Abstract
Objective
Concurrent chemoradiation has improved survival of patients with cervical carcinoma. However, follow-up of randomized studies is relatively short and data on long term toxicity are scarce, as is information on their health-related quality of life. This study assesses and compares incidences of late side-effects among patients treated with radiotherapy or chemoradiation using two toxicity scoring systems, and investigates impact on health-related quality of life.
Methods
Between 1985 and 1993, 114 patients underwent radiotherapy (n=39) or chemoradiation (n=75) for stage IIA-IVB cervical carcinoma. Late side-effects were scored retrospectively by reviewing medical charts using standardised checklists, focusing on bladder- and intestinal side effects. Health-related quality of life was assessed once using the EORTC QLQ-C30.
Results
No significant differences in late treatment-related side-effects between radiotherapy and chemoradiation groups were found. Grade ≥ 2 toxicity was found in 33% (bladder), and in 6% (bowel). Only 1.8% had both grade 3-4 toxicity. Bladder syndrome with high urinary frequency, urine incontinence and small bowel toxicity had a significant impact on health-related quality of life.
In developing countries, carcinoma of the cervix is an important cause of cancer-related death in women [1,2]. The 5-year overall survival rate depends mainly on tumour stage [1,3-5] and varies from 98% in early stage disease to 10% in the most advanced stages [5]. In the last decade, outcome has improved due to the development of new treatment strategies such as the addition of chemotherapy to radiation [6-8].
Currently, a number of treatment options for patients with cervical cancer are available, including surgery, radiotherapy, chemotherapy and hyperthermia, either as single or as combined modality, and the choice of treatment aims at achieving the best results with the least morbidity [5,9,10].
Until 1999, the primary treatment for locally advanced cervical carcinoma was radiotherapy, where the tolerance of normal tissues limits the dose intensity [5,11]. Recently, the results of a number of clinical phase III studies have shown that adding cisplatin-based chemotherapy provides higher cure rates than radiotherapy alone [12-15]. Therefore, in patients with stage IIB and higher, concurrent chemoradiation is now considered standard treatment [1,3,16,17]. As a result, the number of surviving patients has increased as well as the prevalence of women suffering from late radiation-induced side effects [1,17]. It could be hypothesized that the addition of chemotherapy to radiation has increased the risk of late side effects. However, as the follow-up of most randomized studies still is relatively short, reliable data regarding late side effects are scarce.
A number of scoring systems for late treatment related side effects exist, of which the Common Terminology Criteria for Adverse Events version 3.0 (CTCAE v3.0) and 'The late morbidity scoring scheme' from Radiation Therapy Oncology Group/European Organization for Research and Treatment of Cancer (RTOG/EORTC), are the most frequently used [1,11,12,18-25]. In the RTOG/EORTC scoring system, the number of toxicity scales related to side effects of the gastrointestinal and urinary tract is limited as compared to the CTCAE v3.0 scoring system, which enables a more precise definition of these side effects. The difference between these scoring systems may have consequences for the reporting of late side effects among various studies. Determination of the precise incidence and prevalence of radiation-induced side effects requires a direct comparison between these two systems in the same study cohort. It might be assumed that the grading of late side effects may be related to the health-related quality of life scores (HRQoL). However, this assumption has never been studied among patients curatively treated for cervical cancer.
Therefore, the purposes of this study were: 1) to assess the incidence of late radiation-induced side effects among patients curatively treated with radiotherapy with or without chemotherapy; 2) to assess whether the addition of concurrent chemotherapy resulted in higher rates of late radiation-induced side effects; 3) to investigate the association between late treatment-related side effects and HRQoL scored with the mentioned scoring systems.
The population of this retrospective cohort study was composed of 114 patients who were treated primarily with curative intent for locally advanced cervical carcinoma at the University Medical Centre of Groningen (UMCG) in the period from 1985 to 1993. Thirty-nine patients (34%) received curative radiotherapy (RT) alone from 1986-1989, while 75 patients (66%) received concurrent chemoradiation (CRT) from 1989-1993 in a phase II study [26].
