Kikuchi-Fujimoto disease, also called histiocytic necrotizing lymphadenitis, typically presents as fevers and cervical lymphadenopathy. It is more prevalent in Asia, and has been reported to have a female predominance (female to male ratio, 2.9:1) [1]. The syndrome is generally self-limited, and findings commonly include fevers, lymphadenopathy, rash, arthritis, and hepatosplenomegaly. It is postulated that the pathophysiology involves an immune response of T lymphocytes and histiocytes to infectious agents, leading to apoptotic cell death [23]. We present a rare case of Kikuchi-Fujimoto disease complicated by recurrent episodes of aseptic meningitis and discuss the need for disease-modifying treatment.
A 28-year-old woman presented to the emergency room with fever, chills and left-sided neck swelling that began four days prior. The patient reported a past medical history of two episodes of meningitis at the ages of 12 months and 18 years without an infectious etiology, leading to no neurological sequelae. She had no chronic illnesses and was not on any daily medications. The patient denied any recent travel or outdoor activities. Family and social history were noncontributory.
Initial vital signs revealed temperature of 39.4℃, blood pressure of 110/86 mmHg, heart rate of 70 bpm, respiratory rate of 20/minute and SpO2 of 99% on room air. A general examination revealed swollen lymph nodes on the left side of the neck, but no rash or swollen joints. Laboratory results were positive for a mild leukopenia (white blood cell [WBC] count of 3,850: laboratory range, 4,000~10,000/µL), increased C-reactive protein of 3.42 (laboratory range, 0~0.5 mg/dL) and erythrocyte sedimentation rate of 49 (laboratory range, 0~20 mm/hr).
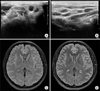
Ultrasonography of the neck was performed, which revealed multiple enlarged lymph nodes along the left side of the neck with increased echogenicity of perinodal fat, indicating an acute lymphadenitis (Figure 1A and 1B). While we did not pursue biopsy in the setting of rapid resolution of lymphadenopathy over the course of 48 to 72 hours, clinical presentation, medical history and ultrasonography findings pointed towards a diagnosis of Kikuchi-Fujimoto disease and she was admitted for further workup and symptom management. During her hospital stay, aspartate aminotransferase and alanine aminotransferase levels increased and reached peak values of 163 and 159 IU/L, respectively, on the fifth day. An ultrasound of the abdomen was performed, revealing findings suggestive of mild fatty liver.
Despite receiving conservative management including intravenous ketorolac and acetaminophen, the patient continued to have persistent fever during her admission and developed headache. Neurological examination did not reveal signs of meningeal irritation. Magnetic resonance imaging of the brain was conducted, which revealed diffuse leptomeningeal enhancement seen on post-contrast T2-weighted image (Figure 1D). A lumbar puncture was then performed, which revealed a normal opening pressure of 16 cmH2O, an increased WBC count of 31 (laboratory range, 0~5/µL) with an increased protein level of 113 (laboratory range, 15~45 mg/dL). Immunoglobulin (Ig) G level of the cerebrospinal fluid (CSF) was found to be elevated at 20.8 mg/dL (laboratory range, 0~3.4 mg/dL). Infectious workup of the CSF was negative. Intravenous methylprednisolone 250 mg was subsequently given, and the patient's headache improved dramatically and fever promptly subsided.
The patient was seen in rheumatologic consultation and investigation of serum antibodies (anti-nuclear antibodies [ANA], anti-neutrophil cytoplasmic antibody [ANCA], anti-cyclic citrullinated peptide [CCP], anti-double-stranded [ds] DNA, anti-ribonucleoprotein [RNP], anti-Sjögren's syndrome antibodies [SS]-A, SS-B, anti-topoisomerase I (Scl70) antibody, anti-Jo1, anti-phospholipid, anti-cardiolipin antibodies) was performed to rule out an autoimmune disorder. There were no positive antibodies found. A serum Ig panel revealed an elevated IgE level at 419 (laboratory values, 0~100 kU/L). The patient was discharged home with oral corticosteroids (methylprednisolone 7.5 mg BID) to prevent further relapses. She remained asymptomatic following her discharge from the hospital and has been in remission since.
Our case is a rare example of recurrent aseptic meningitis in a young woman with findings consistent with Kikuchi-Fujimoto disease, who experienced a total of three episodes of meningitis preceded by fever and neck swelling, over the course of 23 years. While lymph node biopsy results are lacking in this case, the history, clinical presentation and ultrasound findings are consistent with Kikuchi-Fujimoto disease. Aseptic meningitis, which our patient experienced recurrently, is an extremely rare clinical manifestation of Kikuchi-Fujimoto disease [45]. While it is generally considered to be benign, symptoms may result in severe headache and persistent fever such as in our patient, whose symptoms and fevers only subsided following intravenous corticosteroid therapy. Therefore, it may be worthwhile to consider cerebrospinal fluid investigation or brain imaging in a patient with Kikuchi-Fujimoto disease presenting with persistent fever and headache, so as to include corticosteroids in the armamentarium. Factors related to poor prognosis include absence of atypical lymphocytes in peripheral blood and low ratio of blastic cells (<70%) in lymph node specimens [6]. Although this syndrome is usually considered to be self-limiting, reports suggest that the syndrome may also present with atypical features such as extranodal involvement (renal failure, uveitis, testitis, etc.). Surprisingly, to date there are no guidelines regarding disease management and recurrence, despite numerous reports of extranodal involvement in Kikuchi-Fujimoto disease. Therefore, future efforts on a larger scale are required to study this disorder in more detail with special attention to preventing relapses, with the potential use of immuno-modulating therapy relevant to the underlying immuno-pathophysiology.
Figures and Tables
Figure 1
Ultrasound imaging (left aspect of the neck) and magnetic resonance imaging of the brain. Increased echogenicity of conglomerated cervical lymph nodes (arrows) are noted on (A) axial and (B) longitudinal planes (asterisk, sternocleidomastoid muscle). T2-weighted fluid-attenuated inversion recovery sequence images are shown, (C) pre-and (D) post-contrast administration. (D) Diffuse leptomeningeal enhancement is noted.
References
1. Jung IY, Ann HW, Kim JJ, Lee SJ, Kim J, Seong H, et al. The incidence and clinical characteristics by gender differences in patients with Kikuchi-Fujimoto disease. Medicine (Baltimore). 2017; 96:e6332.
2. Iguchi H, Sunami K, Yamane H, Konishi K, Takayama M, Nakai Y, et al. Apoptotic cell death in Kikuchi's disease: a TEM study. Acta Otolaryngol Suppl. 1998; 538:250–253.
3. Ohshima K, Shimazaki K, Kume T, Suzumiya J, Kanda M, Kikuchi M. Perforin and Fas pathways of cytotoxic T-cells in histiocytic necrotizing lymphadenitis. Histopathology. 1998; 33:471–478.
4. Komagamine T, Nagashima T, Kojima M, Kokubun N, Nakamura T, Hashimoto K, et al. Recurrent aseptic meningitis in association with Kikuchi-Fujimoto disease: case report and literature review. BMC Neurol. 2012; 12:112.
5. Sato Y, Kuno H, Oizumi K. Histiocytic necrotizing lymphadenitis (Kikuchi's disease) with aseptic meningitis. J Neurol Sci. 1999; 163:187–191.
6. Marunaka H, Orita Y, Tachibana T, Miki K, Makino T, Gion Y, et al. Kikuchi-Fujimoto disease: evaluation of prognostic factors and analysis of pathologic findings. Acta Otolaryngol. 2016; 136:944–947.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download