Abstract
Objective
To evaluate the acute toxicity of rofecoxib during concurrent use with cisplatin-based chemoradiotherapy (CCRT) in patients with cervical cancer.
Methods
We evaluated 67 FIGO stage IB2-IVA cervical cancer patients treated with CCRT between June 2002 and July 2004. The study group included patients who received rofecoxib (N=30) and the control group included patients who received CCRT only (N=37). The patients' medical records were retrospectively reviewed for patient characteristics, toxicity related to CCRT and treatment results.
Results
There were no significant differences in toxicity between the two groups. The most common acute grade 3/4 toxicity was neutropenia (13.3% in the study group and 21.6% in the control group). Grade 3/4 late toxicity was observed in 2 (6.6%) patients in the study group and 3 (8.1%) in the control group. There was no treatment-related deaths in either group. Six (20.0%) patients in the study group had treatment failure. In the control group, 6 (16.2%) patients experienced treatment failure. Progression-free and overall survival was 55.8±4.2 and 59.0±2.8 months, respectively, in the study group, and 69.7±4.3 and 71.6±3.6 months, respectively, in the control group. There were no differences in progression-free and overall survival between the 2 groups.
Conclusion
Our data indicate that rofecoxib, at a dose of 25 mg twice daily, has acceptable acute toxicity as a radiosensitizer during CCRT. Although rofecoxib was not efficacious as a radiosensitizer in the present study, the benefit of rofecoxib as a radiosensitizer should be further evaluated in a prospective study.
Uterine cervical cancer is the second most common gynecologic malignancy worldwide. In Korea, cervical cancer is the third leading gynecologic cancer and it accounts for 9.8% of newly diagnosed cancer in Korean women, with approximately 4,500 new cases diagnosed in 2002.1 Radiotherapy is one of the major treatment modalities for cervical cancer. In particular, concurrent chemoradiotherapy (CCRT) has improved the overall survival rate in women with locally advanced cervical cancer.2-6 However, one-third of patients with locally advanced cervical cancer still experience treatment failure within 2 years.4 Therefore, there is an urgent need to improve the survival rate of patients with locally advanced cervical cancer.
Cyclooxygenase (COX)-2 is one of the promising molecules that may improve the survival rate of patients with cervical cancer. COX is a key enzyme that catalyzes the conversion of arachidonic acids into prostaglandins, which are involved in carcinogenesis. The 2 isoforms of cyclooxygenase, COX-1 and -2, work in a similar fashion and share 61% homology at the amino acid level. Under many circumstances, COX-1 is constitutively expressed whereas COX-2 can undergo rapid induction through various stimuli.7 COX-2 expression has an important role in tumor angiogenesis, apoptotic inhibition, and tumor cell proliferation.8-10 COX-2 expression is known to be associated with various malignancies, including cervical cancer.11-13 Additionally, numerous studies have reported that COX-2 overexpression is associated with poor prognosis and an unfavorable outcome in uterine cervical cancer.3,14,15 Therefore, COX-2 is considered a target molecule and a COX-2 inhibitor may be a candidate agent for the treatment and prevention of cervical cancer.
Several COX-2 inhibitors, such as rofecoxib, celecoxib, valdecoxib and parecoxib, have been developed and phase II clinical trials for celecoxib have already been completed. However, there are few studies on the efficacy and toxicity of other COX-2 inhibitors, such as rofecoxib, in the treatment of cervical cancer. Merck & Co. (Whitehouse Station, NJ, USA) withdrew rofecoxib from the market because of concerns about the increased risk of cardiovascular disease. It is difficult to prospectively evaluate the acute toxicity and efficacy of rofecoxib as a radiosensitizer for the treatment of cervix cancer. Therefore, we performed this study to evaluate the acute toxicity of rofecoxib when it is used as an adjuvant agent to improve radiosensitivity for CCRT in the primary treatment of cervical cancer.