For pre-treatment tumour staging, physical examination under general anesthesia was performed by the gynecologic oncologist together with the radiation-oncologist. Tumour staging was performed according to the International Federation of Gynecology and Obstetrics (FIGO)-classification system. A chest X-ray or computed tomography (CT) scan of the thorax was performed in all patients as well as a pelvic and abdominal CT scan to assess lymph node status. Ultrasound of the urinary tract, cystoscopy, and/or proctoscopy was only performed when clinically indicated. Some patients underwent a lymphangiography to assess lymph node involvement.
Radiation therapy was delivered by a 6 megavolt (MeV) photon linear accelerator in a standard protocol [27]. In general, a "box" technique was used, including an anterior, posterior and two lateral opposing fields with direct simulation. The superior limit of the anterior-posterior fields was the upper border of the fourth lumbar vertebra. The lower limit was the lower margin of the obturator foramen (or, in stage IIIA, the distal vagina). The lateral margin was 2 cm lateral from the transverse diameter of the pelvic brim. For the lateral fields, the ventral limit was the upper margin of the symphysis and the dorsal limit was the front of the sacrum. Radiation was given by 1.8 Gy daily fractions, five times per week to a total dose of 45 Gy.
Two weeks after completing external beam irradiation, a second examination under general anesthesia was performed and, if technically feasible, brachytherapy was applied. For this purpose, a 137Cesium application of 17.5 Gy to point A was given and this was repeated after one week up to a total dose of 35 Gy. If brachytherapy was not feasible or inappropriate in case of tumour extension into parametrium or lymph nodes, patients received an additional external boost over 3 weeks up to a total dose of 70.2 Gy, with standard fractionation.
Seventy-five patients received chemotherapy, including 3 cycles of carboplatin and 5-fluorouracil (5-FU). Carboplatin, 300 mg/m2, was dissolved in 250 ml 5% glucose and given over 30 minutes intravenously (i.v.) on day 1. 5-FU, 600 mg/m2, was dissolved in 2 liter normal saline and administered continuously i.v. on days 2-5. Cycles were repeated after 28 days for a total of 3 during the first, fifth and ninth week of treatment. Dose modifications only concerned carboplatin. Cycle 3 was given together with the external boost or in sequence to the second application of 137Cesium brachytherapy.
Until 1994, in Groningen, all patients who were feasible for surgery underwent an additional hysterectomy [28]. This comprised an extrafascial hysterectomy and removal of enlarged lymph nodes. In patients in whom a radical hysterectomy was not deemed feasible, no further action was taken.
Patients were followed by the radiation-oncologist alternating with the gynecologic-oncologist at regular intervals for 10 years. Late treatment-related side effects were evaluated during each visit by structured questioning daily life problems in physical and psychosexual functioning and with special attention to urinary tract and intestinal symptoms. A physical examination was performed for evaluating tumour recurrence and treatment-related side effects.
For the purpose of this study, side effects were scored retrospectively by reviewing the medical charts for late toxicity using standardised checklists. Treatment and follow-up of these patients has been done by 2 dedicated radiation oncologists with special expertise in gynecological oncology, and who were and are both very keen on assessing reporting toxicity. For this purpose, they used a well structured questioning methodology focusing on bladder and bowel toxicity. The first checklist was based on the CTCAE v3.0 and the second on the "late radiation morbidity scoring scheme" of the RTOG/EORTC [18,21], focusing on bladder- and intestinal toxicity. The RTOG/EORTC scoring system is a generally accepted method to assess radiation-induced side effects in gynecologic oncology. However, the main limitation of this scoring system is that it enables just one composed scale for urologic and one for intestinal side effects. The CTCAE v.3.0 enables scoring in different kinds of gastrointestinal and urologic side effects and provides a more comprehensive way of scoring radiation-induced side effects. For this reason, we used the CTCAE v3.0 to investigate the impact of these side effects on HRQoL.
A total number of 45 out of 114 patients (39%) still alive were asked to fill out a HRQoL questionnaire. Those who did not respond were contacted by telephone. Eventually, 34 out of 45 survivors (76%) responded. Three of the non-responders had a second malignancy that was treated with palliative chemotherapy. One patient refused to participate and seven patients did not respond for unknown reasons. Of the responders, 16 patients underwent an additional hysterectomy.
