Abstract
To make an overview of the current status of gynecologic cancer in Japan, we reviewed the recent incidence of cervical, endometrial, and ovarian cancer in Japanese women. The incidence of all three cancers has increased, but trends differ respectively. In age specific cancer site distribution data, the uterus and ovary are leading sites of high incidence among Japanese women younger than 40 years of age. Therefore, fertility sparing cancer treatment has received much attention. Several multicenter clinical trials have been done by Japanese groups, and some excellent evidence has been collected for endometrial and ovarian cancer. A promising international collaboration trial for ovarian clear cell carcinoma is also underway at the present time.
Incidence of disease and social environment has been changing. Cancer has become to the leading cause of death and the number of gynecologic cancer patients is constantly increasing. The Japan Society of Gynecologic Oncology (JSOG) first published treatment guidelines for ovarian cancer in 2004, endometrial cancer in 2006, and cervical cancer in 2007. These guidelines are revised every 3 years and the 2nd edition of the guidelines for ovarian cancer treatment was published in 2007. An English version of the ovarian cancer (1st edition) guidelines was also published. These publications contribute to standardizing treatment for Japanese gynecologic cancer patients. This paper reviews recent trends in gynecologic cancer incidence and treatment.
As in other developed countries, cancer has become the leading cause of death in Japan since the 1980's. Fig. 1 shows the change in mortality rate per 100,000 population.1 The mortality rate of uterine cancer including the cervix and corpus consistently decreased from the 1960's until 1995, as the cervical cancer screening system spread nationwide across Japan. The mortality rate of ovarian cancer is increasing remarkably along with breast and gastrointestinal cancer.
The incidence of gynecologic cancer is site specific. Uterine cervix, uterine corpus, and ovary each have an individual trend. Over the past 20 years, the age specific incidence of cervical cancer has transfigured (Fig. 2). The incidence among women aged 40 to 80 has remarkably declined. Nevertheless, the incidence among women age in their 20's and 30's has increased. The increase in the incidence of high risk type HPV infection in this generation must be the cause of this peak. The small number of young women who receive cervical cancer screening is another serious problem. In addition, HPV DNA testing is still not covered by national health insurance. These problems must be solved to protect young women from cervical cancer.
Endometrial cancer has also increased remarkably. According to the Gynecologic tumor committee of the JSOG, the total number of endometrial cancer cases from registered institutions was 976 cases in 1983, increasing to 2,115 cases in 1994, and reached to 4,267 cases in 2005.2 It accounts for 47% of the total number of uterine cancer patients (excluding CIN). Also, the rate of young women under 40 years of age among all endometrial cancer patients has been increasing. It was 4.9% in 1983, rose to 5.1% in 1994, and hit 7.0% in 2005.2 It is obvious that endometrial cancer in Japanese women has a tendency to occur at a young age (Fig. 3). Ovarian cancer has also increased, but a remarkable increase in incidence has occurred in patients over 60 years of age (Fig. 4). There has been no reduction in the number of ovarian cancer deaths in the past 40 years (Fig. 1). In spite of the recent progress in medical technology, we have not been able to keep up with the increase in new patients.
Recent changes in women's life styles have lead to their late marriage, reduction in the birth rate and a rise in maternal age at delivery. According to data from the Ministry of Health, Labor, and Welfare, the average age at first delivery in 2005 was 29.1 years of age, which is 2.7 years older than in 1980. On the other hand, the number of younger cancer patients has been increasing. Among female cancer patients 39 years old and younger, uterine cancer now has the highest incidence rate since 1995, and the incidence of ovarian cancer is also increasing. The incidence rates of uterine and ovarian cancer was 24% of all female cancer in 1975 made up 44% of all female cancers in 2000 (Fig. 5). Thus, fertility preserving therapy for gynecologic cancer has received much attention.
Recently, approximately half of all cervical cancer patients in Japan have stage 0 tumors. According to the 2007 data of the JSOG, conization or other uterine preserving surgery is employed in approximately 85% of all CIN III and 45% of stage Ia1 patients, regardless of their wishes for fertility.3 In contrast, data for 1995 showed that conization was done in only 40% of CIN III cases.4 Recent advances in surgical devices, such as laser or radio-wave knife have brought technical simplicity and safety to conization.
Recently, radical trachelectomy has been introduced for stage Ib1 invasive cervical cancers. In Japan, more institutions prefer the abdominal procedure than laparoscopy. In spite of eager efforts, only a few successful offspring have been reported so far, because of a low pregnancy rate and a high incidence of abortions. It has not become the standard treatment for invasive cervical cancer yet.
