Abstract
Objective
This study was designed to identify the prevalence and clinical features of hyperuricemia in Gwangju and Jeonnam territories.
Methods
We enrolled 2309 participants who underwent health examinations at Chosun University Hospital from January 2008 to June 2010. All participants were free from gout, diabetes, hypertension, rheumatoid arthritis, dyslipidemia, cerebral infarction, cardiovascular disease, cancer, asthma, and autoimmune disease. Hyperuricemia was defined as ≥7 mg/dL in males and ≥6 mg/dL in females. Metabolic syndrome was defined using the International Diabetes Federation (IDF) criteria, which were revised in 2005. Clinical profiles were investigated, including age, waist circumference (WC), body- mass index (BMI), fasting glucose, HbA1c, triglycerides, total cholesterol, high-density lipoprotein cholesterol (HDL-C), low-density lipoprotein cholesterol (LDL-C), blood pressure (BP), high-sensitivity-C-reactive protein (hs-CRP), homocysteine, fibrinogen, total bilirubin, gamma-glutamyl transferase (r-GT), aspartate aminotransferase/alanine aminotransferase (AST/ALT), alcohol consumption, smoking and exercise.
Results
The overall prevalence of hyperuricemia was 9.8% among our study. The condition was more common in males than in females (15.0% vs 4.1%). Uric acid concentration was correlated with WC, BMI, BP, triglycerides, total cholesterol, hs-CRP, and r-GT (p<0.05). Additionally, among males, uric acid concentration was correlated with WC. The prevalence of metabolic syndrome increased when uric acid concentration increased. Males with hyperuricemia had 2.3-fold higher risk of metabolic syndrome (odds ratio (OR)=2.33). Female with hyperuricemia had 2.8-fold higher risk of metabolic syndrome (OR=2.78) as compared to those without hyperuricemia.
Figures and Tables
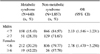
Table 2
The association of hyperuricemia and other characteristics features according to the gender of the participants

Table 3
Multiple logistic regression models to determine the risk of these characteristic factors of hyperuricemia according to gender

References
1. Smith EU, Díaz-Torné C, Perez-Ruiz F, March LM. Epidemiology of gout: an update. Best Pract Res Clin Rheumatol. 2010. 24:811–827.
2. Vitart V, Rudan I, Hayward C, Gray NK, Floyd J, Palmer CN, et al. SLC2A9 is a newly identified urate transporter influencing serum urate concentration, urate excretion and gout. Nat Genet. 2008. 40:437–442.
3. Puig JG, Martínez MA, Mora M, Fraile JM, Montoya F, Torres RJ. Serum urate, metabolic syndrome, and cardiovascular risk factors. A population-based study. Nucleosides Nucleotides Nucleic Acids. 2008. 27:620–623.
4. Sarafidis PA, Nilsson PM. The metabolic syndrome: a glance at its history. J Hypertens. 2006. 24:621–626.
5. Puig JG, Martínez MA. Hyperuricemia, gout and the metabolic syndrome. Curr Opin Rheumatol. 2008. 20:187–191.
6. Feig DI, Johnson RJ. Hyperuricemia in childhood primary hypertension. Hypertension. 2003. 42:247–252.
7. Nakagawa T, Tuttle KR, Short RA, Johnson RJ. Hypothesis: fructose-induced hyperuricemia as a causal mechanism for the epidemic of the metabolic syndrome. Nat Clin Pract Nephrol. 2005. 1:80–86.
8. Niskanen LK, Laaksonen DE, Nyyssönen K, Alfthan G, Lakka HM, Lakka TA, et al. Uric acid level as a risk factor for cardiovascular and all-cause mortality in middle-aged men: a prospective cohort study. Arch Intern Med. 2004. 164:1546–1551.
9. Eckel RH, Grundy SM, Zimmet PZ. The metabolic syndrome. Lancet. 2005. 365:1415–1428.
10. Hjortnaes J, Algra A, Olijhoek J, Huisman M, Jacobs J, van der Graaf Y, et al. Serum uric acid levels and risk for vascular diseases in patients with metabolic syndrome. J Rheumatol. 2007. 34:1882–1887.
11. Ozsahin AK, Gokcel A, Sezgin N, Akbaba M, Guvener N, Ozisik L, et al. Prevalence of the metabolic syndrome in a Turkish adult population. Diabetes Nutr Metab. 2004. 17:230–234.
12. Ford ES, Li C, Cook S, Choi HK. Serum concentrations of uric acid and the metabolic syndrome among US children and adolescents. Circulation. 2007. 115:2526–2532.