For this study, we enrolled patients with FIGO stage IB2-IVA cervical cancer who were treated with CCRT between June 2002 and July 2004 at the Department of Obstetrics and Gynecology, Yonsei University Health System. Patient demographic data, treatment results and treatment related complications were retrospectively reviewed from the patients' medical records. Clinical staging of uterine cervical cancer for each patient was based on the FIGO classification system. The medical records of 188 consecutive patients who were diagnosed with cervical cancer and treated at our institution from June 2002 to July 2004 were initially reviewed. Fig. 1 summarizes the distribution of the patients. Of the 188 patients, we included 67 patients with stage IB2-IVA cervical cancer who received concurrent chemoradiotherapy. Patients received CCRT if they met the following criteria: 1) a performance status of 2 or less on the Eastern Cooperative Oncology Group (ECOG) scale; 2) adequate bone marrow, hepatic and renal functions defined as white blood cells ≥ 4,000 /mm3, absolute neutrophil count (ANC) ≥ 1,500 /mm3, platelet count ≥ 100,000 /mm3, hemoglobin ≥ 8.0 g/dl, serum bilirubin ≤ 1.5 mg/dl, alanine aminotransferase/aspartate aminotransferase ≤ 2.5 times the upper limit of normal and serum creatinine ≤ 1.5 mg/dl; and 3) written informed consent and agreement to undergo rofecoxib treatment. Patients who had medical illness preventing the use of rofecoxib were considered ineligible for rofecoxib treatment. Such medical illness included the following: previous psychiatric illness, previous hypersensitivity to COX-2 inhibitor, known human immunodeficiency virus infection, active gastrointestinal ulcers or inflammatory bowel disease.
The pretreatment evaluation included a pelvic examination, common laboratory tests, chest X-ray, magnetic resonance imaging (MRI) of the pelvis at least to the level of the renal vessels, cystoscopy, intravenous pyelogram and sigmoidoscopy. Lymph node metastasis was evaluated using MRI without pathologic evaluation. Lymph nodes larger than 1 cm in the short-axis diameter were considered metastasis. This study was approved by the Institutional Review Board of Yonsei University College of Medicine.
Radiotherapy was delivered with a combination of external irradiation and high-dose rate intracavitary radiation by a remote afterloading system using iridium192 sources (Gamma-Med II). External whole-pelvis irradiation was performed with a dose of 1.8 Gy per fraction 5 times per week to a midline dose of 27.0-36.0 Gy. This was followed by high-dose rate intracavitary radiation with 6 insertions (twice per week) with a fractional dose of 5.0 Gy to a total dose of 30.0 Gy at point A. After high-dose rate intracavitary radiation, patients received a second course of external irradiation with central shielding up to a total external dose of 45.0-50.4 Gy. Parametrial or pelvic side wall boost with central shielding was used for patients with suspected residual parametrial disease after planned external irradiation and brachytherapy. The total dose to point A and point B was usually between 75 Gy and 90 Gy and 45 to 65 Gy, respectively, depending on the extent of parametrial disease.
During radiotherapy, cisplatin was given intravenously once a week at a dose of 40 mg/m2 of body surface area (BSA) with the total dose not exceeding 70 mg per week. In addition, patients in the study group were given rofecoxib as a radiosensitizer during chemoradiotherapy. Rofecoxib (Vioxx®, Merck & Co., Inc.) was started on day 1 of radiotherapy and continued daily during chemoradiotherapy (25 mg per os b.i.d., total 50 mg daily).
For chemotherapy, all patients were admitted to the hospital for 2 to 3 days. A 24-hour urine-creatinine clearance, pelvic exam, colposcopy, complete blood count with differential and platelet count, routine chemistry, chest X-ray, electrocardiogram and blood pressure measurement were taken weekly before each cycle of chemotherapy was started. Adverse events and severity were recorded according to the Common Toxicity Criteria version 2.0 (CTC ver. 2.0). Acute toxicities were defined as those that developed during CCRT or within 90 days after completion. Late toxicities were those occurring 90 days after completion of CCRT. If the patient experienced grade 3 or 4 gastrointestinal, renal, cardiac, pulmonary, hepatic or neurologic toxicity, chemotherapy was withheld until the toxicity had resolved to grade 0-2.
