Abstract
Poor adherence to asthma medication treatment is a dilemma as it decreases the chance of achieving and maintaining a proper asthma control. Another dilemma is that there seems to be a small range of functional interventions that enhance adherence to long-term medication treatments. The aim was to review the last five years of published educational interventions for improving adherence to asthma medication. Through systematic database searches 20 articles were identified, which matched the inclusion criteria and described educational interventions to improve asthma self-management including adherence. The current review showed that addressing unintentional non-adherence in terms of incorrect inhaler technique by recurrent education improved the technique among many patients, but not among all. Phoning patients, as a means to remove medication beliefs as adherence barriers, seemed to be an effective educational strategy, shown as increased adherence. Involving patients in treatment decisions and individualising or tailoring educational support also seemed to have favourable effect on adherence. To conclude, addressing specific adherence barriers such as poor inhaler technique or medication beliefs could favour adherence. To change adherence behavior, the current review proposes that educational adherence support should be a collaborative effort between the patient and the health-care professional based on each individual patient's needs and patient factors, including elements such as personality traits.
A plethora of studies have reported about poor adherence to asthma medication treatment [1-4]. As an example, an overall adherence to asthma medication of 22% in a sample of 5,500 persons with asthma was reported in one study [5]. People with asthma, who display poor medication adherence, most likely run increased risk of experiencing poor asthma outcomes [4]. The chance of achieving and maintaining the goal of modern asthma treatment: a well-controlled asthma, may also diminish [6]. There are arguments stating that the discovery of effective methods to improve adherence almost certainly would have a more advantageous influence on health than any treatment. However, there seems to be a lack of fruitful interventions, which successfully improve both adherence and treatment outcome [7]. Therefore, the aim was to review the last five years of published educational interventions for improving adherence to asthma medication.
Systematic searches were carried out in the databases PubMed, Cinahl and Scopus with the following limitations: English language, publication between 2007 and 2011, adults (≥18 years) and articles accessible in full-text versions. Inclusion criteria were that the articles should be based on an empirical intervention including efforts to improve adherence in adult persons with asthma. Reviews, guidelines and study protocols were excluded. The following search terms were used: asthma, adherence, compliance, medication and intervention. In PubMed the Mesh terms: behavioral medicine, patient education and health psychology were used and in Cinahl the heading: medication compliance was used. The search terms were used in combinations and together with the Boolean operators OR and AND. Twenty articles matched the stipulated criteria and were included in the current review.
Thanks to the large body of adherence research conducted in recent decades, a rather good picture of factors that influence adherence behaviour is obtainable. The World Health Organization (WHO) has organized these factors into five dimensions: social/economic, therapy-related, patient-related, condition-related factors and those related to the health-care team and system [8]. As efforts to improve adherence are recommended to address these dimensions [9], the current review adheres to that recommendation and will present the articles accordingly.
Because asthma medication usually is administered by inhalation, the patients need to have an adequate technique to allow the medication to deposit in the lungs. Although manufacturing companies are striving to develop inhalers that are user friendly, incorrect inhaler use seems common [12, 13]. Another problem is that many patients seem to be unaware of their incorrect inhaler technique [12]. Considering adherence, this could be referred to as unintentional non-adherence, which means that the patient has an intention to adhere to recommended treatment, but fails due to defective inhaler technique [14, 15]. Five of the articles included in this review specifically addressed the issue with incorrect inhaler technique in their educational interventions.
In all five studies improvements in patients' inhaler technique were reported but Hardwell et al. [16] concluded that despite improvements the majority still used a faulty technique. The interventions were carried out by asthma nurses in two studies [16, 17], by pharmacists in two studies [18, 19] and by physicians in one study [20].
