Abstract
Objective
We assessed the prognostic factors and the efficacy of adjuvant therapy and reviewed randomized studies carried out on patients receiving adjuvant therapy with early endometrial carcinoma.
Methods
One hundred and five patients that received primary surgical treatment for stage IB, IC and II endometrial cancer were enrolled in this study. The clinical outcomes were compared among the patients with variable prognostic factors and adjuvant treatments.
Results
One hundred and five patients fulfilled the eligibility criteria and 46 patients (43.8%) underwent adjuvant therapy. Disease recurrence occurred in nine patients within a median time of 24 months. Cervical involvement was an independent prognostic factor for the disease-free survival rates. Eight of 16 patients with FIGO stage II disease received adjuvant chemotherapy consisting of cisplatin and etoposide (or cyclophosphamide) or combined chemoradiation. The 5-year disease-free survival rate for these patients was 87.5%, a value significantly higher than for patients that received radiation therapy alone (30%).
Each year 15-20 per 100,000 women in Western countries are diagnosed with endometrial cancer, making it the most common gynecological cancer.1 The number of patients is increasing rapidly in Korea, where it is the third most common malignancy in women, affecting approximately 862 patients per year.2 The number of patients with recurrent endometrial cancer is also increasing. Approximately 10% to 15% of patients with early stage endometrial cancer will experience a recurrence.3,4
However, there is no consensus on the standard adjuvant therapy for stage I - II endometrial cancer. Because most women with endometrial cancer have early stage disease with a good prognosis, it has been difficult to identify the ideal protocol for adjuvant therapy in the small group of women who may be at increased risk for disease recurrence and possibly death. Historically, adjuvant radiation therapy has played a central role in the treatment of early-stage endometrial cancer. However, in recent large randomized studies, no significant survival benefit has been demonstrated with this method of treatment.3,5,6
Therefore, in the present study, we assessed the efficacy of adjuvant therapy and reviewed randomized studies carried out on patients receiving adjuvant therapy with early endometrial cancer in order to determine the optimal adjuvant treatment for patients with high-risk early stage endometrial cancer.
Between January 1990 and July 2007, all patients with FIGO stage IB, IC and II that underwent primary surgery with or without adjuvant therapy were selected for the present study. Non-endometrioid histological sub-types were not eligible for the analysis. The surgical stages were decided according to the 1988 International Federation of Gynecology and Obstetrics (FIGO) classification, based on the pathology findings.7 In general, we have routinely performed staging with systemic pelvic and paraaortic lymphadenectomy whenever technically possible. All cases were reviewed pathologically, and the stage and depth of invasion, grades and status of lymph-vascular space invasion were recorded. The treatment protocol included postoperative adjuvant therapy consisting of chemotherapy, chemoradiation and radiation in patients with at least one of the following unfavorable risk factors: histological grade 2-3, invasion of the outer half of the myometrium, isthmus-cervical extension, and lymph-vascular space invasion. Adjuvant treatment was not provided in some cases because of medical complications or patient refusal.
During the time of the study, the chemotherapy group received cisplatin (or carboplatin), etoposide (or cyclophosphamide) with or without adriamycin every four weeks for six courses. Pelvic irradiation was given at 45 to 50 Gy within four to six weeks, with 9 to 10 Gy of irradiation per week. The chemoradiation group received chemotherapy first and subsequently received pelvic irradiation.
When toxicity (World Health Organization Toxicity Guidelines) was recognized, the chemotherapy was paused until the symptoms resolved. The following doses were reduced or alternative drugs were used. All patients were followed with physical and/or imaging studies every three to four months during the first three years and every six months thereafter at our institution.
All statistical analyses were performed using SPSS 14.0 for Window (Release 14.02). Survival rates were calculated by the Kaplan-Meier method. The log rank test was used to test for survival differences. Factors found to be significant were then applied to a stepwise Cox multivariate proportional hazard model to determine their prognostic value. All reported p-values are based on two-sided tests with a p<0.05 accepted as significant.