Objective responses were confirmed 6 weeks after the criteria for response were first met. Patients underwent MRI, colposcopy and pelvic exam after treatment to determine treatment response. The Response Evaluation Criteria in Solid Tumors (RECIST) guidelines were used to determine overall response. Complete response (CR) was defined as the disappearance of all target lesions; partial response (PR), at least a 30% decrease in the sum of longest diameter of target lesions; progressive disease (PD), at least a 20% increase in the sum of the longest diameter of target lesions; and stable disease (SD), neither sufficient shrinkage to qualify for PR nor increase to qualify for PD. Local treatment failure was defined as the persistence of local disease or local recurrence, and regional treatment failure was defined as the persistence, appearance or recurrence of regional nodal disease. The follow-up schedule was every month for the first 3 months, every 3 months for the first year, and every 6 months thereafter. Progression-free survival was determined from the date of the end of treatment to the date of disease progression. Overall survival was determined from the date of the end of treatment until death or the last date that the patient was reported alive. We investigated the cause of death and survival in 16 patients who were not followed up by telephone survey and data from the Korea National Cancer Information Center. Six patients were followed by telephone and the others were followed by data from the Korea National Cancer Information Center.
Although this was a retrospective study, a sample size was calculated with grade 3-4 acute toxicities including hematologic toxicities, vomiting or diarrhea, cardiac, pulmonary, hepatic and neurologic toxicity as the primary endpoint. Based on the acute toxicities data from Kim et al.,16 26% of patients who received CCRT with a weekly cisplatin regimen experienced grade 3-4 toxicities. Assuming 25% of the acute toxicity is considered tolerable, 45% or above of acute toxicities are considered excessive. A study design with a 1:1 allocation of study:control group with a significance level of 0.10 and a 2-sided, 2-sample t-test with a power of 80% would require 28 patient in each group to demonstrate a 20% aggravation in grade 3-4 acute toxicities. Statistical analysis was performed using SPSS ver. 12.0 (SPSS Inc., Chicago, IL, USA). Differences in clinicopathologic parameters, toxicity and pattern of treatment failure were evaluated by independent T test, Pearson chi-square test and Fisher's exact test. To estimate overall and progression-free survival, the Kaplan-Meier method was used. Survival difference was analyzed using a log-rank test. A difference was considered significant when the p-value was less than 0.05.
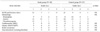
Between June 2002 and July 2004, 67 patients with locally advanced cervical cancer were treated with CCRT. Thirty of 67 patients received rofecoxib during chemoradiotherapy and were assigned to the study group. The control group consisted of 37 patients who received only CCRT. The median age of all patients was 50.6 years (range, 29 to 80 years). The median tumor size was 4.1 cm (range, 1.5 to 7.5 cm). Patient characteristics are summarized in Table 1. There were no statistically significant differences in clinicopathologic parameters between the two groups.
Seven (22.2%) patients failed to complete the planned treatment of rofecoxib. Four patients discontinued rofecoxib due to gastrointestinal toxicity such as gastritis, which did not affect the chemotherapy schedule for the patients. The others showed poor compliance with daily rofecoxib treatment. However, they completed the planned treatment with CCRT. The median treatment duration of rofecoxib in those patients was 35.5 days. Four patients in the study group could not complete their planned weekly cisplatin chemotherapy. Among them, 2 had grade 3/4 neutropenia and 1 experienced severe anemia. The other patient was an 80-year-old woman with an ECOG performance status of 3 during chemotherapy. After 2 cycles of chemotherapy, she refused additional treatment. Seven patients in the control group could not complete their planned chemotherapy. Four patients stopped chemotherapy due to grade 3/4 hematologic toxicity and 1 due to liver toxicity. One patient experienced systemic hypersensitivity reactions including skin rash, hypotension and dyspnea after the third cycle, and another was diagnosed with renal cell carcinoma in the fifth cycle of CCRT. Those two patients also stopped receiving chemotherapy.