Progesterone has played the major role in conservative therapy for endometrial cancer. Only medroxyprogesterone (MPA) is available for endometrial cancer in Japan. Kaku et al.5 reported a multi-institutional retrospective study on the status of fertility sparing treatment for endometrial cancer in Japan. In this report, there were discrepancies in many cases between the original histological diagnosis and the final diagnoses by central pathological review. Patients were treated with MPA at 200-800 mg for 2-14 months by each institutional policy. According to this result, the Japanese Gynecologic Cancer Study Group conducted a multi-institutional prospective phase II study of fertility sparing treatment. Inclusion criteria is as follows, patients with histologically confirmed atypical endometrial hyperplasia or endometrioid adenocarcinoma grade 1 at presumed stage Ia disease, and a strong desire to preserve fertility.6 MPA was administered 600 mg/day with 81 mg of aspirin for 26 weeks. The overall complete response rate was 67% (26/39), which included 55% (12/22) endometrioid adenocarcinomas and 82% (14/17) atypical endometrial hyperplasias. In this study, among 20 patients desiring to conceive, 7 normal full term deliveries were achieved out of 12 pregnancies. Most pregnancies were brought on by assisted reproductive treatment, and five in particular were achieved by the in vitro fertilization and embryo transfer (IVF-ET) program. Nevertheless, the author also paid attention to their high recurrence rate (47% of complete response cases) and 3 cases with synchronous ovarian and 1 peritoneal cancer in this study. According to the 2007 JSOG data, 13% of atypical endometrial hyperplasias were treated by hormonal therapy. Although the newest data on the incidence of conservative therapy for stage Ia endometrial cancer is not available, it may be one of the standard treatments for Japanese women with atypical hyperplasia or stage Ia endometrial cancer who desire to preserve their fertility.
There is no definite consensus about the indication of fertility preserving treatment for epithelial ovarian cancer. According to the 2007 ovarian cancer treatment guidelines of the JSOG, patients with a strong desire for child bearing who are stage Ia with well differentiated or borderline tumor are permitted to receive conservative surgery. It is noted that there is no difference in prognosis between ruptured Ic (b) and stage Ia. Clear cell adenocarcinoma and moderate or poorly differentiated tumors are not included in this category.7 In clinical practice, each institution has a number of patients who have preserved their fertility violating this rule and some have conceived or recurred after treatment. Preserving fertility in stage Ia with clear cell histology or unilateral stage Ib or Ic tumor may be permitted with exception. The Japanese Gynecologic Cancer Study Group collected data on this issue from 30 major Japanese institutions. A new concept reflecting the present Japanese status regarding this issue will be revealed soon.
In western countries, external radiation therapy is still the standard treatment as a postoperative adjuvant for endometrial cancer. Chemotherapy has been employed for recurrent or advanced disease. Many Japanese physicians switched their adjuvant therapy for endometrial cancer from radiation to chemotherapy in the early 90's. Cyclophosphamide, adriacin, cisplatin (CAP) combination became the standard regimen for endometrial cancer in Japan as well as ovarian cancer. The Japan Society Gynecologic Oncology Group (JGOG) conducted a randomized control study comparing whole pelvic radiotherapy to platinum based chemotherapy (CAP) to clarify which is more effective as the adjuvant therapy for stage Ic to IIIc endometrial cancer (JGOG 2033). Four hundred seventy-five patients were recruited from 1994 to 2000, and were divided into the CAP and radiotherapy groups. This study showed that chemotherapy group had a significantly higher progression free survival and overall survival rate than the pelvic radiotherapy group among patients in the high to intermediate risk group (stage Ic over 70 years old, with G3 endometrioid adenocarcinoma or stage II or IIIa by positive cytology).8 This was the first report showing superiority of chemotherapy over radiotherapy for early stage endometrial cancer, and was accepted at the oral presentation of ASCO in 2005. From a recent JGOG interior report, paclitaxel/carboplatin (TC) has been reported to be the most used combination for endometrial cancer in Japan. Although adriacin/cisplatin (AP) has been approved, evidence in a GOG study shows that AP is used in only 8% of all chemotherapy regimens. JGOG is now carrying out a three-arm randomized control trial (JGOG 2043) to decide which is the best combination as adjuvant therapy, TC, AP, or docetaxel/cisplatin (DP) (Fig. 6). Six hundred patients are expected to participate, and over 430 patients have participated in this trial already.