For the evaluation of HRQoL, the EORTC core questionnaire (QLQ-C30 ver. 3.0) was used [18,24,25]. The EORTC QLQ-C30 is a cancer-specific quality of life questionnaire developed for repeated assessments within clinical trials. It is developed in a cross-cultural setting and has been found valid and reliable for quality of life assessments in various cancer populations. It contains five functional scales (physical, cognitive, emotional, social and role), a global quality of life scale, three symptom scales (pain, fatigue and nausea/vomiting) and six single items (dyspnea, insomnia, loss of appetite, constipation, diarrhea and financial difficulties).
For the analysis of late radiation-induced side effects, the incidences of grade ≥ 2 late side effects during the first 10 years were estimated. Univariate and multivariate logistic regression analyses were performed to study the additional risk of concurrent chemoradiation reference to radiotherapy alone. Associations were expressed as odds ratios (OR) along with 95% confidence intervals (95% CI). An OR can be interpreted as a relative risk. First, univariate analyses were carried out to calculate the unadjusted association between treatment modality and side effects. In addition, multivariate analyses were performed to adjust for the imbalance between the two treatment groups with regard to age and follow-up time. The following variables were entered in the model: age, chemotherapy (yes or no), surgery (yes or no), FIGO stage (stage I-II vs. III) and boost technique (external beam versus brachytherapy). All results were considered statistically significant when p<0.05.
All scales of the EORTC QLQ-C30 were linearly converted to a 0 to 100 scale. For the functional and global health status/quality of life scales, higher scores represent a better level of functioning. For symptom scales, higher scores represent a greater degree of symptoms.
To analyze the association between the late treatment-related morbidity and HRQoL, the general linear model (GLM)-multivariate analysis of variance (MANOVA) was used. The GLM-MANOVA approach can be used to test the hypothesis of a significant association between a set of interrelated dependent variables, e.g., the quality of life scales, and one or more grouping variables. This method was preferred over analysis of each quality of life domain separately, because it also takes into account the correlation among the individual quality of life scales. This multivariate approach also protects against type I errors. In the present study, MANOVA was performed in two steps. First, to investigate the association of a given prognostic factor with HRQoL, an overall analysis was performed to establish whether the prognostic factors were significantly associated with any of the HRQoL domains. In case of a significant association between a late toxicity grading and all quality of life domains taken together, a second analysis was performed to investigate the association between that factor and each quality of life domain separately.
In the current study, the mean scores of the HRQoL scales observed among patients with a grade 2-4 were compared to the scores observed among patients with a grade 0-1 scoring. The clinical relevance of the differences in the mean scores of the HRQoL scales between groups was classified by calculating the effect size using Cohen's D coefficient. An effect size of ≥ 0.20-0.49 is generally considered small, ≥ 0.50-0.79 as moderate and ≥ 0.8 as large.
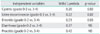
The pre-treatment characteristics of the study population are listed in Table 1. The two groups were well balanced with regard to most patient characteristics except for age. The mean age was 59 years in the RT group and 47 years in the CRT group (p<0.001). Brachytherapy was given to 23 of the patients in the radiotherapy group and to 38 patients in the combined group. Fifty-four percent of all patients underwent an additional (radical) hysterectomy (49% in the RT group, 56% in the CRT group). Until 1994 all patients underwent an additional hysterectomy if patients were feasible for surgery [28]. The mean follow-up was 4.0 years (range, 0.4 to 15.8 years) in the RT group and 6.8 years (range, 0.4 to 15.8 years) in the CRT group (p=0.002), respectively.
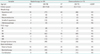
The total median follow-up time for the whole group investigated was 5.8 years, and was 6.8 years among the patient who received CRT compared to 4.0 years among those who received RT alone (p=0.002). With the EORTC/RTOG scoring system, the highest incidence of grade ≥ 2 late side effects was found for bladder toxicity (33%), while grade ≥ 2 late small and large intestinal toxicity was found in 6% of the patients. Only 1.8% had grade 3-4 toxicity for both bladder and bowel. Using the CTCAE v.3.0 scoring system, the highest incidence of grade ≥ 2 was observed for cystitis (39%). The CTCAE v.3.0 system provided a more detailed description of the different toxicities than the EORTC/RTOG system did with slightly higher incidence rates (Table 2). Using univariate and multivariate logistic regression analysis, no significant differences in baseline characteristics between the two treatment groups were observed with regard to the incidence of grade ≥ 2 side effects for any of the toxicity scales (Table 2).