All patients were examined for acute toxicities. Table 2 demonstrates treatment-related acute toxicities. There was no treatment-related death in either group. The most common grade 3 and 4 toxicities were hematologic. However, all patients who experienced severe hematologic toxicities recovered with supportive treatment. All cardiovascular complications observed in the study group were nonspecific T wave changes on electrocardiography. No patient in the study group developed myocardial infarction or angina pectoris. There were no significant differences in the frequency of acute toxicities between the two groups. Three patients in the study group and 6 in the control group stopped chemotherapy due to acute toxicities.
In the study group, 1 patient who showed persistent disease developed a vesicovaginal fistula 1 year after CCRT. There was a case of radiation proctitis combined with hematochezia requiring transfusion. In the control group, 3 cases of late toxicity were noted. Among these, there were 2 cases of radiation proctitis and 1 of small bowel perforation.
In the study group, 6 patients showed treatment failure. The treatment failure pattern distribution included 3 local failures and 3 regional failures. Two patients had SD and died at 14 and 29 months, respectively, after completion of CCRT. Another patient who was diagnosed with FIGO stage IVA cervical cancer showed partial response and died at 35 months. Other patients developed recurrent cervical cancer within 24 months. Two patients recurred in the left iliac lymph node and another in the left supraclavicular lymph node. Overall survival of those 3 patients was 44, 40 and 37 months, respectively. In addition, 3 patients developed other malignancies, such as non-small cell lung cancer, cholangiocellular carcinoma and pancreatic cancer, and died at 36, 34 and 35 months during follow-up, respectively.
In the control group, there was 1 case of PD, 2 of SD and 3 of recurrence. Six cases of treatment failures included 4 cases of local failures and 2 cases of regional failures. Two patients recurred in the iliac lymph nodes and 1 in the vaginal vault. All 6 patients who showed treatment failure died. In addition, 2 patients developed other malignancies during follow-up; one patient developed lung cancer after 69 months of follow-up and died at 77 months, and the other was diagnosed with renal cell carcinoma during the fifth cycle of CCRT and was cured after surgery (Table 3). All patients who died of secondary malignancy in this study were in complete remission of cervical cancer.
The median follow-up duration was 52.9±13.4 months in the study group and 63.9±19.3 months in the control group. Progression-free survival was 55.8±4.2 months in the study group and 69.7±4.3 months in the control group (Fig. 2A). Overall survival was 59.0±2.8 months in the study group and 71.6±3.6 months in the control group (Fig. 2B). There were no differences in progression-free and overall survival between the 2 groups (p=0.46 and p=0.30, respectively).
Based on the results of 5 randomized trials, CCRT is considered to be the primary treatment for locally advanced cervical cancer.2-6 Weekly cisplatin alone and cisplatin plus 5-fluorouracil were effective regimens for CCRT in these trials. In the present study, cisplatin was given intravenously once a week at a dose of 40 mg/m2 of body surface area (BSA), with the total dose not exceeding 70 mg per week during radiotherapy. Two of the randomized studies reported acute toxicities related to CCRT using weekly cisplatin. Keys et al. indicated that 64 of 183 patients in the CCRT group had grade 3/4 adverse effects that consisted of hematologic (21.3%) and gastrointestinal (GI) toxicities (14.2%). Grade 3/4 leucopenia and GI toxicities were also reported by Rose et al. in 23% and 12% of cases, respectively.4
Our data revealed that grade 2 GI toxicities in the study and control groups were 16.6% and 16.2%, respectively. Grade 3/4 neutropenia was observed in 13.3% of cases in the study group and 21.6% of cases in the control group. There were no significant differences in acute toxicities between the study and control groups. The daily dosage of rofecoxib in the present study was 50 mg, which is the typical dose for other diseases such as arthritis and primary dysmenorrhea. These results related to toxicities were comparable to those of other randomized trials, indicating that a conventional dose of rofecoxib does not elevate acute toxicities related to CCRT.