Repeated inhaler instructions were used as method to improve inhaler technique in three of the studies [16, 19, 20] and in the other two studies tailored and individualised educational strategies were used [17, 18]. Takemura et al. [20], invited 146 patients of which 25 received repeated instructions of inhaler use and their inhaler technique was checked regularly. The instructions comprised verbal information and demonstration provided by their physician. In the study conducted by Daiane de Oliveira and colleagues [19], patients assigned to the intervention (n=28) received instructions on correct use of medication on four occasions, while the control group (n=27) only received this information once. Hardwell et al. [16] enrolled patients (n=1,092) with uncontrolled asthma prescribed pressurised metered-dose inhaler (pMDI) to check their inhaler technique using an Aerosol Inhalation Monitor (AIM). Patients received specific education on pMDI use, if they failed any of the three set AIM parameters. Takemura et al. [20] reported that their intervention apart from improving inhaler skills also resulted in improvements in self-reported adherence. These findings were partly opposed to those reported by Daiane de Oliveira et al. [19], who reported that there was no difference between the groups as regards reported adherence, but the inhaler technique had improved in the intervention group by the end of the project. The intervention carried out by Hardwell et al. [16] resulted in a statistically significant increase in number of patients with appropriate pDMI use after two and three educational occasions, but a majority of the patients still used faulty inhaler technique.
In a randomised controlled trial, a tailor-made intervention, depending on the patient's current asthma control, was used to optimise use of asthma medication [18]. The intervention group (n=94) received education on three occasions at the pharmacy and the control group (n=107) received usual care. The effect of this intervention was estimated after six months and was described as higher frequency of filled prescriptions and better inhaler technique in the intervention group compared to the control group. The use of rescue medication was decreased and fewer nighttime awakenings were reported in the intervention group. However, self-reported adherence was similar in both groups [18]. This inconsistency in adherence estimations (frequencies of prescription fills and self-reports) sheds light on the difficulties with adherence monitoring.
An individualised education program was used in patients defined as "poor adherers to asthma medication" [17]. The intervention comprised three individual sessions each lasting 30 min. In the first session a nurse checked the patient's knowledge and skills about his/her prescribed inhaler. A trained nurse informed and demonstrated the skills for self-management of asthma including inhaler technique. In the second session, a pharmacist informed about dosage, effects and side-effects of the medication but also about the method of controlling dosage based on asthma symptoms and lung function measured with peak expiratory flow (PEF). During the third session, patients were provided a self-asthma action plan describing how to recognise and to handle an asthma attack. The plan also gave clear instructions about how to use the asthma medication, how to interpret PEF rates and to avoid triggers. This intervention specifically improved both inhaler skills and increased PEF values, suggesting that asthma control became better. These effects sustained eight weeks after the intervention and this was the last follow-up [17].
Patients' perceptions of their asthma and their beliefs about asthma medication may influence adherence behaviour [9]. These perceptions and beliefs could result in so called intentional non-adherence, which is a result of a person's conscious decision to deviate from the recommended treatment, for instance by under or overusing the medication or by prematurely terminating the treatment [14, 15]. Patients, who deny an asthma diagnosis, or patients, who do not perceive their asthma to be a chronic condition, seem more inclined to refrain from the medication treatment [21]. Medication beliefs are also known to influence adherence behavior. For instance, patients who regard the asthma medication as a necessity for their health, seem more motivated to follow the treatment recommendations [21-23], whereas those who are concerned with side-effects or becoming dependent, tend to intentionally deviate from the recommendations [21, 23]. Patients who have concerns about regular medication intake, side-effects or poor effect, also tend to display a non-adherent behaviour [24]. In this review, one article specifically addressing illness perceptions and four studies addressing medication beliefs as a means to improve adherence, were included.
