperception is associated with reduced likelihood of following a physical activity/diet intervention [26], future interventions for these groups should focus in part on correcting misperceptions regarding the weight-health correlation.
These findings point to the fact that endometrial cancer survivors from the Bronx are more ethnically diverse, less educated and more obese than those assessed in previous studies of endometrial cancer survivors, and thus offer a unique perspective of the lifestyle intervention needs of an underserved and high-risk cancer patient population. The only other study of endometrial cancer survivor exercise preferences, conducted by Karvinen et al. [21], found that 42% of participants would definitely be interested in an exercise program, and another 35% might be interested. The current study found that 66% would definitely be interested and another 20% possibly interested, indicating that the population sampled in this study perceived themselves to be more ready to engage in a physical activity program. Furthermore, two-thirds of the study participants indicated an interest in attending at least two physical activity sessions per week.
Based on the findings from the preliminary assessment, a pilot physical activity intervention was developed and implemented to determine which exercises where tolerable and those that stimulated enthusiasm. To illustrate the adaptive nature of the program, hula hooping was initially included as a warm-up exercise in order to mobilize the hips and boost morale. However, none of the participants could actually perform the exercise, leading to frustration and a temporary break in movement, so the hula-hoop was used as a prop on the floor for aerobic training. The playlist of songs was developed to cover both contemporary and more classic up-tempo songs that would engage and motivate the participants. Some samples were "I'm not afraid" by Jill Scott, an African-American singer, and "La Guagua" by the late Hispanic singer, Celia Cruz. Participants also submitted requests that were then added to the playlist. Adherence to the 8-week pilot intervention among those that attended the first class was 83%, which is higher than was reported (73%) during a less vigorous behavioral intervention for more educated, mostly non-Hispanic white endometrial cancer survivors [27]. This is also similar to the adherence reported in another group exercise pilot conducted with breast cancer survivors [28].
While respondents to the needs assessment reported high self-efficacy regarding common barriers to exercise, and strong interest in devoting a significant amount of time to a physical activity program, only five of the 66 endometrial cancer survivors who had expressed interest in a physical activity program evaluation actually attended class, indicating a significant discord between expressed and realized interest in participating in a physical activity program. The primary stated reasons for non-participation were inability or unwillingness to obtain physician clearance and inconvenience of the chosen class time. Great care should be taken in future studies to maximize the appeal while lowering the burden of physical activity programs to ethnically diverse cancer survivors because recruitment was low but adherence was high. Future interventions should offer multiple classes each week so that participants will have a choice of days and times to attend class. Facilitative incentives such as transportation remuneration, group-branded workout gear and accessories, and gift cards to local sporting goods stores should be used to increase motivation and lower the burden of participation.
The data from the pedometers were not used because they were compromised by participant interaction with the devices. Although the pedometers were set up to assess daily and weekly walking habits, and participants were instructed to leave the pedometers closed, participants regularly opened the devices and toggled through the various modes, even resetting the data occasionally. Future studies should utilize either pedometers that are not accessible (i.e., taped shut) or accelerometer models that cannot be modified by the user.
These findings suggest that ethnically diverse endometrial cancer survivors are different in several ways relative to previously studied samples, and may have unique needs and challenges regarding physical activity interventions including higher BMI. Physical activity interventions for these groups that are based on assessments of the needs and preferences of the population for which they will be administered are feasible, provided they are convenient. Although the pilot study showed promising outcomes, a more robust scientific study of the feasibility and effectiveness of such a program should be conducted.
Figures and Tables
Table 1
Participant characteristics
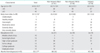
Table 2
Stages of change
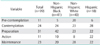
Table 3
The degree of confidence to participate in a regular exercise program according to the situation
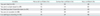
Table 4
What kind of exercise program would you prefer?
ACKNOWLEDGMENTS
This research was supported in part by the Entertainment Industry Foundation and the New Yankee Stadium Community Benefits Fund, Inc.
References
1. Lee I, Oguma Y. Physical activity. In : Schottenfeld D, Fraumeni JF, editors. Cancer epidemiology and prevention. 3rd ed. New York: Oxford University Press;2006.
2. Garber CE, Blissmer B, Deschenes MR, Franklin BA, Lamonte MJ, Lee IM, et al. American College of Sports Medicine position stand. Quantity and quality of exercise for developing and maintaining cardiorespiratory, musculoskeletal, and neuromotor fitness in apparently healthy adults: guidance for prescribing exercise. Med Sci Sports Exerc. 2011; 43:1334–1359.
3. Basen-Engquist K, Scruggs S, Jhingran A, Bodurka DC, Lu K, Ramondetta L, et al. Physical activity and obesity in endometrial cancer survivors: associations with pain, fatigue, and physical functioning. Am J Obstet Gynecol. 2009; 200:288.e1–288.e8.
4. Mayer DK, Terrin NC, Menon U, Kreps GL, McCance K, Parsons SK, et al. Health behaviors in cancer survivors. Oncol Nurs Forum. 2007; 34:643–651.