Although there is no study with which to compare our data on the toxicity of rofecoxib during radiotherapy or CCRT, two clinical phase II trials revealed toxicities of celecoxib combined with CCRT. Gaffney et al.17 reported a significant rate of acute GI toxicity in 43% (33/77) of patients in the RTOG 0128 study using celecoxib. The most frequently observed grade 3 and 4 toxicity was hematologic toxicity (40/77). Twenty patients showed grade 3 and 4 leucopenia. There were no cardiovascular complications related to the COX-2 inhibitor. Twenty percent of patients discontinued celecoxib due to toxicity. The author concluded that celecoxib at 400 mg twice daily together with CCRT produces a high incidence of acute toxicities. Another phase I-II trial using celecoxib as a radiosensitizer was performed by Herrera et al.18 The author demonstrated that the most common acute grade 3/4 toxicities were hematologic (4/31) and gastrointestinal (5/31). Three of 31 patients developed recto-vaginal fistulas as late complications. Performing interim analysis of acute and late toxicities, the authors found that celecoxib at 800 mg/day did not elevate acute toxicities, but did increase late toxicities. As a result, the celecoxib dose was reduced to 300 mg twice daily. Combining the results of these studies, 300 mg twice daily dose is considered to be a safer dose for a radiosensitizer in the treatment of locally advanced cervical cancer.
Our data on toxicities was superior to that of the RTOG 0128 study. Our lower rates of acute GI and hematologic toxicities might be due to differences in the disease stage of enrolled patients and chemotherapy regimens. The chemotherapy regimen used by Gaffney et al.17 was cisplatin at 75 mg/m2 to a maximal dose of 150 mg with 5-fluorouracil. A prospective randomized study, which was conducted to compare monthly fluorouracil plus cisplatin and weekly cisplatin-based CCRT for cervical cancer, demonstrated that acute hematologic and GI toxicities developed more frequently in patients who received monthly fluorouracil and cisplatin-based CCRT. A prospective study of celecoxib in which the authors used weekly cisplatin chemotherapy at 40 mg/m2 also reported an acute toxicity profile similar to ours.18
In terms of the treatment response, disease-free and overall survival, using rofecoxib as a radiosensitizer did not improve the prognosis of patients with locally advanced cervical cancer in the present study. However, it is difficult to make a conclusion regarding the efficacy of rofecoxib as a radiosensitizer because of the retrospective nature of our analysis. A phase II trial of rofecoxib in the treatment of cervical dysplasia also demonstrated that regression rates in the rofecoxib and placebo arm were not significant.19 There have been no reports indicating the efficacy of rofecoxib as a radiosensitizer in patients who received CCRT. Using celecoxib as a sensitizer, 24 of 78 patients had treatment failure, and 18 of those experienced loco-regional failure in the RTOG 0128 study.20 Another prospective study reported that 25 of 31 patients achieved a CR, and 5 of these developed recurrent disease.18 These prospective studies using celecoxib as a radiosensitizer showed that celecoxib did not improve patient survival.
There are several potential reasons why COX-2 inhibitors fail to improve patient survival and treatment results. Treatment using COX-2 inhibitors is a molecular target therapy. To evaluate the exact effects of COX-2 inhibitors, COX-2 expression needs to be measured in each patient, and it is preferable to recruit patients with cancer that strongly expresses COX-2. Additionally, the optimal dose of COX-2 inhibitor needed to act as a radiosensitizer is not known, and there are no available data on changes of COX-2 expression in cervical cancer after drug treatment.