Illness perceptions as factors influencing adherence were addressed by Smith et al. [25] who intervened by using a self-management model of illness comprising a structured step-wise and patient-centered approach. The intervention lasted nine months and patients were randomised to intervention (n=35) or control group (n=56), which received usual care. The health-care providers used the model to help the patients to identify areas of everyday life when asthma control was difficult to achieve, to set goals and to find strategies how to deal with these problematic situations. Hereby, the patients were working with personal defined goals and strategies. This intervention did not result in improved adherence to asthma medication. Instead asthma control, asthma self-efficacy and asthma quality of life improved in both groups but more in the intervention group.
All four studies addressing medication beliefs reported that their approaches had a positive impact on medication barriers and adherence behaviour. In three studies, telephone calls were used as method to carry out the interventions whereas Clerisme-Beaty and colleagues [26] used quite a different method to address adherence and medication beliefs by using a specific drug presentation style. The presentation about the drug was aimed at increasing patients' expectancy that the asthma medication could control the asthma symptoms adequately. Patients (n=25) who received the medication presented in this manner reported better adherence and they also expressed higher expectancy with the specific asthma medication.
In a randomised controlled trial [27], the effect of phone calls made by pharmacists to patients, who received their first prescription for a long-term disease (ten had asthma), was evaluated. Two weeks after the patients had filled their prescription, a pharmacist phoned the patient to ask if there were any problems with the medication, about adherence and whether any additional information was needed. The pharmacist gave information and advice depending on the patient's expressed needs. Four weeks later a researcher phoned the patients asking about the medication and adherence. The intervention of the pharmacist calling the patients resulted in better self-reported adherence in comparison to the control group. According to the result section in the abstract, fewer problems with the medication were reported in the intervention group [27].
Telephone calls were combined with educational material sent by mail on three occasions, in an intervention conducted by Park et al. [28]. The study group (n=87) received two telephone calls from a trained care manager with a health-care background. The phone-calls were concentrated on barriers to asthma medication adherence and the development of asthma management strategies. The educational mailings comprised general medication adherence topics and asthma specific information. Each telephone call and mailing did also encourage the participant to carry out proper asthma management. The intervention lasted six months and resulted in a reduction in both adherence barriers and in days when housework and schoolwork were limited due to asthma. Additionally, a reduction in the number of days when the patients was unable to attend to social, recreational and family activities was seen.
The effect of an "interactive voice recognition call" on adherence to asthma medication treatment was evaluated by Bender et al. [29]. The intervention group (n=25) received a maximum of three robot-phone calls during the intervention period of ten weeks and the control group (n=25) received none. By the end of this project, the intervention group reported both increased adherence and a favourable change in medication beliefs.
The symptom variability characteristic for asthma is claimed to be an important barrier to remain in regular medication treatment. This typical asthma feature could thus lead to doubts about the diagnosis and the need for regular medication treatment [9], which may explain why initiated medication treatment sometimes is interrupted when the asthma symptoms vanish [22] or when the patients start to feel better [30]. On the other hand, an adherent behaviour seems more likely to occur among those who perceive their asthma as severe [22] but it has also been reported that poor adherence frequently occurs among asthmatics with uncontrolled disease [31, 32]. Two articles were included in this section of the review, of which one succeeded in improving adherence.
Patients with "difficult asthma" were invited to a two phase intervention [33]. The first phase comprised a "concordance discussion", which addressed whether the patient was adherent or not. Briefly, poor adherence was determined using prescription refill frequency, and a plan to address adherence obstacles was actively discussed with the appropriate patients. At six months follow-up, an improvement in adherence among the patients (n=83) was seen, which was associated with improved lung function and a reduction of hospital admissions. The second phase comprised an individual psycho-educational intervention, which was planned in light of the patient's stated reasons for not adhering to the prescribed asthma medication treatment. Nine patients were randomised to the intervention and 11 to the control group. The effect of the intervention was determined at 12 months and was seen in an increase in prescriptions filled, as well as a reduction in total oral corticosteroid doses taken [33].