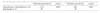
Between January 1990 and July 2007, a total of 105 patients were considered eligible for this study; 59 received no adjuvant therapy, 16 received chemotherapy, 20 received radiotherapy, and 10 received chemoradiation. Table 1 lists the distribution of patients according to age, FIGO stage, grade, degree of myometrial invasion, cervical involvement, and lymph-vascular space involvement. The patients varied in age from 22 to 73 (mean: 52 years). The mean follow-up time was 59 months (range 7 to 197 months).
The 5-year disease-free rate was 88.9% and the overall survival rate was 94.8%. Disease recurrence occurred in nine patients (8.6%), locoregional disease in three, and distant disease in six (Table 2); the median time to recurrence was 24 months (range 4 to 45 months). The univariate analysis showed (Table 3) that histological grade, presence of myometrial invasion, cervical involvement, and lymph-vascular space involvement were all significant factors for the diseasefree survival rate; the cervical involvement and lymph-vascular space involvement were also significant factors involved in the overall survival rate. The multivariate analysis using the Cox multivariate proportional hazard model showed that cervical involvement was the only independent factor that was significantly associated with the disease-free and overall survival rates (Table 4). Among 16 patients with cervical involve ment, a statistically significant difference was found for the disease-free and overall survival rates between patients that received adjuvant chemotherapy or chemoradiation, and patients that received radiotherapy (Table 5).
The toxicities associated with the adjuvant chemotherapy were mild to moderate. Treatment was halted temporarily in five patients (23%) at two to three weeks as a result of grade 2-3 hematologic toxicities. Bowel obstruction was the main complication in the radiotherapy group. However, there was no treatment-related death in all eligible patients.
Stage I and II, intermediate or high risk endometrial cancers are known to have a good prognosis. The overall survival rate is 76-85% for Stage I and 46-85% for stage II.3,5,8,9 It is generally accepted that patients with FIGO stage IA and IB, grade 1 or 2 tumors, do not require additional therapy. However, given the presence of variable prognostic factors, recurrences occur and the survival rate for relapsed patients is poor.9-11 Therefore, the decision to provide adjuvant treatment depends on the presence of certain risk factors.12 These treatments include radiotherapy, chemotherapy and hormonal therapy.
The known prognostic factors for the disease-free survival of patients with endometrial carcinoma are: tumor stage, depth of invasion, tumor grade, histological type, age, lymph-vascular space invasion, menopausal state, and progesterone receptor activity.4,13-15 In the present study, we analyzed the factors predictive of pelvic or distant recurrence in a series of 105 patients with FIGO stage I or II, high risk endometrial cancer. We found an overall recurrence rate of 8.5%. This recurrence rate compares favorably with the rates published in other studies, ranging from 4 to 19% in early-stage patients.3,9,16 In our study, cervical involvement was the most relevant independent prognostic factor in endometrial cancer that was histologically confined to the uterus. The fact that we found only this factor as an independent prognostic factor in the women with stage I and II high-risk endometrial cancer may be due to the relatively small number of patients with recurrent disease, limiting the statistical power.
Various randomized trials have shown that radiotherapy decreased the risk of pelvic and local recurrence in patients with early stage endometrial carcinoma.3,5,6,17 However, there is uncertainty as to whether adjuvant radiotherapy improves overall survival. Aalders et al, the Postoperative Radiation Therapy in Endometrial Cancer (PORTEC) trial and the Gynecological Oncology Group-99 suggested that for the high-risk category of patients, radiotherapy decreases local recurrence but, this did not reduce the risk of death.3,5,6 In addition, the recent adjuvant radiotherapy studies from the National Cancer Institute of Canada Clinical Trial Group (CAN-NCIS-En5) and the MRC/NCRI (UK) ASTEC did not show a survival benefit for adjuvant radiotherapy in women with early stage endometrial carcinoma.18 A Dutch multicenter randomized phase III trial (PORTEC 2 trial) concluded that since the patient reported that the quality of life, after vaginal brachytherapy, was shown to be better than after external beam radiation therapy, vaginal brachytherapy should be considered for patients with high risk early stage endometrial carcinoma.19
In our present study, the five year disease-free survival rate after radiotherapy was 71%. Although it was lower than the surgery alone group, the multivariate analysis confirmed that there was no real difference between the radiotherapy group and the surgery alone group. This result may have been due to the fact that we performed radiotherapy in patients with a poor prognosis compared to the surgery alone group.
