Abstract
Objective
To determine risk factors associated with recurrence in patients with high intermediate risk (HIR) endometrioid adenocarcinoma.
Methods
A retrospective analysis of patients with HIR endometrioid adenocarcinoma who underwent hysterectomy, bilateral salpingo-oophorectomy, with or without pelvic/para-aortic lymphadenectomy at the University of Pennsylvania between 1990 and 2009 was performed.
Results
A total of 103 women with HIR endometrial cancer were identified. Multivariable analysis revealed that ≥2/3 myometrial invasion (HR, 4.79; p=0.010) and grade 3 disease (HR, 3.04; p=0.045) were independently predictive of distant metastases. The 5-year distant metastases free survival (DMFS) for patients with neither or one of these risk factors was 89%, and the 5-year DMFS for patients with both risk factors was 48% (p<0.001).
Endometrial cancer is the most common gynecological malignancy in the United States with an estimated 43,470 new cases and 7,950 deaths expected to occur in 2010 [1]. Amongst all types of endometrial adenocarcinoma, endometrioid type is the most common, and has the most favorable prognosis [2,3]. Recent studies have determined that the presence of certain factors amongst patients with uterine confined disease, notably increasing age, deep myometrial invasion, tumor grade, presence of lymphovascular space invasion (LVSI), and stage were predictive of a higher risk of recurrence and poorer outcome [3-8]. Thus it became evident that there existed a high intermediate risk (HIR) patient population that may stand to benefit from more aggressive therapy. Though criteria for determination of a HIR endometrial adenocarcinoma subgroup has varied depending on the study, the Gynecologic Oncology Group (GOG) identified a HIR subgroup based on surgicopathologic factors and age [7,8]. Since the publication of GOG 99, the risk stratification algorithm has been increasingly used to guide the adjuvant therapy for patients with intermediate risk endometrial adenocarcinoma in the United States, and is currently the selection criteria for a phase III clinical trial comparing pelvic radiation versus vaginal brachytherapy (VBT) with chemotherapy as adjuvant therapy after surgical staging [9-11]. The objective of this study was to assess the recurrence rates and long term outcomes of patients with HIR endometrioid adenocarcinoma treated at the University of Pennsylvania.
This retrospective study was approved by the University of Pennsylvania Institutional Review Board. Out of the 383 patients with histologically confirmed stage I-II (occult) endometrioid adenocarcinoma that were operated on between 1990 and 2009, 103 patients were found to have HIR disease and were selected for this analysis. HIR disease was defined as per GOG 99. Surgicopathologic risk factors were: grade 2 or 3, outer one-third myometrial invasion, LVSI, and age. HIR was defined as: 1) at least 70 years of age with one risk factor, 2) at least 50 years of age with two risk factors, and 3) any age with all three of the other risk factors.
All patients were initially managed with total hysterectomy and bilateral salpingo-oophorectomy with or without pelvic/para-aortic (PA) lymph node (LN) dissection with or without adjuvant radiation within the University of Pennsylvania Health System. A total of 24 patients underwent pelvic lymphadenectomy, 55 underwent pelvic and PA lymphadenectomy, and 4 patients had only PA LNs sampled. Twenty patients had no LN sampling. Seventy five (73%) patients received adjuvant radiation. Twenty two (21%) patients received only pelvic external beam radiotherapy (EBRT), 22 (21%) received EBRT followed by VBT, and 30 (29%) received only VBT. For the patients who received EBRT with or without VBT, forty three patients were simulated using computed tomography and 1 patient with orthogonal imaging. Five patients were treated using intensity modulated radiation therapy (IMRT) and the remaining patients were treated using a four-field technique.