Patients with moderate and severe asthma (n=333) participated in a randomised controlled trial testing whether an individualised problem-solving intervention improved adherence to inhaled corticosteroids and asthma outcomes [34]. The intervention group (n=165) took part in four 30 min sessions aimed at improving or maintaining adherence by addressing individual barriers to adherence and finding solutions to remove the barriers. The control group (n=168) received standard asthma education during four 30 min sessions covering asthma topics exclusive of adherence. Adherence, which was measured electronically, decreased in both groups. In contrast, both asthma control and asthma quality of life improved, but emergency department visits and hospitalisation were unaffected [34].
Patients' dissatisfaction with the patient-provider interaction may have a negative impact on adherence behaviour. Another factor related to the health-care system could be that the appointments with the physicians are too short to include patient education and to provide written information about asthma [9]. Patients and physicians seem to have different perceptions about the content during appointments. For instance, patients think that inhaler technique and side-effects with the asthma medication is discussed more rarely than do the physicians [35]. Two of the articles included in this review addressed the interaction between the patient and the health-care provider and six studies focused on patient education.
Both studies included in this section of the review focused on stimulating to a collaborative effort between the patient and the health-care provider to improve adherence to asthma medication. The effect of "shared decision making" between the patient and clinician as regards asthma medication was investigated in a randomised controlled trial. The intervention group (n=182) shared in making decisions about the medication, in the other group the clinician made the decisions (n=180) and the third group received usual care (n=189). At follow-up after one year, the patients, who shared in making decisions about their asthma medication treatment, improved their adherence based on pharmacy data, but at follow-up after two years the intervention effect did not occur. Nevertheless, adherence was better at year two compared to baseline scores [36].
A "cueing therapeutic communication" between patients and their clinicians was used to improve adherence to inhaled corticosteroids and asthma control in another study. The cue intervention comprised of visually standardised interpreted peak flow graphs, which were aimed to enhance the communication about the patient's treatment plan. Sixty-eight patients assigned to 22 clinicians were randomised to the intervention group and 71 patients assigned to 21 clinicians to the control group. At the first visit the patients received a brief education session and a booklet. Adherence was measured electronically but in some cases the inhalers' own dose counters were used. This intervention did not improve adherence but it seemed that it had a positive influence on asthma control, as patients who participated in the intervention used fewer courses of oral steroids during winter and spring, reported fewer asthma worsenings and made fewer urgent care visits during winter in comparison to the control group. However, there was no difference in the patients' perceptions of the communication between the clinicians between the two groups [37].
This section of the review comprises articles describing rather extensive educational interventions covering important aspects of asthma management required for an adequate self-management.
The two studies in which interventions had a clear effect on adherence, were conducted by Morisky et al. [38] and by Armour et al. [39]. The first study was a two year prospective evaluation of a cohort comprising of 15,275 patients, of which 35% had asthma. The aim was to determine the effect of a disease management program addressing physiological and behavioural health indicators by tailored education. The results in the asthma subgroup showed significant increase in adherence in relation to asthma medication and improved asthma symptoms in regard to severity, frequency, nocturnal awakenings and activity limitations. Additionally, the patient's use of PEF monitoring to assess asthma was increased [38]. The second study tested the effect of a pharmacy asthma care program comprising targeted education on the asthma, medication, lifestyle, inhaler technique, adherence, medication problems and goal-setting. Fifty pharmacies were randomised to the intervention and control pharmacies and 165 patients completed the intervention and 186 control patients finalised the study. The intervention resulted in improved adherence to preventer medication and a simultaneous reduction in reliever medication use in the intervention group. Moreover, the risk of non-adherence decreased and asthma quality of life, asthma knowledge and asthma control improved [39].