As in other countries, TC is the most frequently used combination for adjuvant chemotherapy in ovarian cancer. A triweekly schedule is the standard regimen. A dose-dense weekly schedule showed promising effects in some phase II studies.9 Weekly administration of paclitaxel has also been employed in clinical practice in Japan for several reasons, not only for effect, but also less toxicity, and high adjustability. JGOG conducted a large phase III study (JGOG 3016) comparing conventional dose paclitaxel 180 mg/m2 and carboplatin AUC 6 on day 1 every 21 days (c-TC) with a dose-dense weekly schedule of 80 mg/m2 of paclitaxel on days 1,8, and 15, and carboplatin (AUC 6) on day1 (dd-TC). Among 637 patients enrolled, dd-TC (N=317) showed a statistically significant longer PFS than c-TC (N=320). Also, the 2-year survival rates were 83.6% in dd-TC, and 77.7% in c-TC (p=0.0496). Grade 3 and 4 anemia was reported more frequently in the dd-TC group, and other toxicities were similar in both groups (Table 1). This report had a great impact and was selected as one of the best of ASCO in 2008.10 It is still unclear whether the standard therapy should be changed to a weekly schedule or not. Nevertheless, weekly administration of TC must be a good option for epithelial ovarian cancer according to this result.
Clear cell adnocarcinoma (CCC) has a higher incidence rate in Japan, at 20-25% of all epithelial ovarian cancers, than in other Asian or Western countries (5-10%). It is still increasing in Japan. Most studies regarding CCC and its chemo-sensitivity are from Japan. Sugiyama et al showed the platinum resistance of CCC compared with serous carcinoma.11 The Osaka group showed that CCC had also a poor response with TC and poor prognosis compared with other histologic types.12 Irinotecan (CPT-11) combined with cisplatin were introduced as the favorable regimen for refractory or recurrent ovarian cancer.13 A Japanese multi-center retrospective study showed that there was no difference in progression free survival between the CPT-P group (patients treated with CPT-11 plus cisplatin) and the TP group (patients treated with taxane plus platinum combination) in patients with stage I and patients with suboptimally debulked stage II-IV tumor. Nevertheless, among patients with optimally debulked stage II-IV tumor, the CPT-P group showed a significantly better progression free survival than the TP group.14 The JGOG conducted phase II trials to find the safety and response rate for both TC and CPT-P chemotherapy (JGOG 3014). Then the JGOG proposed a worldwide randomized control study of TC versus CPT-P chemotherapy (GCIG/GOG 3017), and is expecting a total of 652 patients to be enrolled (Fig. 7). It started at September 2006, and 337 patients including 15 patients from the KGOG have already enrolled as of the end of this April.
In response to national demand to receive excellent cancer treatment all over Japan, the JSGO started an authorization system for gynecologic oncologists since 2004, resembling the SGO of United States. Doctors wanting to be authorized need to pass written and oral tests organized by the JSGO. Currently 460 specialists for gynecologic oncology have been authorized by the JSGO and they are working hard teaching young trainees to be gynecologic oncologists throughout Japan. They belong to major hospitals, authorized as training facilities, for teaching gynecologic oncologists. These hospitals are also acting as regional centers, trying new treatment strategies, and recruiting many patients for multicenter clinical trials including international collaboration. In the future, a more excellent outcome can be expected from Japanese and other Asian groups participating in these trials.
Figures and Tables
Fig. 1
Changes in site distribution of the cancer mortality rate of Japanese women. Uterine cancer decreased until 1995, then slightly increased. Ovarian cancer increased similar to breast, rectal and colon cancer.
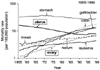
Fig. 2
Changes in the age-specific incidence rate of cervical cancer in Japanese women. The total number of incidences decreased remarkably between 1980 and 2000. Nevertheless, there was an obvious elevation in the incidence rate for women in their 20's and 30's in 2000 (Source: center for cancer control and information services, National Cancer Center, Japan).
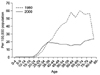
Fig. 3
Changes in the age-specific incidence rate of endometrial cancer. Total number of incidences obviously increased. The rise in younger patients stands out (Source: center for cancer control and information services, National Cancer Center, Japan).
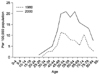
Fig. 4
Changes in the age-specific incidence rate of ovarian cancer. A striking increase is shown in women at over sixty of age (Source: center for cancer control and information services, National Cancer Center, Japan).