The incidences of grade 3-4 late side effects were low (Table 2). No significant differences between the two treatment groups were observed. Because of the low number of events, multivariate logistic regression analysis was not feasible and therefore omitted.
In the first step of the GLM-MANOVA, the association between the CTCAE v3.0 toxicity scales and HRQoL was investigated. In this analysis, a linear combination of the functioning scales, the global QoL scale and general symptom scales assessed with all EORTC QLQ-C30 scales used as the dependent variable. Ileus and fecal incontinence were excluded from the analysis, because of the low number of events. The toxicity scales cystitis, urinary incontinence and enteritis were significantly associated with HRQoL (Table 3).
In addition, for the scales that significantly affected all HRQoL together, we investigated the impact of late radiation-induced morbidity on the individual HRQoL-scales. For cystitis, large effect were observed on different HRQoL scales, including global quality of life, physical functioning, role functioning, emotional functioning, social functioning and fatigue (Table 4). For urine incontinence, large effects were observed on global quality of life, physical functioning, role functioning, and social functioning (Table 4).
Enteritis had a significant effect on physical functioning, emotional functioning and insomnia (Table 5).
In this retrospective study, we examined the incidence of late radiation-induced side effects among patients curatively treated for cervical cancer that were followed for a long period of time. The results revealed that grade 2 or higher late radiation-induced side effects occurred in a relatively large proportion of patients of which the majority suffered from urinary tract toxicities. However, the incidence of severe, grade 3-4 side effects remained within reasonable limits, i.e. less than 2% for most toxicity scales up to 9.6% for urinary incontinence. Similar results were found by Lajer et al. [4] among 177 patients who received radiotherapy alone for cervical carcinoma. In their study, the incidence of grade 1, 2 and 3 toxicity together varied from 25 to 62%. The amount of grade 2 toxicity in their study was 2-32% for grade 1-2 and only 0-4% for grade 3 [4].
In the current study, the incidence of urine incontinence was 22% for all grade 2-4 and 9.8% for grade 3-4, which was higher than expected. However, the definition of urine incontinence according to the CTCAE v3.0 scoring system does not allow for a distinction between urine incontinence resulting from cancer treatment or other causes, e.g., surgery. In this respect, it should be noted that the overall incidence of urine incontinence in healthy elderly women in the Netherlands increases with age (Central Bureau for Statistics, the Netherlands, CBS), e.g., Kok et al. [29] reported on a cohort study among Dutch women of ≥ 60 years of age and found a prevalence of urine incontinence of 23.5%. The mean age of the current study population was 53 years at the time of treatment, and most of the women were post-menopausal, which means that the observed incidence of 22% will only be partly due to the cancer treatment.
Of our study population, 54% underwent an additional hysterectomy. The general policy at our hospital since 1994 is to perform an additional hysterectomy approximately 10 weeks after completion of radiation, if a biopsy proved to be positive for residual tumour. When a radical resection is considered possible by the gynecologist, a gynecologic examination under general anesthesia 8-10 weeks after completion of treatment is planned. In case a central biopsy proved to be tumour negative, no additional surgery is performed [28]. The high incidence of bladder toxicity may partly be due to the performed surgery in this group. In the CTCAE v3.0 overall toxicity is scored and not differentiated according to the type of treatment. For the currently treated patients, the incidence of bladder toxicity may be increased because of the biopsy positive additional surgery.