Three additional studies using educational programs reported important progress in self-management but the effect was not clearly reflected in adherence behaviour.
The effect of asthma education in two intervention groups, which received specific asthma education comprising elements of asthma management, inhaler use techniques as well as written information, was investigated by Kritikos et al. [40]. In one intervention group, the education was provided by specially trained pharmacists and the other group by pharmacist researchers trained as asthma educators. The control group did only receive written information - the same as in the intervention groups. Adherence measured through self-reports improved in both intervention groups but not more than in the control group.
In the next study, Wang et al. [41] explored whether there were any differences in outcomes if the patients were provided with asthma education by a nurse, or asthma counseling by a pharmacist. The patients were randomly assigned to two intervention groups and one control group. The first intervention group (n=35) received education from a nurse including asthma knowledge, monitoring disease severity, PEF use, information about asthma medication and self-management such as triggers and handling asthma attacks. The second group (n=34) received the same education in combination with information about the function and side-effects of the asthma medication by a pharmacist. The control group received usual care. At the last follow-up after six months, the two intervention groups had no significantly higher adherence compared to the control group.
The impact of self-management education on adherence to asthma medication was studied by Janson et al. [42]. Eighty-four participants were randomised to an individualised self-management education (n=45) or to a control group (n=39) receiving usual care. The intervention lasted 30 minutes and was given on three occasions with two weeks interval. The first was held by a nurse and a respiratory therapist both certified as asthma educators. There was also a personalised part addressing results from spirometry, PEF, skin prick tests and specific strategies to remove triggers. Adherence was monitored electronically. Mean adherence did not differ between the intervention and the control groups. When adherence scores were dichotomised as ≥60% or <60%, the odds of maintaining ≥60% adherence was nine-fold for the intervention group. These odds were maintained at 24 weeks, when the intervention was finalised.
These last three studies considered, a positive effect on patient's asthma knowledge was seen [40-42]. In Wang's study [41] no improvements in asthma quality of life were seen but in Kritikos' study [40] an improvement in both asthma quality of life and inhaler technique was found in the intervention groups. Kritikos et al. [40] also found a reduction in severe asthma and in Janson's study [42], the intervention group reported fewer symptoms than the controls but mean symptom scores decreased in both groups. The nocturnal awakenings decreased in the intervention group and the odds of experiencing awakenings decreased in this group. The use of rescue medication decreased in the intervention group versus in the control group but both groups decreased their use during the intervention.
The final study had a different approach in comparison with the other studies in this section as a learner centered intervention was used. The focus was on interactive discussions, problem-solving, social support and procedures to change asthma specific behaviour. Additionally, the participants were encouraged to support each other. Twenty-four patients were randomised to the intervention group and 21 in the control group. The intervention comprised seven weekly meetings lasting two hours. The effect of this self-management program was reflected in improved asthma knowledge and asthma quality of life, self-efficacy and patient activation. As regards use of controller medication the mean was already at intervention start 6.8 of a maximum 7 scores, which did not leave much space for an improvement [43].
With reference to the interventions accounted for in the present review, a reasonable conclusion is that stimulating the asthma patients to active participation in treatment planning seems to improve their self-management of asthma including adherence to prescribed asthma medication. As an example, increased adherence was seen among patients who shared in decisions about medication treatment [36] and among patients, whose medication problems and own treatment goals, were considered [39]. However, solving the dilemma with poor adherence is not that as easy as just engaging the patients, which was learnt from the study conducted by Smith et al. [25]. Regardless of ambitious efforts, not all interventions accounted for in the current review led to improved adherence. In some cases, because the control patients also improved their adherence behaviour, which brings to mind the famous Hawthorne effect [44].