Traditionally endometrial carcinoma has been thought to be a rather chemotherapy insensitive tumor. However, since the GOG trial (GOG 122) showed that chemotherapy had a significantly better OS and PFS than whole abdominal radiation in patients with advanced endometrial carcinoma, this view has changed.20 The choice of chemotherapeutic agents that might be effective has therefore been selected based on the trials of drugs used in patients with advanced or recurrent disease. Historically, adriamycin and platinum, and more recently paclitaxel, have been the favored agents.21-23 The GOG trial (GOG 209) is currently comparing paclitaxel-carboplatin with paclitaxel-cisplatic-adriamycin and G-CSF chemotherapy in women with advanced or metastatic endometrial cancer. In Japan, there are several published data about the efficacy of adjuvant chemotherapy in patients with early endometrial cancer.24-26 However, there have been no published randomized trials looking solely at the role of adjuvant chemotherapy in women with endometrial carcinoma.
In our study, we administered cisplatin (or carboplatin), etoposide (or cyclophosphamide) with or without adriamycin every four weeks for six courses. The five year disease-free survival rate of the chemotherapy group was 91.7%, which was better than the radiotherapy group; however, the difference was not statistically significant. The relatively small number of patients with recurrent disease might have limited the statistical power.
Only two randomized trials have compared chemotherapy with pelvic radiotherapy for adjuvant treatment in women with intermediate and high risk endometrial cancer. These studies failed to show a difference in either the overall or disease-free survival. However, the cumulative incidence of local regional recurrence was lower in patients receiving radiotherapy, and distant relapse was lower in patients given adjuvant chemotherapy.27,28 Therefore, there is some justification for the combination of adjuvant chemotherapy and radiotherapy either concurrently or sequentially in high risk endometrial cancer patients. The RTOG 9708 and EORTC 55991 trials were performed to determine the role of adjuvant chemotherapy in addition to external beam radiotherapy.29,30 The combined adjuvant chemotherapy and radiotherapy showed additive effects for the local and distant control of endometrial cancer. In our retrospective study, a statistically significant difference was found in the disease-free and overall survival rate between patients who received adjuvant chemotherapy or chemoradiation, and those that received radiotherapy. Currently a randomized phase III trial comparing concurrent chemoradiation and adjuvant chemotherapy with pelvic radiation alone, in high risk and advanced stage endometrial cancer (PORTEC 3 trial) patients, is recruiting participants.
The results of this study showed that cervical involvement was an independent prognostic factor in patients with endometrial cancer confined to the uterus. In addition, adjuvant chemotherapy or combination of chemo-radiotherapy appeared to significantly improve patient survival. The results of phase III randomized controlled trials are required to establish standard adjuvant therapy for women with high-risk early stage endometrial cancer.
References
1. Parkin DM, Bray F, Ferlay J, Pisani P. Global cancer statistics,2002. CA Cancer J Clin. 2005. 55:74–108.
2. SOG Gynecologic Oncology Committee. Annual report of gynecologic cancer registry program in Korea for 2004 (Jan. 1st, 2004-Dec. 31st, 2004). Korean J Obstet Gynecol. 2007. 50:28–78.