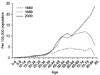
Fig. 5
Changes in site distribution of the cancer incidence rate for ages 0 to 39. The incidence of cancer in the female genital tract certainly has increased more than any other cancer site among younger women (Source: center for cancer control and information services, National Cancer Center, Japan).

Fig. 6
Protocol scheme of JGOG 2043 for adjuvant chemotherapy for endometrial cancer. Patients eligibility: Patients who received surgical staging laparotomy, and pathologically confirmed endometrial cancer under the following conditions. 1) FIGO stage Ic to II, with grade 2 or 3 tumor (G3 included serous, clear, undifferentiated tumor). 2) FIGO stage III and IV tumor without distant metastasis. 3) age 20 to 75 years old, performance status 0-2, reasonable organ function.

Fig. 7
Protocol scheme of GCIG/JGOG 3017 for adjuvant chemotherapy for ovarian clear cell carcinoma patients eligibility: Patients with a pathologically confirmed clear cell carcinoma of the ovary. The histological diagnosis will be confirmed by central pathological review. Ages 18 or older, reasonable organ function.
PFS: progression-free survival, OS: overall survival

References
1. Oshima A, Kuroisi T, Tajima K. Cancer statistic statement. 2004. Tokyo: Shinohara Publishing.
2. Report from gynecologic tumor committee of JSOG. Acta Obstet Gynaecol Jpn. 2007. 59:952.
3. Report from gynecologic tumor committee of JSOG. Acta Obstet Gynaecol Jpn. 2009. 61:936.
4. Report from gynecologic tumor committee of JSOG. Acta Obstet Gynaecol Jpn. 2000. 52:855.
5. Kaku T, Yoshikawa H, Tsuda H, Sakamoto A, Fukunaga M, Kamura T, et al. Conservative therapy for adenocarcinoma and atypical endometrial hyperplasia of the endometrium in young women: central pathologic review and treatment outcome. Cancer Lett. 2001. 167:39–48.
6. Ushijima K, Yahata H, Yoshikawa H, Konishi I, Yasugi T, Saito T, et al. Multicenter phase II study of fertility-sparing treatment with medroxyprogesterone acetate for endometrial carcinoma and atypical hyperplasia in young women. J Clin Oncol. 2007. 25:2798–2803.
7. Japan Society of Gynecologic Oncology. Ovarian cancer treatment guidelines 2007. 2007. Tokyo: Kanehara & Co. Ltd.
8. Susumu N, Sagae S, Udagawa Y, Niwa K, Kuramoto H, Satoh S, et al. Randomized phase III trial of pelvic radiotherapy versus cisplatin-based combined chemotherapy in patients with intermediate- and high-risk endometrial cancer: a Japanese Gynecologic Oncology Group study. Gynecol Oncol. 2008. 108:226–233.
9. Rose PG, Smrekar M, Fusco N. A phase II trial of weekly paclitaxel and every 3 weeks of carboplatin in potentially platinum-sensitive ovarian and peritoneal carcinoma. Gynecol Oncol. 2005. 96:296–300.
10. Isonishi S, Yasuda M, Takahashi F, Katsumata N, Kimura E, Aoki D, et al. Randomized phase III trial of conventional paclitaxel and carboplatin (c-TC) versus dose dense weekly paclitaxel and carboplatin (dd-TC) in women with advanced epithelial ovarian, fallopian tube, or primary peritoneal cancer: Japanese Gynecologic Oncology [abstract]. J Clin Oncol. 2008. 26(15S):abstr 5506.
11. Taguchi K. Clinical characteristics of clear cell carcinoma of the ovary: a distinct histologic type with poor prognosis and resistance to platinum-based chemotherapy. Cancer. 2000. 88:2584–2589.
12. Enomoto T, Kuragaki C, Yamasaki M, Sugita N, Otsuki Y, Ikegami H, et al. Is clear cell carcinoma and mucinous carcinoma of the ovary sensitive to combination chemotherapy with paclitaxel and carboplatin? [abstract]. Proc Am Soc Clin Oncol. 2003. 22:abstr 1797.
13. Sugiyama T, Yakushiji M, Nishida T, Ushijima K, Okura N, Kigawa J, et al. Irinotecan (CPT-11) combined with cisplatin in patients with refractory or recurrent ovarian cancer. Cancer Lett. 1998. 128:211–218.
14. Takano M, Kikuchi Y, Yaegashi N, Suzuki M, Tsuda H, Sagae S, et al. Adjuvant chemotherapy with irinotecan hydrochloride and cisplatin for clear cell carcinoma of the ovary. Oncol Rep. 2006. 16:1301–1306.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download