Another conclusion is that medication barriers, which prevent adequate adherence to asthma medication, may be demolished by simple phone calls from a health-care professional [27-29]. If we could spare a couple of minutes to make a phone call to follow-up on our asthma patients' potential medication concerns, we may have a cost-effective method to promote adherence, which in continuation prevents poor asthma control. Another effective method may be to address unintentional non-adherence like poor inhaler skills with repeated instructions [16, 19, 20]. It is to be noted, as Hardwell et al. [16] put forward, that many patients have an incorrect technique despite having received education, which recommends that such instructions should be tailored to each patient's ability and that inhaler technique should be checked at each health-care appointment.
Another important remark is that dif ferent health-care professions have an educational role in promoting adherence to medication as part of proper asthma self-management. Addressing adherence in various health-care relations and contexts may emphasise its importance as the connecting link between the prescribed asthma medication and advantageous asthma outcomes. This work may be facilitated by identification of persons with high probability to display poorer adherence behaviour to asthma medication. The tricky part is to estimate accurate adherence level and to identify which patients are likely to deviate from a prescribed treatment, in daily practice in clinical settings [45]. The influence of patients' personality on health behaviours such as adherence to medication treatment could be one guiding tool in this aspect.
Personality could be described in terms of five broad and bipolar personality traits Neuroticism, Extraversion, Openness to experience, Agreeableness and Conscientiousness. Each of the five personality traits are hierarchical constructed by more specific personality traits. These five personality traits contribute to enduring and individual differences in disposition to display a certain behaviour in a given situation [46]. We have previously reported that persons with various chronic diseases, who scored higher on Neuroticism, lower on Agreeableness or lower on Conscientiousness, seemed more inclined to display poorer adherence to medication treatment [47]. In yet another study, we found that more impulsive young adults with asthma reported lower adherence to asthma medication than the less impulsive. Young adult men, who were either more antagonistic or alexithymic, also reported lower adherence to asthma medication [48]. Associations between Neuroticism and poorer adherence in men with asthma have also been reported [49]. The advantage of assessing personality in relation to adherence is that it provides an indication of potential personal needs [50], which could be useful targets when planning adherence support. For instance, less conscientiousness or impulsive persons, who tend to be less goal-directed and structured [46], may be less inclined to plan ahead. This behavior may not be conducive to regular medication intake. For that reason, they may benefit from support with reminders or incorporation of routines for their medication intake. In contrast, persons scoring high on Neuroticism, who could be described as worried and with difficulties handling stress [50], most likely need another type of adherence support.
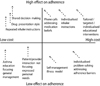
Some of the interventions in the currently reviewed articles were described as individualised for instance in terms of using the patients level of asthma knowledge, inhaler or PEF skills as points of departures [17] or interpretation of spirometry, PEF rate or control over environmental exposures [42], which certainly is of significance. Nevertheless, none of the interventions focused on individual differences in terms of personality among the selected patients, as personality is a major contributor of behavior, including health behavior [47, 48]. Fig. 1 shows a hypothetical personality perspective on adherence interventions. As a suggestion, future interventions aimed at promoting adherence and preventing poor asthma control should focus on persons with high risk of displaying poor adherence to the prescribed asthma medication treatment. In this work, assessment of personality could provide a useful tool to identify patients' different needs and resources [50], which could function as targets when planning forthcoming adherence support.
Figures and Tables
References
1. Latry P, Pinet M, Labat A, Magand JP, Peter C, Robinson P, Martin-Latry K, Molimard M. Adherence to anti-inflammatory treatment for asthma in clinical practice in France. Clin Ther. 2008. 30:1058–1068.