13. Kim EH, Jeon K, Park KW, Kim HJ, Ahn JK, Jeon CH, et al. The prevalence of gout among hyperuricemic population. J Korean Rheum Assoc. 2004. 11:7–13.
14. Miao Z, Li C, Chen Y, Zhao S, Wang Y, Wang Z, et al. Dietary and lifestyle changes associated with high prevalence of hyperuricemia and gout in the Shandong coastal cities of Eastern China. J Rheumatol. 2008. 35:1859–1864.
15. Saag KG, Choi H. Epidemiology, risk factors, and lifestyle modifications for gout. Arthritis Res Ther. 2006. 8:Suppl 1. S2.
16. Roddy E, Zhang W, Doherty M. The changing epidemiology of gout. Nat Clin Pract Rheumatol. 2007. 3:443–449.
17. Lee SJ, Terkeltaub RA, Kavanaugh A. Recent developments in diet and gout. Current Opinions in Rheumatology. 2006. 18:193–198.
18. Nan H, Qiao Q, Dong Y, Gao W, Tang B, Qian R, et al. The prevalence of hyperuricemia in a population of the coastal city of Qingdao, China. J Rheumatol. 2006. 33:1346–1350.
19. Uaratanawong S, Suraamornkul S, Angkeaw S, Uaratanawong R. Prevalence of hyperuricemia in Bangkok population. Clin Rheumatol. 2011. 30:887–893.
20. Yoo B. Serum uric acid levels in Korean adult population and their correlates. J Korean Rheum Assoc. 1995. 2:60–68.
21. Gagliardi AC, Miname MH, Santos RD. Uric acid: A marker of increased cardiovascular risk. Atherosclerosis. 2009. 202:11–17.
22. Oh J, Won HY, Kang SM. Uric acid and cardiovascular risk. N Engl J Med. 2009. 360:539–540.
23. Chin HJ, Na KY, Kim Y, Chae DW, Kim S. The impact of uric acid and metabolic syndrome on the incidence of hypertention in a Korean population. Korean J Med. 2007. 73:58–66.
24. Nilssen O, Førde OH, Brenn T. The Tromsø Study. Distribution and population determinants of gamma-glutamyltransferase. Am J Epidemiol. 1990. 132:318–326.
25. Wannamethee G, Ebrahim S, Shaper AG. Gamma-glutamyltransferase: determinants and association with mortality from ischemic heart disease and all causes. Am J Epidemiol. 1995. 142:699–708.
26. Perry IJ, Wannamethee SG, Shaper AG. Prospective study of serum gamma-glutamyltransferase and risk of NIDDM. Diabetes Care. 1998. 21:732–737.
27. Karp DR, Shimooku K, Lipsky PE. Expression of gamma-glutamyl transpeptidase protects ramos B cells from oxidation-induced cell death. J Biol Chem. 2001. 276:3798–3804.
28. Carlisle ML, King MR, Karp DR. Gamma-glutamyl transpeptidase activity alters the T cell response to oxidative stress and Fas-induced apoptosis. Int Immunol. 2003. 15:17–27.
29. Lee DS, Evans JC, Robins SJ, Wilson PW, Albano I, Fox CS, et al. Gamma glutamyl transferase and metabolic syndrome, cardiovascular disease, and mortality risk: the Framingham Heart Study. Arterioscler Thromb Vasc Biol. 2007. 27:127–133.
30. Devaraj S, Valleggi S, Siegel D, Jialal I. Role of C-reactive protein in contributing to increased cardiovascular risk in metabolic syndrome. Curr Atheroscler Rep. 2010. 12:110–118.
31. Welsh P, Woodward M, Rumley A, Lowe G. Associations of plasma pro-inflammatory cytokines, fibrinogen, viscosity and C-reactive protein with cardiovascular risk factors and social deprivation: the fourth Glasgow MONICA study. Br J Haematol. 2008. 141:852–861.
32. Lindahl B, Toss H, Siegbahn A, Venge P, Wallentin L. Markers of myocardial damage and inflammation in relation to long-term mortality in unstable coronary artery disease. FRISC Study Group. Fragmin during Instability in Coronary Artery Disease. N Engl J Med. 2000. 343:1139–1147.
33. Rho YH, Woo JH, Choi SJ, Lee YH, Ji JD, Song GG. Association between serum uric acid and the Adult Treatment Panel III-defined metabolic syndrome: results from a single hospital database. Metabolism. 2008. 57:71–76.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download