3. Creutzberg CL, van Putten WL, Koper PC, Lybeert ML, Jobsen JJ, Warlam-Rodenhuis CC, et al. Surgery and postoperative radiotherapy versus surgery alone for patients with stage-1 endometrial carcinoma: Multicentre randomised trial.PORTEC Study Group. Post Operative Radiation Therapy in Endometrial Carcinoma. Lancet. 2000. 355:1404–1411.
4. Morrow CP, Bundy BN, Kurman RJ, Creasman WT, Heller P, Homesley HD, et al. Relationship between surgical-pathological risk factors and outcome in clinical stage I and II carcinoma of the endometrium: A Gynecologic Oncology Group study. Gynecol Oncol. 1991. 40:55–65.
5. Aalders J, Abeler V, Kolstad P, Onsrud M. Postoperative external irradiation and prognostic parameters in stage I endometrial carcinoma: Clinical and histopathologic study of 540 patients. Obstet Gynecol. 1980. 56:419–427.
6. Keys HM, Roberts JA, Brunetto VL, Zaino RJ, Spirtos NM, Bloss JD, et al. A phase III trial of surgery with or without adjunctive external pelvic radiation therapy in intermediate risk endometrial adenocarcinoma: A Gynecologic Oncology Group study. Gynecol Oncol. 2004. 92:744–751.
7. FIGO stages: 1988 revision. Gynecol Oncol. 1989. 35:125–127.
8. Sartori E, Gadducci A, Landoni F, Lissoni A, Maggino T, Zola P, et al. Clinical behavior of 203 stage II endometrial cancer cases: The impact of primary surgical approach and of adjuvant radiation therapy. Int J Gynecol Cancer. 2001. 11:430–437.
9. Descamps P, Calais G, Moire C, Bertrand P, Castiel M, Le Floch O, et al. Predictors of distant recurrence in clinical stage I or II endometrial carcinoma treated by combination surgical and radiation therapy. Gynecol Oncol. 1997. 64:54–58.
10. Kuten A, Grigsby PW, Perez CA, Fineberg B, Garcia DM, Simpson JR. Results of radiotherapy in recurrent endometrial carcinoma: A retrospective analysis of 51 patients. Int J Radiat Oncol Biol Phys. 1989. 17:29–34.
11. Vavra N, Denison U, Kucera H, Barrada M, Kurz C, Salzer H, et al. Prognostic factors related to recurrent endometrial carcinoma following initial surgery. Acta Obstet Gynecol Scand. 1993. 72:205–209.
12. Lybeert ML, van Putten WL, Brolmann HA, Coebergh JW. Postoperative radiotherapy for endometrial carcinoma. Stage I. Wide variation in referral patterns but no effect on long-term survival in a retrospective study in the southeast Netherlands. Eur J Cancer. 1998. 34:586–590.
13. Creasman WT. Endometrial cancer: incidence, prognostic factors, diagnosis, and treatment. Semin Oncol. 1997. 24:1 Suppl 1. S1–S140. S141–S150.
14. DiSaia PJ, Creasman WT, Boronow RC, Blessing JA. Risk factors and recurrent patterns in Stage I endometrial cancer. Am J Obstet Gynecol. 1985. 151:1009–1015.
15. Grigsby PW, Perez CA, Kuten A, Simpson JR, Garcia DM, Camel HM, et al. Clinical stage I endometrial cancer: Prognostic factors for local control and distant metastasis and implications of the new FIGO surgical staging system. Int J Radiat Oncol Biol Phys. 1992. 22:905–911.
16. Mariani A, Webb MJ, Keeney GL, Lesnick TG, Podratz KC. Surgical stage I endometrial cancer: Predictors of distant failure and death. Gynecol Oncol. 2002. 87:274–280.
17. Johnson N, Cornes P. Survival and recurrent disease after postoperative radiotherapy for early endometrial cancer: Systematic review and meta-analysis. BJOG. 2007. 114:1313–1320.