2. Gamble J, Stevenson M, McClean E, Heaney LG. The prevalence of nonadherence in difficult asthma. Am J Respir Crit Care Med. 2009. 180:817–822.

3. Jones C, Santanello NC, Boccuzzi SJ, Wogen J, Strub P, Nelsen LM. Adherence to prescribed treatment for asthma: evidence from pharmacy benefits data. J Asthma. 2003. 40:93–101.

4. Williams LK, Pladevall M, Xi H, Peterson EL, Joseph C, Lafata JE, Ownby DR, Johnson CC. Relationship between adherence to inhaled corticosteroids and poor outcomes among adults with asthma. J Allergy Clin Immunol. 2004. 114:1288–1293.

5. Bender BG, Pedan A, Varasteh LT. Adherence and persistence with fluticasone propionate/salmeterol combination therapy. J Allergy Clin Immunol. 2006. 118:899–904.

6. Global Strategy for Asthma Management and Prevention, Global Initiative for Asthma (GINA). Accessed: 2011-11-18. [updated December 2010]. Available from: http://www.ginasthma.org.
7. Haynes RB, Ackloo E, Sahota N, McDonald HP, Yao X. Interventions for enhancing medication adherence. Cochrane Database Syst Rev. 2008. CD000011.

8. World Health Organization. Adherence to long-term therapies: evidence for action. 2003. Geneva: World Health Organization.
9. O'Donohue WT, Levensky ER. Promoting treatment adherence: a practical handbook for health care providers. 2006. Thousand Oaks: Sage Publications.
10. Williams SL, DiMatteo MR, Haskard KB. Shumaker SA, Ockene JK, Riekert KA, editors. Psychosocial barriers to adherence and lifestyle change. The handbook of health behavior change. 2009. New York: Springer Publishing Company;445–462.
11. DiMatteo MR. Variations in patients' adherence to medical recommendations: a quantitative review of 50 years of research. Med Care. 2004. 42:200–209.
12. Souza ML, Meneghini AC, Ferraz E, Vianna EO, Borges MC. Knowledge of and technique for using inhalation devices among asthma patients and COPD patients. J Bras Pneumol. 2009. 35:824–831.
13. Lavorini F, Magnan A, Dubus JC, Voshaar T, Corbetta L, Broeders M, Dekhuijzen R, Sanchis J, Viejo JL, Barnes P, Corrigan C, Levy M, Crompton GK. Effect of incorrect use of dry powder inhalers on management of patients with asthma and COPD. Respir Med. 2008. 102:593–604.

14. Horne R. Compliance, adherence, and concordance: implications for asthma treatment. Chest. 2006. 130:65S–72S.
16. Hardwell A, Barber V, Hargadon T, McKnight E, Holmes J, Levy ML. Technique training does not improve the ability of most patients to use pressurised metered-dose inhalers (pMDIs). Prim Care Respir J. 2011. 20:92–96.

17. Choi JY, Cho Chung HI. Effect of an individualised education programme on asthma control, inhaler use skill, asthma knowledge and health-related quality of life among poorly compliant Korean adult patients with asthma. J Clin Nurs. 2011. 20:119–126.

18. Mehuys E, Van Bortel L, De Bolle L, Van Tongelen I, Annemans L, Remon JP, Brusselle G. Effectiveness of pharmacist intervention for asthma control improvement. Eur Respir J. 2008. 31:790–799.

19. Daiane de Oliveira S, Martins MC, Cipriano SL, Pinto RM, Cukier A, Stelmach R. Pharmaceutical care for patients with persistent asthma: assessment of treatment compliance and use of inhaled medications. J Bras Pneumol. 2010. 36:14–22.
20. Takemura M, Kobayashi M, Kimura K, Mitsui K, Masui H, Koyama M, Itotani R, Ishitoko M, Suzuki S, Aihara K, Matsumoto M, Oguma T, Ueda T, Kagioka H, Fukui M. Repeated instruction on inhalation technique improves adherence to the therapeutic regimen in asthma. J Asthma. 2010. 47:202–208.

21. Horne R, Weinman J. Self-regulation and self-management in asthma: exploring the role of illness perceptions and treatment beliefs in explaining non-adherence to preventer medication. Psychol Health. 2002. 17:17–32.

22. Ulrik CS, Backer V, Søes-Petersen U, Lange P, Harving H, Plaschke PP. The patient's perspective: adherence or non-adherence to asthma controller therapy? J Asthma. 2006. 43:701–704.

23. Menckeberg TT, Bouvy ML, Bracke M, Kaptein AA, Leufkens HG, Raaijmakers JA, Horne R. Beliefs about medicines predict refill adherence to inhaled corticosteroids. J Psychosom Res. 2008. 64:47–54.

24. Choi TN, Westermann H, Sayles W, Mancuso CA, Charlson ME. Beliefs about asthma medications: patients perceive both benefits and drawbacks. J Asthma. 2008. 45:409–414.

25. Smith L, Bosnic-Anticevich SZ, Mitchell B, Saini B, Krass I, Armour C. Treating asthma with a self-management model of illness behaviour in an Australian community pharmacy setting. Soc Sci Med. 2007. 64:1501–1511.

26. Clerisme-Beaty EM, Bartlett SJ, Teague WG, Lima J, Irvin CG, Cohen R, Castro M, