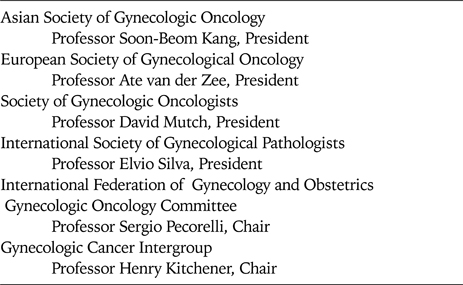
On behalf of the seven sister societies in gynecologic cancer, I am delighted to convey congratulations on the inaugural meeting of the Asian Society of Gynecologic Oncology to ASGO President Soon-Beom Kang, Officers, Council and members. By working together, we have made much progress. Working together in the future, we can make and we need to make much more progress in basic, translational, and clinical research, in education of health care professionals, the public, and policy makers, and in strengthening our annual and biennial meetings. To illustrate how we have made progress in reducing the global burden of women's cancer, we may look at the progress which has been made to combat the human papillomavirus (HPV) and HPV-associated neoplasia, including cervical cancer, over the past two centuries. We have made major progress across the continuum of cancer control, including primary prevention, secondary prevention, treatment, symptom management, and palliation and end-of-life care.
One of the first advances was in pain control. Friedrich WA Sertürner isolated morphine in Germany in 1804. He named morphine after Morpheus, the Greek god of sleep. The next advance of note was in epidemiology. Domenico Rigoni-Stern of Italy observed that cervical cancer occurred less often in nuns while breast cancer occurred more commonly among nuns. The surgical treatment of invasive cervical cancer underwent rapid development at the end of the 19th century. John Goodrich Clark, working in the US, described a radical abdominal hysterectomy in 1895, while Friedrich Schauta, working in Austria, described a radical vaginal hysterectomy in 1898. Two years later, in 1900, Ernst Wertheim, also working in Austria, described an abdominal radical hysterectomy. About the same time, Marie and Pierre Curie, working in France, isolated radium. This radioactive element was first used to treat cervical cancer by direct topical application in 1903. External beam irradiation was added to the treatment of cervical cancer in the 1920s. George Papanicolaou, working in the US, reported the use of cervical cytology to identify cancer in 1928. Subsequently, he found that cervical cytology could identify precursor lesions, thus permitting the treatment of preinvasive disease, via both excision (via hysterectomy or conization) or ablation (via cautery, laser, or cryotherapy).
More rapid progress began with the identification of HPV as the causative agent of cervical cancer by Harold zur Hausen, working in Germany, in 1976. This finding made possible extensive investigations into the epidemiology, natural history, and biology of HPV, the development of prophylactic and therapeutic HPV vaccines, and the identification of other risk factors for HPV-associated neoplasia, such as chronic immunosuppression, cigarette smoking, prolonged use of oral contraceptives, and high-risk male partners. Today we now have two prophylactic HPV vaccines approved for use, Gardisil®, which provides protection against infection with HPV subtypes 6, 11, 16, and 18, and Cervarix®, which provides protection against infection with HPV subtypes 16 and 18.
We have also made advances in cancer treatment through the finding that platinum-based chemoradiation significantly improves both progression-free survival and overall survival compared with radiation only in women with locally advanced cervical cancer. In addition, we have learned how to decrease the morbidity of treatment. The nerve-sparing radical hysterectomy, described by Takashi Kobayashi, working in Japan, in 1961, helps preserve bowel, bladder, and vaginal function. Neoadjuvant chemotherapy, pioneered by Juan Sardi in Argentina in 1986, has been shown to shrink cervical cancers dramatically, leading to less radical surgery. More recently, gynecologic surgeons have developed fertility-sparing procedures, including radical trachelectomy, first reported by Daniel Dargent in France and Michel Roy in Canada, and neoadjuvant chemotherapy followed by conization.
We have also improved care at the end of life, such as better pain control using the WHO pain control pyramid. We have learned how to preserve renal function with stent, preserve gastrointestinal function with ostomies, and control hemorrhage with arterial embolization via interventional radiology. The US NCI has helped develop a comprehensive educational program for symptom control and end-of-life care for cancer patients, entitled "Education in Palliation and End-of-Life Care for Oncology Curriculum."
The World Health Organization, the International Union against Cancer, the American Cancer Society, the US Centers for Disease Control, and the US National Cancer Institute have worked together to help develop recommendations for national cancer control plans. Comprehensive cervical cancer control has now become a standard part of national cancer control planning and policies. Policy makers are now wrestling with such issues as how to pay for and encourage wide-spread uptake of prophylactic HPV vaccines, how to ensure compliance with recommendations for screening, and how to encourage access to treatment of preinvasive HPV-associated neoplasia and cervical cancer.
We have also learned the importance of multidisciplinary care in the treatment of women with gynecologic cancer. Disciplines central to our work include gynecologic oncology, gynecologic pathology, radiation oncology, medical oncology, and gynecologic oncology nursing. Our education programs must involve all these disciplines. We also need to ensure that our collaborators in other disciplines, such as epidemiology, biostatistics, basic and translational science, pharmacology and pharmacy, psychology, rehabilitation and palliative medicine, understand the unique challenges in gynecologic cancer. We also have responsibility for educating our patients, their families, and the general public about the importance of a healthy lifestyle, adherence to screening recommendations for breast, cervical, and colon cancer, the early symptoms of gynecologic cancer, and the importance of cancer research and clinical trials.
What have we learned from the experience of older gynecologic oncology societies? First, our societies must be multidisciplinary, with each medical discipline treated with the same respect. Second, geographic rotation of meetings will permit more people to attend. The International Gynecologic Cancer Society, for example, has met in Australia, Japan, Korea, and Thailand. Third, our societies should schedule their meeting dates and sites to complement each other and promote one another's meetings. Fourth, society meetings should promote academic clinical trials, disseminate the results of important trials, and facilitate the development and coordination of new trials. Finally, the leadership of our sister societies should meet several times a year to share information and coordinate educational programs. We must continue to work together to reduce the global burden of gynecologic cancer.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download