5. von Gruenigen VE, Waggoner SE, Frasure HE, Kavanagh MB, Janata JW, Rose PG, et al. Lifestyle challenges in endometrial cancer survivorship. Obstet Gynecol. 2011; 117:93–100.
6. Courneya KS, Karvinen KH, Campbell KL, Pearcey RG, Dundas G, Capstick V, et al. Associations among exercise, body weight, and quality of life in a population-based sample of endometrial cancer survivors. Gynecol Oncol. 2005; 97:422–430.
7. Fader AN, Frasure HE, Gil KM, Berger NA, von Gruenigen VE. Quality of life in endometrial cancer survivors: what does obesity have to do with it? Obstet Gynecol Int. 2011; 2011:308609.
8. Arem H, Irwin ML. Obesity and endometrial cancer survival: a systematic review. Int J Obes (Lond). 2013; 37:634–639.
9. Setiawan VW, Pike MC, Kolonel LN, Nomura AM, Goodman MT, Henderson BE. Racial/ethnic differences in endometrial cancer risk: the multiethnic cohort study. Am J Epidemiol. 2007; 165:262–270.
10. Rosato V, Zucchetto A, Bosetti C, Dal Maso L, Montella M, Pelucchi C, et al. Metabolic syndrome and endometrial cancer risk. Ann Oncol. 2011; 22:884–889.
11. Voskuil DW, Monninkhof EM, Elias SG, Vlems FA, van Leeuwen FE. Physical activity and endometrial cancer risk, a systematic review of current evidence. Cancer Epidemiol Biomarkers Prev. 2007; 16:639–648.
12. Kwon S, Hou N, Wang M. Comparison of physical activity levels between cancer survivors and non-cancer participants in the 2009 BRFSS. J Cancer Surviv. 2012; 6:54–62.
13. Marcus BH, Selby VC, Niaura RS, Rossi JS. Self-efficacy and the stages of exercise behavior change. Res Q Exerc Sport. 1992; 63:60–66.
14. Marcus BH, Simkin LR. The stages of exercise behavior. J Sports Med Phys Fitness. 1993; 33:83–88.
15. Blaney CL, Robbins ML, Paiva AL, Redding CA, Rossi JS, Blissmer B, et al. Validation of the measures of the transtheoretical model for exercise in an adult African-American sample. Am J Health Promot. 2012; 26:317–326.
16. Berscheid E, Walster E, Bohrnstedt G. The happy American body: a survey report. Psychol Today. 1973; 7:119–131.
17. Petrie TA, Tripp MM, Harvey P. Factorial and construct validity of the body parts satisfaction scale-revised: an examination of minority and nonminority women. Psychol Women Q. 2002; 26:213–221.
18. Smith SL. Physical exercise as an oncology nursing intervention to enhance quality of life. Oncol Nurs Forum. 1996; 23:771–778.
19. Arem H, Irwin ML, Zhou Y, Lu L, Risch H, Yu H. Physical activity and endometrial cancer in a population-based case-control study. Cancer Causes Control. 2011; 22:219–226.
20. US Census Bureau. American Community Survey selected population tables, 2007-2011. Suitland: US Census Bureau;2011.
21. Karvinen KH, Courneya KS, Campbell KL, Pearcey RG, Dundas G, Capstick V, et al. Exercise preferences of endometrial cancer survivors: a population-based study. Cancer Nurs. 2006; 29:259–265.
22. Beesley VL, Eakin EG, Janda M, Battistutta D. Gynecological cancer survivors' health behaviors and their associations with quality of life. Cancer Causes Control. 2008; 19:775–782.
23. Giardina EG, Sciacca RR, Flink LE, Bier ML, Paul TK, Moise N. Cardiovascular disease knowledge and weight perception among Hispanic and non-Hispanic white women. J Womens Health (Larchmt). 2013; 22:1009–1015.
24. Dorsey RR, Eberhardt MS, Ogden CL. Racial/ethnic differences in weight perception. Obesity (Silver Spring). 2009; 17:790–795.
25. Kuchler F, Variyam JN. Mistakes were made: misperception as a barrier to reducing overweight. Int J Obes Relat Metab Disord. 2003; 27:856–861.
26. Duncan DT, Wolin KY, Scharoun-Lee M, Ding EL, Warner ET, Bennett GG. Does perception equal reality? Weight misperception in relation to weight-related attitudes and behaviors among overweight and obese US adults. Int J Behav Nutr Phys Act. 2011; 8:20.
27. von Gruenigen VE, Courneya KS, Gibbons HE, Kavanagh MB, Waggoner SE, Lerner E. Feasibility and effectiveness of a lifestyle intervention program in obese endometrial cancer patients: a randomized trial. Gynecol Oncol. 2008; 109:19–26.
28. Kolden GG, Strauman TJ, Ward A, Kuta J, Woods TE, Schneider KL, et al. A pilot study of group exercise training (GET) for women with primary breast cancer: feasibility and health benefits. Psychooncology. 2002; 11:447–456.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download