There are several limitations in the present study. First of all, this is a retrospective study. To examine the toxicity and efficacy of rofecoxib as a radiosensitizer, a prospectively designed study would be more appropriate. The study population was heterogeneous in terms of disease stage compared with the small sample size. Finally, the toxicity induced by rofecoxib itself could not be examined due to study design. It is important to examine the adverse effects that might be aggravated by COX-2 inhibitor during CCRT, as well as the toxicity of rofecoxib itself.
Since it has been reported that COX-2 inhibitors lead to a significant reduction in the number of colorectal polyps in patients with familial adenomatous polyposis, several studies have been performed to evaluate the efficacy and toxicity of celecoxib in the treatment of uterine cervical cancer.17,18,20,21 Celecoxib and rofecoxib were the first 2 COX-2 inhibitors approved by the US Food and Drug Administration. However, there have been no reports on the use of rofecoxib in the treatment of cervical cancer.
To the best of our knowledge, this is the first study to evaluate the acute toxicity and efficacy of rofecoxib as a radiosensitizer for chemoradiation in the treatment of locally advanced cervical cancer. Notwithstanding the inherent drawbacks of a retrospective analysis, our data indicate that using rofecoxib at 25 mg twice a day during CCRT does not affect the acute toxicities of CCRT. Although rofecoxib is considered a safe drug if used only during CCRT, its benefit as a radiosensitizer should be further evaluated by a prospective study.
Figures and Tables
Fig. 2
Progression-free (A) and overall survival (B) with rofecoxib treatment. There were no differences in progression-free and overall survival between the 2 groups (p=0.46 and p=0.30, respectively).

References
1. Kim YT. Current status of cervical cancer and HPV infection in Korea. J Gynecol Oncol. 2009. 20:1–7.
2. Keys HM, Bundy BN, Stehman FB, Muderspach LI, Chafe WE, Suggs CL, et al. Cisplatin, radiation, and adjuvant hysterectomy compared with radiation and adjuvant hysterectomy for bulky stage IB cervical carcinoma. N Engl J Med. 1999. 340:1154–1161.
3. Morris M, Eifel PJ, Lu J, Grigsby PW, Levenback C, Stevens RE, et al. Pelvic radiation with concurrent chemotherapy compared with pelvic and para-aortic radiation for high-risk cervical cancer. N Engl J Med. 1999. 340:1137–1143.
4. Rose PG, Bundy BN, Watkins EB, Thigpen JT, Deppe G, Maiman MA, et al. Concurrent cisplatin-based radiotherapy and chemotherapy for locally advanced cervical cancer. N Engl J Med. 1999. 340:1144–1153.
5. Whitney CW, Sause W, Bundy BN, Malfetano JH, Hannigan EV, Fowler WC, et al. Randomized comparison of fluorouracil plus cisplatin versus hydroxyurea as an adjunct to radiation therapy in stage IIB-IVA carcinoma of the cervix with negative para-aortic lymph nodes: a Gynecologic Oncology Group and Southwest Oncology Group study. J Clin Oncol. 1999. 17:1339–1348.
6. Peters WA, Liu PY, Barrett RJ, Stock RJ, Monk BJ, Berek JS, et al. Concurrent chemotherapy and pelvic radiation therapy compared with pelvic radiation therapy alone as adjuvant therapy after radical surgery in high-risk early-stage cancer of the cervix. J Clin Oncol. 2000. 18:1606–1613.
7. Wang MT, Honn KV, Nie D. Cyclooxygenases, prostanoids, and tumor progression. Cancer Metastasis Rev. 2007. 26:525–534.
8. Lee JS, Choi YD, Lee JH, Nam JH, Choi C, Lee MC, et al. Expression of cyclooxygenase-2 in adenocarcinomas of the uterine cervix and its relation to angiogenesis and tumor growth. Gynecol Oncol. 2004. 95:523–529.