Although, we observed some trends towards more late radiation-induced side effects among patients treated with chemoradiation, e.g., for diarrhea and enteritis (CTCAE v3.0) and for small and large intestinal toxicities (EORTC/RTOG) These differences were not statistically significant, even after correction for two potential confounding factors (age and follow-up). Retrospective studies showed that the incidence of late bowel toxicity such as increased frequency, abdominal pain, diarrhea, rectal blood or mucus loss, and rectal discomfort increased dramatically with doses higher than 50-55 Gy [30]. However, with modern treatment techniques, the risk of severe late side effects is 5% or less [12,30]. Although in most randomized studies, acute toxicity rates were significantly higher with chemoradiation, this does not seem to result in more late side effects. These results are similar to those reported by Eiffel et al. [12].
The most recently adapted toxicity scoring system, the CTCAE v3.0, includes the definitions of a large set toxicity items for both acute and late side effects and does not only take into account toxicity induced by radiotherapy but also side effects induced by other treatment modalities such as surgery and chemotherapy [18,24]. Although the CTCAE v3.0 is currently the most specific and frequently used grading system for treatment-related side effects in clinical trials, most papers on radiotherapy will use the less specific RTOG/EORTC system.
Since 2006 there is a specific module for cervical carcinoma patients (CX 24). It specifies the problems that could exist after radiotherapy treatment e.g., bladder, intestine and sexual functioning. In the current study, toxicity was graded according to both CTCAE v3.0 and RTOG/EORTC systems, because the CX 24 was not available. The results of this study clearly indicate that mutual comparison of late radiation-induced side effects between studies that used different toxicity grading systems is severely hampered by these discrepancies.
The female pelvis contains several critical organs, and therefore a variety of complications may occur in patients treated with radiation therapy to this area. Severe complications may overshadow the more mild complications. Multiplicity of therapeutic approaches requires scoring systems that considers all types of side effects, but it has to specify the type of different complaints. Moreover, different kinds of late morbidity may have different impact. For instance, bowel obstruction can be treated and thus may be reversible, while urine incontinence may continue to increase throughout the remaining life period. In the current study, we found that cystitis, urine incontinence and enteritis had a severely/markedly negative impact on various HRQoL domains. It should be stressed that even though the majority of patients had grade 2 side effects or less, both general as well as the more specific dimensions of HRQoL were affected. The proportion of patients with grade 3-4 side effects was low and therefore, the impact of these higher grades of toxicity on HRQoL remains to be determined. Nevertheless, these results indicate that although physicians generally consider grade 2 side effects as mild and acceptable, from the patient's perspective the impact of these side effects may be impressive. Some "mild" side effects may have more effect than "severe" side effects, e.g., depending on their duration and potential for reversibility [4]. Similar results were found by other investigators [31].
The results of the present study clearly indicate that radiation-induced morbidity has a significant impact on various HRQoL domains. Especially bladder toxicity is a important finding, because late bladder toxicity increases in time [26]. Since survival in patients with cervical carcinoma increases, very late bladder toxicity may become a problem for these women.
In this study, the frequency of bladder toxicity may be high due to the use of older radiation techniques. The external beam radiation is planned with a box technique instead of CT planning nowadays. In reports obtained with intensity modulated radiotherapy in cervical cancer that have been published, only acute and early late side effects have been reported thus far [32].
A more important factor might be the brachytherapy technique. Dose prescription in point A gives high doses in rectum and bladder. Modern brachytherapy techniques with MRI planning can reduce these dose and give a more detailed dose distribution in organs at risk [33].
Although these developments in treatment techniques will reduce bladder- and rectal late treatment related morbidity, the impact on HRQoL is evident. Therefore, scoring late treatment related morbidity must be scored consequently in follow-up.
The present study with long term follow-up revealed a considerable proportion of patients with late grade 2 urinary and gastro-intestinal tract sequelae. These side effects have a major impact on HRQoL despite the occurrence of grade 3-4 toxicity in only a minority of patients. New radiation techniques aiming at reduction of these side effects may carry less toxicity with a positive impact on HRQoL.
Figures and Tables
Table 2
Cumulative incidence for toxicity grade 2 or higher and grade 3 or higher treatment-related morbidity

Table 3
Results of the general linear model multivariate analysis for variance testing the effect of the CTCAE v3.0 toxicity scales and on all health-related quality of life domains
References
1. Maduro JH, Pras E, Willemse PH, de Vries EG. Acute and long-term toxicity following radiotherapy alone or in combination with chemotherapy for locally advanced cervical cancer. Cancer Treat Rev. 2003. 29:471–488.
2. Kirwan JM, Symonds P, Green JA, Tierney J, Collingwood M, Williams CJ. A systematic review of acute and late toxicity of concomitant chemoradiation for cervical cancer. Radiother Oncol. 2003. 68:217–226.
3. Denton AS, Bond SJ, Matthews S, Bentzen SM, Maher EJ. UK Link Gynaecology-Oncology Group. National audit of the management and outcome of carcinoma of the cervix treated with radiotherapy in 1993. Clin Oncol (R Coll Radiol). 2000. 12:347–353.
4. Lajer H, Thranov IR, Skovgaard LT, Engelholm SA. Late urologic morbidity in 177 consecutive patients after radiotherapy for cervical carcinoma: a longitudinal study. Int J Radiat Oncol Biol Phys. 2002. 54:1356–1361.
5. Guidelines gynaecologic tumours: cervical carcinoma [Internet]. National Cancer Institutes. 2004. cited 2011 Jun 20. Bethesda, MD: National Cancer Instututes;Available from: http://www.cancer.gov.
6. Thomas GM. Improved treatment for cervical cancer: concurrent chemotherapy and radiotherapy. N Engl J Med. 1999. 340:1198–1200.
7. Ozsaran Z, Kamer S, Yalman D, Akagunduz O, Aras A. Treatment results and prognostic factors for cervical cancer patients treated by radiochemotherapy with weekly cisplatin. Eur J Gynaecol Oncol. 2007. 28:196–200.
8. King M, McConkey C, Latief TN, Hartley A, Fernando I. Improved survival after concurrent weekly cisplatin and radiotherapy for cervical carcinoma with assessment of acute and late side-effects. Clin Oncol (R Coll Radiol). 2006. 18:38–45.
9. Bentzen SM, Dorr W, Anscher MS, Denham JW, Hauer-Jensen M, Marks LB, et al. Normal tissue effects: reporting and analysis. Semin Radiat Oncol. 2003. 13:189–202.
10. van der Zee J, Gonzalez Gonzalez D, van Rhoon GC, van Dijk JD, van Putten WL, Hart AA. Comparison of radiotherapy alone with radiotherapy plus hyperthermia in locally advanced pelvic tumours: a prospective, randomised, multicentre trial: Dutch Deep Hyperthermia Group. Lancet. 2000. 355:1119–1125.
11. Chassagne D, Sismondi P, Horiot JC, Sinistrero G, Bey P, Zola P, et al. A glossary for reporting complications of treatment in gynecological cancers. Radiother Oncol. 1993. 26:195–202.
12. Eifel PJ, Winter K, Morris M, Levenback C, Grigsby PW, Cooper J, et al. Pelvic irradiation with concurrent chemotherapy versus pelvic and para-aortic irradiation for high-risk cervical cancer: an update of radiation therapy oncology group trial (RTOG) 90-01. J Clin Oncol. 2004. 22:872–880.
13. Green JA, Kirwan JM, Tierney JF, Symonds P, Fresco L, Collingwood M, et al. Survival and recurrence after concomitant chemotherapy and radiotherapy for cancer of the uterine cervix: a systematic review and meta-analysis. Lancet. 2001. 358:781–786.
14. Rose PG. Chemoradiotherapy for cervical cancer. Eur J Cancer. 2002. 38:270–278.
15. Chemoradiotherapy for Cervical Cancer Meta-Analysis Collaboration. Reducing uncertainties about the effects of chemoradiotherapy for cervical cancer: a systematic review and meta-analysis of individual patient data from 18 randomized trials. J Clin Oncol. 2008. 26:5802–5812.
16. Lukka H, Hirte H, Fyles A, Thomas G, Elit L, Johnston M, et al. Concurrent cisplatin-based chemotherapy plus radiotherapy for cervical cancer: a meta-analysis. Clin Oncol (R Coll Radiol). 2002. 14:203–212.
17. Tan LT, Russell S, Burgess L. Acute toxicity of chemo-radiotherapy for cervical cancer: the Addenbrooke's experience. Clin Oncol (R Coll Radiol). 2004. 16:255–260.