A total of 53 patients received VBT with or without EBRT. All patients were simulated using either CT or magnetic resonance imaging. Forty six patients received high dose rate (HDR) VBT and 7 patients received low dose rate (LDR) VBT. The most common fractionation scheme used for HDR brachytherapy was 21 Gy given in 3 fractions (24 patients) prescribed to a depth of 0.5 cm. The median active length (distance between the most proximal and most distal end of the active dwell positions) was 4.0 cm (range, 3.5 to 7.0 cm). No patients received chemotherapy as part of their initial treatment.
After completion of their treatment, patients were followed by their radiation and/or gynecologic oncologist at regular intervals. Follow-up data was complete as of May 2011. A locoregional recurrence was defined as a vaginal or pelvic relapse. Overall survival was defined as time from date of surgery to death from any cause. Relapse free survival was defined as the time from date of surgery to disease recurrence or death from any cause, whichever occurred first or to date of last contact for those patients alive without recurrence. Loco-regional recurrence free survival (LRFS) and distant metastasis free survival (DMFS) were defined as time from surgery to either locoregional or distant recurrence, respectively; patients were censored at time of relapse, death without recurrence, or last follow-up.
Acute and late treatment related side effects were graded according to the Common Toxicity Criteria for Adverse Events (CTCAE) ver. 4.02. Acute toxicity was defined as any adverse event that occurred within 90 days since the initiation of adjuvant treatment and late toxicity was defined as any adverse event that occurred beyond 90 days from the initiation of adjuvant treatment.
The log rank test and Cox regression were used to assess for significant associations between local and distant metastases with patient and tumor related prognostic factors. Factors found to be significant on univariate analysis were entered into the Cox proportional multivariable model. A p<0.05 was considered significant. The Kaplan-Meier method was utilized to estimate survival outcomes. The statistical software used was Stata ver. 11 (StataCorp LP, College Station, TX, USA).
The patient demographics and pathologic characteristics are outlined in Table 1. The median patient age was 67 years (range, 25 to 88 years); the median number of pelvic and PA LN removed was 7 (range, 0 to 47) and 3 (range, 0 to 27), respectively. Patients were restaged based on the 2010 FIGO staging criteria [12]. The median follow-up time was 47 months (range, 1.8 months to 18 years).
The 5-year Kaplan Meier overall and relapse free survival were 79% and 71%, respectively. The median time to local recurrence was 6 months (range, 3 to 10 months), and the median time to distant metastasis was 24 months (range, 8 months to 9.4 years). The 5-year LRFS and DMFS rates were 97% and 81%, respectively. Overall, there were a total of 17 (17%) disease recurrences; twelve (12%) patients died of endometrioid adenocarcinoma. Initial local recurrences occurred in 2 (2%) patients. Sixteen patients had initial distant metastases. The sites of distant metastases were: lung (10), peritoneum (4), liver (6), brain (2), bone (1), adrenal gland (1), and LNs (axillary, 1), mediastinal (1), and PA (2). Five patients had metastases to multiple sites. Table 2 summarizes the original treatments, recurrence sites, treatments for recurrence, and ultimate outcomes for the 17 patients who recurred.
Twenty eight (27%) patients received no adjuvant treatment and two recurred. One had an isolated vaginal recurrence and the other suffered distant metastasis to the lung. Both patients underwent treatment for relapse, and both ultimately died of disease.
Twenty two (21%) patients received only pelvic radiation and 4 recurred. Two patients experienced isolated recurrences to the PA nodes in previously untreated regions and the other two patients experienced only distant metastases. With respect to the two patients who experienced PA recurrences, one patient did not undergo a PA dissection while the other had three PA LNs removed. The two patients with PA node recurrences underwent successful treatment for relapse. The third patient with a distant metastasis to the liver failed her relapse treatment and died of disease; the fourth patient with metastases to the brain, lung, and liver was treated with whole brain radiation therapy and ultimately died of disease.
Thirty one (30%) patients received only VBT and 3 recurred. One patient had distant metastases only, one patient had a recurrence in the sigmoid colon followed by a second distant relapse, and the third had an isolated vaginal recurrence. The third patient with the isolated vaginal recurrence received 35 Gy out of the planned 60-65 Gy of low dose rate VBT; treatment was discontinued at the patient's request due to grade 2 diarrhea and the patient's history of irritable bowel syndrome. She underwent surgical excision, received Megace and is alive with disease.
Twenty two (21%) patients received both pelvic radiation and VBT and 8 recurred. All had only distant metastases. Seven patients underwent treatment for their relapses. Two patients, whose disease spread to a single site, underwent successful therapy. The remaining 4 patients, whose disease spread to multiple sites, died of disease despite therapy. There were no differences in the rates of locoregional recurrence or distant metastasis based on radiation modality (pelvic radiation, VBT, or observation) or whether they underwent a LN dissection.
Several patient and histopathological factors were analyzed in our study population. Age and number of LNs removed were treated as continuous variables, and the other factors were treated as dichotomous variables. Adjuvant radiation was dichotomized to either the administration versus no administration of adjuvant radiation. Myometrial depth was dichotomized to either <2/3 invasion versus >2/3 invasion, and tumor grade was dichotomized to grades 1-2 versus grade 3. No factors were associated with local recurrence in our study population, but deep myometrial invasion (p=0.008), grade 3 histology (p=0.023), number of pelvic LNs removed, (p=0.023), and cervical glandular invasion (p=0.049) were significantly associated with an increased risk of distant metastases on univariate analysis. LVSI (p=0.23) and age (p=0.84) were not significantly associated with an increased risk of distant metastases (Table 3). On multivariable analysis, grade 3 (p=0.045; HR, 3.04; 95% CI, 1.02 to 9.04) and deep third myometrial invasion (p=0.010; HR, 4.79; 95% CI, 1.45 to 15.84) were predictive of distant metastases (Table 4). The largest impact on the hazard ratio was obtained by dichotomizing the variables: grade 3 vs. grade 1 or 2 and myometrial invasion as greater than or less than 2/3 invasion of the myometrium. DMFS was not significantly different for women with grade 1 and 2 disease. The presence of both risk factors (grade 3 disease and deep third myometrial invasion) conveyed a significantly higher risk of distant metastases than the presence of either one alone. There was no significant difference in DMFS amongst patients with either grade 3 or deep third myometrial invasion and those with neither risk factor. The 5-year DMFS for patients with one or neither risk factor was 89% and the 5-year DMFS for patients with both risk factors was 48% (p<0.001) as illustrated in Fig. 1. Of the 19 patients with both deep myometrial invasion and grade 3 disease, 14 underwent LN dissection vs. 5 patients that had no LN dissection. Nine patients (64%) with LN dissection relapsed (1 local, 8 distant) vs. one relapse (20%) in a patient without LN sampling (distant), p=0.13.
In our study population, the median total dose was 50.4 Gy (range, 41.4 to 50.4 Gy in 23 to 28 fractions), and the median energy of the photon beam was 15 MV (range, 10 to 23 MV). One patient received only 41.4 Gy out of a planned total dose of 45 Gy due to severe diarrhea. One patient with a history of irritable bowel syndrome who received LDR brachytherapy received only 35 Gy out of the planned 60-65 Gy due to severe diarrhea. The rates of any acute and late symptomatic (grade 2) toxicities were: 26% and 18%, respectively. The rates of acute and late severe (grade 3) toxicities were: 2% and 4%, respectively (one patient had grade 3 diarrhea during treatment which resolved within 90 days, one patient had grade 3 cystitis during treatment which resolved within 90 days, and 4 patients who received external beam radiotherapy had a small bowel obstruction requiring surgery).
In this single institutional retrospective analysis, we investigated the patterns of relapse and risk factors for recurrence amongst patients considered to have HIR endometrioid adenocarcinoma as defined by GOG 99 treated with either adjuvant pelvic radiation +/- VBT, VBT alone, or observation. On multivariable analysis, grade 3 disease and deep third myometrial invasion were the most important predictors of distant metastasis amongst this high risk group. Additionally, patients with both pathologic risk factors had a higher rate of distant metastasis compared to those that had neither or just one risk factors with 5-year DMFS 89% vs. 48%, p<0.001.
Our results are consistent with that reported in other studies. Several publications have suggested that the incidence of distant metastasis in early stage endometrial adenocarcinoma ranges between 4-12% [7,13-21]. Several prognostic factors have been analyzed for correlations with distant metastasis, and the most commonly reported risk factors for distant metastasis in this HIR group are: LVSI, deep myometrial invasion, and grade 3 histology [7,15,22-26]. For the subset of patients with IC grade 3 disease who all received pelvic radiotherapy in the Post Operative Radiation Therapy in Endometrial Carcinoma (PORTEC) study reported by Creutzberg et al. [22], rate of distant metastases was 31% at 5 years. The 5-year DMFS in this analysis was 48% for patients with both outer one third myometrial invasion and grade 3 disease. Grade 3 disease has consistently been identified in prior studies as a risk factor for extrapelvic recurrences. In a multi-institutional analysis of patterns of relapse amongst patients with stage I, grade 3 disease, 81% of patients who developed an extrapelvic recurrence died of their disease [16]. A retrospective analysis of stage IC patients by Long et al. [27], found that patients with grade 3 disease were at significantly increased risk of recurrence (28.9%) with all recurrences containing a distant component and the majority being fatal. Additionally, amongst patients that have an isolated vaginal relapse, grade 3 disease is a poor prognostic factor. All patients with grade 3 disease died within four years of their relapse in a retrospective study by Lin et al. [28]. We did not find LVSI to be significant in our analysis, but 16 patients lacked information with regard to LVSI, and thus the lack of significance maybe related to the limited patient numbers.
The use of adjuvant radiotherapy in this group was varied ranging from none to pelvic and/or vaginal brachytherapy; no patients received chemotherapy. Rates of local recurrence were low in this analysis and are consistent with reported rates of loco-regional failure in patients who have been treated with radiotherapy. Type of radiotherapy used had no impact on risk of distant metastases or survival. The majority of patients (17/22) in this analysis with IC grade 3 disease received pelvic radiotherapy +/- VBT. It is difficult, therefore, to comment on whether vaginal brachytherapy alone would have been adequate local treatment in this cohort of patients.
With respect to local disease control, three major randomized studies have demonstrated the benefit to adjuvant pelvic radiation to decrease the risk of locoregional relapse, though there was no significant survival benefit [6,7,17]. However, the rate of adverse gastrointestinal side effects were significantly higher in the pelvic radiation arm in both the PORTEC and GOG 99 study, and both trials found that the majority of the local recurrences occurred at the vaginal vault in the control arms. The recent PORTEC2 study demonstrated that VBT alone can effectively provide local disease control in patients with intermediate risk endometrial adenocarcinoma with less severe side effects when compared to pelvic radiation [29,30]. Patients with IC grade 3 disease, however, were not eligible for this study. Additionally, several single institutional retrospective studies have demonstrated the low risk of subsequent vaginal failures after brachytherapy alone for stage I/II endometrial cancer, particularly if the patient populations underwent surgical staging [31-33]. Adjuvant radiotherapy in this population is justified given the high local control rates. In our analysis, no patient who received initial pelvic external beam radiotherapy had a local relapse. The modality of radiotherapy remains an open question for this high risk population though there is some retrospective data to suggest that vaginal brachytherapy alone in this population may be sufficient local treatment. In one of the largest retrospective series to date that included only high risk patients defined by PORTEC, GOG 99, or Aalders et al. [17], McCloskey et al. [34] observed a 3.4% loco-regional recurrence rate with vaginal brachytherapy alone. As reported in other series, pelvic radiotherapy and/or brachytherapy reduces the risk of pelvic or vaginal recurrences, but does not ultimately impact on the rate of distant recurrence or survival [16,22]. A subgroup of these patients though remains at high risk of distant relapse as this analysis demonstrates and novel strategies to improve survival are needed. As studies have demonstrated, there is no impact on survival with LN dissection, and in patients with grade 1-2 disease, small volume disease, and less than 50% myometrial invasion, the risk of lymph node metastases is very low [35-37]. In our analysis, the risk of relapse (64%) was high despite LN sampling in patients with deep myometrial invasion and grade 3 disease with the majority of relapses occurring in distant areas.
The high rates of extrapelvic recurrences in this group of patients suggests a need for systemic therapy, however, the role of chemotherapy for stage I patients has not yet been defined. It would be rational to hypothesize that chemotherapy may benefit patients with earlier stage HIR disease given the significant rates of distant metastases that have been previously demonstrated by others as well [5,15,16,22,26,38]. This hypothesis was tested in a phase III study by the Japan Gynecologic Oncology Group; whole pelvic radiotherapy was compared to cyclophosphamide, doxorubicin, and cisplatin (CAP) chemotherapy in women with stage I-III endometrial cancer [39]. Though there was no difference overall between the two arms, on subgroup analysis, patients with HIR disease who received chemotherapy had a significantly higher PFS (83.8% vs. 66.2%, p=0.024) and OS (89.75 vs. 73.6%, p=0.006) compared to patients who received radiation therapy. HIR patients were defined as stage IC over 70 years of age, grade 3 endometrioid adenocarcinoma, or stage II/IIIA with >50% myometrial invasion. In a single institutional phase II study by Landrum et al. [40], twenty-three patients with HIR endometrioid cancer or stages I-IIB serous or clear cell carcinoma received 3 fractions of VBT followed by 3 cycles of carboplatin/paclitaxel. At a median follow-up of 12 months, only one recurrence was identified. This approach seems reasonable, but needs to be evaluated with larger patient numbers and longer follow-up.
Currently, GOG 249 is recruiting patients to examine the therapeutic benefit and treatment toxicity profile of VBT with carboplatin/paclitaxel × 3 cycles vs. pelvic radiation in patients with HIR endometrial adenocarcinoma [11]. The findings of this study will elucidate whether systemic therapy is justifiable in patients with early stage endometrioid adenocarcinoma at high risk for distant metastasis. Although we agree with conventional thought that not all HIR patients may benefit from systemic therapy, we believe that a subset of the population with multiple risk factors for distant metastasis may be suitable candidates for adjuvant chemotherapy and in particular those patients with both grade 3 and deep myometrial disease.
Our study has a number of limitations. First, as with any retrospective study, our data may be confounded by selection bias. Second, our study population was relatively small due to our strict selection criteria. Third, only 54% of our study population underwent both pelvic and PA LN dissection, so we cannot exclude the possibility that a proportion of our patients had occult stage III disease. Prospective studies are needed to verify our findings.
In conclusion, our results suggest that patients with grade 3 and deep third myometrial invasion are at high risk of distant relapse. Additional larger cohort studies examining this patient population are warranted to rationally recommend systemic therapy.
Figures and Tables
Fig. 1
Kaplan-Meier curve for distant metastasis free-survival stratified by presence or absence of both grade 3 and deep myometrial invasion.
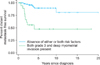
Table 2
Recurrence patterns, treatments, and outcome of the 17 patients that developed recurrence

AWD, alive with disease; DID, died of intercurrent disease; DOD, died of disease; EBRT, external beam radiotherapy; IMRT, intensity modulated radiation therapy; LN, lymph node; NED, no evidence of disease; PA, Para-aortic; RT, radiation therapy; VBT, vaginal brachytherapy; WBRT, whole brain radiation therapy.
*Depth of invasion: 1, inner one-third; 2, middle one-third; 3, outer one-third. †Patient died of second recurrence to the liver, lung, and rib. ‡Died of subsequent distant metastases to liver. §Gastrointestinal. ∥Patient did not complete VBT course.
References
1. National Cancer Institute. Endometrial cancer [Internet]. c2012. cited 2012 Aug 20. Bethesda, MD: National Cancer Institute;Available from: http://www.cancer.gov/cancertopics/types/endometrial.
2. Lee CM, Szabo A, Shrieve DC, Macdonald OK, Tward JD, Skidmore TB, et al. Descriptive nomograms of adjuvant radiotherapy use and patterns of care analysis for stage I and II endometrial adenocarcinoma: a surveillance, epidemiology, and end results population study. Cancer. 2007. 110:2092–2100.
3. Creasman WT, Odicino F, Maisonneuve P, Quinn MA, Beller U, Benedet JL, et al. Carcinoma of the corpus uteri. FIGO 26th Annual Report on the Results of Treatment in Gynecological Cancer. Int J Gynaecol Obstet. 2006. 95:Suppl 1. S105–S143.
4. Kadar N, Malfetano JH, Homesley HD. Determinants of survival of surgically staged patients with endometrial carcinoma histologically confined to the uterus: implications for therapy. Obstet Gynecol. 1992. 80:655–659.
5. Briet JM, Hollema H, Reesink N, Aalders JG, Mourits MJ, ten Hoor KA, et al. Lymphvascular space involvement: an independent prognostic factor in endometrial cancer. Gynecol Oncol. 2005. 96:799–804.
6. Creutzberg CL, van Putten WL, Koper PC, Lybeert ML, Jobsen JJ, Warlam-Rodenhuis CC, et al. Surgery and postoperative radiotherapy versus surgery alone for patients with stage-1 endometrial carcinoma: multicentre randomised trial. PORTEC Study Group. Post Operative Radiation Therapy in Endometrial Carcinoma. Lancet. 2000. 355:1404–1411.
7. Keys HM, Roberts JA, Brunetto VL, Zaino RJ, Spirtos NM, Bloss JD, et al. A phase III trial of surgery with or without adjunctive external pelvic radiation therapy in intermediate risk endometrial adenocarcinoma: a Gynecologic Oncology Group study. Gynecol Oncol. 2004. 92:744–751.
8. Morrow CP, Bundy BN, Kurman RJ, Creasman WT, Heller P, Homesley HD, et al. Relationship between surgical-pathological risk factors and outcome in clinical stage I and II carcinoma of the endometrium: a Gynecologic Oncology Group study. Gynecol Oncol. 1991. 40:55–65.
9. Ioffe Y, Delic L, Amneus M, Leuchter R, Karlan B, Li A, et al. Before and after GOG 99: did our practice patterns for treatment of intermediate risk endometrial adenocarcinoma change? Gynecol Oncol. 2010. 116:595.
10. Rankins NC, Secord AA, Jewell E, Havrilesky LJ, Soper JT, Myers E. Cost-effectiveness of adjuvant radiotherapy in intermediate risk endometrial cancer. Gynecol Oncol. 2007. 106:388–393.
11. McMeekin DS, Randall ME. Pelvic radiation therapy or vaginal implant radiation therapy, paclitaxel, and carboplatin in treating patients with high-risk stage I or stage II endometrial cancer. c2012. Bethesda, MD: National Cancer Institute;ClinicalTrials.gov Id: NCT00807768.
12. Edge SB, Fritz AG, Byrd DR, Greene FL, Campton CC, Trotti A, editors. Cancer staging handbook: from the AJCC cancer staging manual. 2010. 7th ed. Chicago, IL: American Joint Committee on Cancer.
13. Irwin C, Levin W, Fyles A, Pintilie M, Manchul L, Kirkbride P. The role of adjuvant radiotherapy in carcinoma of the endometrium-results in 550 patients with pathologic stage I disease. Gynecol Oncol. 1998. 70:247–254.
14. Rush S, Gal D, Potters L, Bosworth J, Lovecchio J. Pelvic control following external beam radiation for surgical stage I endometrial adenocarcinoma. Int J Radiat Oncol Biol Phys. 1995. 33:851–854.
15. Gadducci A, Cavazzana A, Cosio S, DI Cristofano C, Tana R, Fanucchi A, et al. Lymph-vascular space involvement and outer one-third myometrial invasion are strong predictors of distant haematogeneous failures in patients with stage I-II endometrioid-type endometrial cancer. Anticancer Res. 2009. 29:1715–1720.
16. Rasool N, Fader AN, Seamon L, Neubauer NL, Shahin FA, Alexander HA, et al. Stage I, grade 3 endometrioid adenocarcinoma of the endometrium: an analysis of clinical outcomes and patterns of recurrence. Gynecol Oncol. 2010. 116:10–14.
17. Aalders J, Abeler V, Kolstad P, Onsrud M. Postoperative external irradiation and prognostic parameters in stage I endometrial carcinoma: clinical and histopathologic study of 540 patients. Obstet Gynecol. 1980. 56:419–427.
18. Podczaski E, Kaminski P, Gurski K, MacNeill C, Stryker JA, Singapuri K, et al. Detection and patterns of treatment failure in 300 consecutive cases of "early" endometrial cancer after primary surgery. Gynecol Oncol. 1992. 47:323–327.
19. Reddoch JM, Burke TW, Morris M, Tornos C, Levenback C, Gershenson DM. Surveillance for recurrent endometrial carcinoma: development of a follow-up scheme. Gynecol Oncol. 1995. 59:221–225.
20. DiSaia PJ, Creasman WT, Boronow RC, Blessing JA. Risk factors and recurrent patterns in stage I endometrial cancer. Am J Obstet Gynecol. 1985. 151:1009–1015.
21. Fanning J, Nanavati PJ, Hilgers RD. Surgical staging and high dose rate brachytherapy for endometrial cancer: limiting external radiotherapy to node-positive tumors. Obstet Gynecol. 1996. 87:1041–1044.
22. Creutzberg CL, van Putten WL, Warlam-Rodenhuis CC, van den Bergh AC, de Winter KA, Koper PC, et al. Outcome of high-risk stage IC, grade 3, compared with stage I endometrial carcinoma patients: the Postoperative Radiation Therapy in Endometrial Carcinoma Trial. J Clin Oncol. 2004. 22:1234–1241.
23. Nofech-Mozes S, Ackerman I, Ghorab Z, Ismiil N, Thomas G, Covens A, et al. Lymphovascular invasion is a significant predictor for distant recurrence in patients with early-stage endometrial endometrioid adenocarcinoma. Am J Clin Pathol. 2008. 129:912–917.
24. Creasman WT, Morrow CP, Bundy BN, Homesley HD, Graham JE, Heller PB. Surgical pathologic spread patterns of endometrial cancer: a Gynecologic Oncology Group study. Cancer. 1987. 60:2035–2041.
25. Mariani A, Webb MJ, Keeney GL, Lesnick TG, Podratz KC. Surgical stage I endometrial cancer: predictors of distant failure and death. Gynecol Oncol. 2002. 87:274–280.
26. Greven KM, Randall M, Fanning J, Bahktar M, Duray P, Peters A, et al. Patterns of failure in patients with stage I, grade 3 carcinoma of the endometrium. Int J Radiat Oncol Biol Phys. 1990. 19:529–534.
27. Long KC, Zhou Q, Hensley ML, Alektiar KM, Gomez J, Gardner GJ, et al. Patterns of recurrence in 1988 FIGO stage IC endometrioid endometrial cancer. Gynecol Oncol. 2012. 125:99–102.