18. Lukka H, Whelan T, Blake P, Swart AM, Orton J, Branson A, et al. Adjuvant external beam radiotherapy in the treatment of endometrial cancer: Results of the randomized MRC ASTEC and NCIC CTG EN.5 Trials, a systematic review and meta-analysis. Int J Radiat Oncol Biol Phys. 2008. 72:1 Suppl 1. S353–S354.
19. Nout RA, Putter H, Jurgenliemk-Schulz IM, Jobsen JJ, Lutgens LC, van der Steen-Banasik EM, et al. Vaginal brachytherapy versus external beam pelvic radiotherapy for high-intermediate risk endometrial cancer: Results of the randomized PORTEC, 2 trial [abstract]. J Clin Oncol. 2008. 26(15S):Abstract LBA5503.
20. Randall ME, Spirtos NM, Dvoretsky P. Whole abdominal radiotherapy versus combination chemotherapy with doxorubicin and cisplatin in advanced endometrial carcinoma (phase III): Gynecologic Oncology Group Study No. 122. J Natl Cancer Inst Monogr. 1995. (19):13–15.
21. Humber CE, Tierney JF, Symonds RP, Collingwood M, Kirwan J, Williams C, et al. Chemotherapy for advanced, recurrent or metastatic endometrial cancer: A systematic review of Cochrane collaboration. Ann Oncol. 2007. 18:409–420.
22. Fleming GF, Brunetto VL, Cella D, Look KY, Reid GC, Munkarah AR, et al. Phase III trial of doxorubicin plus cisplatin with or without paclitaxel plus filgrastim in advanced endometrial carcinoma: A Gynecologic Oncology Group Study. J Clin Oncol. 2004. 22:2159–2166.
23. Sorbe B, Andersson H, Boman K, Rosenberg P, Kalling M. Treatment of primary advanced and recurrent endometrial carcinoma with a combination of carboplatin and paclitaxel-long-term follow-up. Int J Gynecol Cancer. 2008. 18:803–808.
24. Hirai M, Hirono M, Oosaki T, Hayashi Y, Yoshihara T, Itami M. Adjuvant chemotherapy in stage I uterine endometrial carcinoma. Int J Gynaecol Obstet. 2002. 78:37–44.
25. Aoki Y, Watanabe M, Amikura T, Obata H, Sekine M, Yahata T, et al. Adjuvant chemotherapy as treatment of high-risk stage I and II endometrial cancer. Gynecol Oncol. 2004. 94:333–339.
26. Kodama J, Seki N, Hiramatsu Y. Chemotherapy for high-risk early-stage endometrial cancer. Curr Opin Obstet Gynecol. 2007. 19:42–47.
27. Maggi R, Lissoni A, Spina F, Melpignano M, Zola P, Favalli G, et al. Adjuvant chemotherapy vs radiotherapy in high-risk endometrial carcinoma: Results of a randomised trial. Br J Cancer. 2006. 95:266–271.
28. Susumu N, Sagae S, Udagawa Y, Niwa K, Kuramoto H, Satoh S, et al. Randomized phase III trial of pelvic radiotherapy versus cisplatin-based combined chemotherapy in patients with intermediate- and high-risk endometrial cancer: A Japanese Gynecologic Oncology Group study. Gynecol Oncol. 2008. 108:226–233.
29. Hogberg T, Rosenberg P, Kristensen G, de Oliveira CF, de Pont Christensen R, Sorbe B, et al. A randomized phase-III study on adjuvant treatment with radiation (RT){+/-} chemotherapy (CT) in early-stage high-risk endometrial cancer (NSGO-EC-9501/EORTC 55991) [abstract]. J Clin Oncol. 2007. 25(18S):Abstract 5503.
30. Greven K, Winter K, Underhill K, Fontenesci J, Cooper J, Burke T. Final analysis of RTOG 9708: Adjuvant postoperative irradiation combined with cisplatin/paclitaxel chemotherapy following surgery for patients with high-risk endometrial cancer. Gynecol Oncol. 2006. 103:155–159.




 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download