9. Ishiko O, Sumi T, Yoshida H, Matsumoto Y, Honda K, Deguchi M, et al. Association between overexpression of cyclooxygenase-2 and suppression of apoptosis in advanced cancer of the uterine cervix after cyclic balloon-occluded arterial infusion. Oncol Rep. 2001. 8:1259–1263.
10. Fujimoto J, Toyoki H, Sato E, Sakaguchi H, Jahan I, Alam SM, et al. Expression of cyclooxygenase-2 related to angiogenesis in uterine cervical cancers. J Biomed Sci. 2006. 13:825–832.
11. Ryu HS, Chang KH, Yang HW, Kim MS, Kwon HC, Oh KS. High cyclooxygenase-2 expression in stage IB cervical cancer with lymph node metastasis or parametrial invasion. Gynecol Oncol. 2000. 76:320–325.
12. Lindstrom AK, Stendahl U, Tot T, Lidström BM, Hellberg D. Predicting the outcome of squamous cell carcinoma of the uterine cervix using combinations of individual tumor marker expressions. Anticancer Res. 2007. 27:1609–1615.
13. Kim GE, Kim YB, Cho NH, Chung HC, Pyo HR, Lee JD, et al. Synchronous coexpression of epidermal growth factor receptor and cyclooxygenase-2 in carcinomas of the uterine cervix: a potential predictor of poor survival. Clin Cancer Res. 2004. 10:1366–1374.
14. Kim YB, Kim GE, Cho NH, Pyo HR, Shim SJ, Chang SK, et al. Overexpression of cyclooxygenase-2 is associated with a poor prognosis in patients with squamous cell carcinoma of the uterine cervix treated with radiation and concurrent chemotherapy. Cancer. 2002. 95:531–539.
15. Ferrandina G, Lauriola L, Distefano MG, Zannoni GF, Gessi M, Legge F, et al. Increased cyclooxygenase-2 expression is associated with chemotherapy resistance and poor survival in cervical cancer patients. J Clin Oncol. 2002. 20:973–981.
16. Kim YS, Shin SS, Nam JH, Kim YT, Kim YM, Kim JH, et al. Prospective randomized comparison of monthly fluorouracil and cisplatin versus weekly cisplatin concurrent with pelvic radiotherapy and high-dose rate brachytherapy for locally advanced cervical cancer. Gynecol Oncol. 2008. 108:195–200.
17. Gaffney DK, Winter K, Dicker AP, Miller B, Eifel PJ, Ryu J, et al. A Phase II study of acute toxicity for Celebrex (celecoxib) and chemoradiation in patients with locally advanced cervical cancer: primary endpoint analysis of RTOG 0128. Int J Radiat Oncol Biol Phys. 2007. 67:104–109.
18. Herrera FG, Chan P, Doll C, Milosevic M, Oza A, Syed A, et al. A prospective phase I-II trial of the cyclooxygenase-2 inhibitor celecoxib in patients with carcinoma of the cervix with biomarker assessment of the tumor microenvironment. Int J Radiat Oncol Biol Phys. 2007. 67:97–103.
19. Hefler LA, Grimm C, Speiser P, Sliutz G, Reinthaller A. The cyclooxygenase-2 inhibitor rofecoxib (Vioxx) in the treatment of cervical dysplasia grade II-III A phase II trial. Eur J Obstet Gynecol Reprod Biol. 2006. 125:251–254.
20. Gaffney DK, Winter K, Dicker AP, Miller B, Eifel PJ, Ryu J, et al. Efficacy and patterns of failure for locally advanced cancer of the cervix treated with celebrex (celecoxib) and chemoradiotherapy in RTOG 0128. Int J Radiat Oncol Biol Phys. 2007. 69:111–117.
21. Steinbach G, Lynch PM, Phillips RK, Wallace MH, Hawk E, Gordon GB, et al. The effect of celecoxib, a cyclooxygenase-2 inhibitor, in familial adenomatous polyposis. N Engl J Med. 2000. 342:1946–1952.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download