28. Lin LL, Grigsby PW, Powell MA, Mutch DG. Definitive radiotherapy in the management of isolated vaginal recurrences of endometrial cancer. Int J Radiat Oncol Biol Phys. 2005. 63:500–504.
29. Nout RA, Smit VT, Putter H, Jurgenliemk-Schulz IM, Jobsen JJ, Lutgens LC, et al. Vaginal brachytherapy versus pelvic external beam radiotherapy for patients with endometrial cancer of high-intermediate risk (PORTEC-2): an open-label, non-inferiority, randomized trial. Lancet. 2010. 375:816–823.
30. Nout RA, Putter H, Jurgenliemk-Schulz IM, Jobsen JJ, Lutgens LC, van der Steen-Banasik EM, et al. Quality of life after pelvic radiotherapy or vaginal brachytherapy for endometrial cancer: first results of the randomized PORTEC-2 trial. J Clin Oncol. 2009. 27:3547–3556.
31. Horowitz NS, Peters WA 3rd, Smith MR, Drescher CW, Atwood M, Mate TP. Adjuvant high dose rate vaginal brachytherapy as treatment of stage I and II endometrial carcinoma. Obstet Gynecol. 2002. 99:235–240.
32. Ng TY, Nicklin JL, Perrin LC, Cheuk R, Crandon AJ. Postoperative vaginal vault brachytherapy for node-negative stage II (occult) endometrial carcinoma. Gynecol Oncol. 2001. 81:193–195.
33. Chadha M, Nanavati PJ, Liu P, Fanning J, Jacobs A. Patterns of failure in endometrial carcinoma stage IB grade 3 and IC patients treated with postoperative vaginal vault brachytherapy. Gynecol Oncol. 1999. 75:103–107.
34. McCloskey SA, Tchabo NE, Malhotra HK, Odunsi K, Rodabaugh K, Singhal P, et al. Adjuvant vaginal brachytherapy alone for high risk localized endometrial cancer as defined by the three major randomized trials of adjuvant pelvic radiation. Gynecol Oncol. 2010. 116:404–407.
35. ASTEC study group. Kitchener H, Swart AM, Qian Q, Amos C, Parmar MK. Efficacy of systematic pelvic lymphadenectomy in endometrial cancer (MRC ASTEC trial): a randomised study. Lancet. 2009. 373:125–136.
36. Convery PA, Cantrell LA, Di Santo N, Broadwater G, Modesitt SC, Secord AA, et al. Retrospective review of an intraoperative algorithm to predict lymph node metastasis in low-grade endometrial adenocarcinoma. Gynecol Oncol. 2011. 123:65–70.
37. Mariani A, Webb MJ, Keeney GL, Haddock MG, Calori G, Podratz KC. Low-risk corpus cancer: is lymphadenectomy or radiotherapy necessary? Am J Obstet Gynecol. 2000. 182:1506–1519.
38. Fotiou S, Trimble EL, Papakonstantinou K, Kondi-Pafiti A, Panoskaltsis T, Deliconstantinos G, et al. Complete pelvic lymphadenectomy in patients with clinical early, grade I and II endometrioid corpus cancer. Anticancer Res. 2009. 29:2781–2785.
39. Susumu N, Sagae S, Udagawa Y, Niwa K, Kuramoto H, Satoh S, et al. Randomized phase III trial of pelvic radiotherapy versus cisplatin-based combined chemotherapy in patients with intermediate- and high-risk endometrial cancer: a Japanese Gynecologic Oncology Group study. Gynecol Oncol. 2008. 108:226–233.
40. Landrum LM, Mannel RS, Moore KN, Walker JL, Syzek EJ, Zuna RE, et al. Vaginal cuff brachytherapy combined with carboplatin and paclitaxel as adjuvant therapy for high-intermediate-risk patients with endometrial carcinoma. J Clin Oncol. 2010. 28:15s. (abstr 5095).




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download