18. Common Terminology Criteria for Adverse Events v. 3.0. [Internet]. National Cancer Institute. 2003. cited 2011 Jun 20. Bethesda, MD: National Cancer Instututes;Available from: http://ctep.cancer.gov.
19. EORTC QLQ-C30 [Internet]. European Organization for Research and Treatment of Cancer. 2005. cited cited 2011 Jun 20. Brussel: EORTC;Available from: http://www.eortc.be.
20. Anacak Y, Yalman D, Ozsaran Z, Haydarog lu A. Late radiation effects to the rectum and bladder in gynecologic cancer patients: the comparison of LENT/SOMA and RTOG/EORTC late-effects scoring systems. Int J Radiat Oncol Biol Phys. 2001. 50:1107–1112.
21. Cox JD, Stetz J, Pajak TF. Toxicity criteria of the Radiation Therapy Oncology Group (RTOG) and the European Organization for Research and Treatment of Cancer (EORTC). Int J Radiat Oncol Biol Phys. 1995. 31:1341–1346.
22. Overgaard J, Bartelink H. About tolerance and quality: an important notice to all radiation oncologists. Radiother Oncol. 1995. 35:1–3.
23. Routledge JA, Burns MP, Swindell R, Khoo VS, West CM, Davidson SE. Evaluation of the LENT-SOMA scales for the prospective assessment of treatment morbidity in cervical carcinoma. Int J Radiat Oncol Biol Phys. 2003. 56:502–510.
24. Trotti A, Byhardt R, Stetz J, Gwede C, Corn B, Fu K, et al. Common toxicity criteria: version 2.0. an improved reference for grading the acute effects of cancer treatment: impact on radiotherapy. Int J Radiat Oncol Biol Phys. 2000. 47:13–47.
25. Trotti A, Colevas AD, Setser A, Rusch V, Jaques D, Budach V, et al. CTCAE v3.0: development of a comprehensive grading system for the adverse effects of cancer treatment. Semin Radiat Oncol. 2003. 13:176–181.
26. Pras E, Willemse PH, Boonstra H, Hollema H, Heesters MA, Szabo BG, et al. Concurrent chemo- and radiotherapy in patients with locally advanced carcinoma of the cervix. Ann Oncol. 1996. 7:511–516.
27. Willemse PH, de Vries EG, Pras E, Maduro JH. Treatment of cervical cancer. Lancet. 2002. 359:357–358.
28. Nijhuis ER, van der Zee AG, in't Hout BA, Boomgaard JJ, de Hullu JA, Pras E, et al. Gynecologic examination and cervical biopsies after (chemo) radiation for cervical cancer to identify patients eligible for salvage surgery. Int J Radiat Oncol Biol Phys. 2006. 66:699–705.
29. Kok AL, Voorhorst FJ, Halff-Butter CM, Janssens J, Kenemans P. The prevalence of urinary incontinence in elderly women. Ned Tijdschr Geneeskd. 1991. 135:98–101.
30. Coia LR, Myerson RJ, Tepper JE. Late effects of radiation therapy on the gastrointestinal tract. Int J Radiat Oncol Biol Phys. 1995. 31:1213–1236.
31. Bye A, Trope C, Loge JH, Hjermstad M, Kaasa S. Health-related quality of life and occurrence of intestinal side effects after pelvic radiotherapy: evaluation of long-term effects of diagnosis and treatment. Acta Oncol. 2000. 39:173–180.
32. Beriwal S, Gan GN, Heron DE, Selvaraj RN, Kim H, Lalonde R, et al. Early clinical outcome with concurrent chemotherapy and extended-field, intensity-modulated radiotherapy for cervical cancer. Int J Radiat Oncol Biol Phys. 2007. 68:166–171.
33. Wachter-Gerstner N, Wachter S, Reinstadler E, Fellner C, Knocke TH, Wambersie A, et al. Bladder and rectum dose defined from MRI based treatment planning for cervix cancer brachytherapy: comparison of dose-volume histograms for organ contours and organ wall, comparison with ICRU rectum and bladder reference point. Radiother Oncol. 2003. 68:269–276.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download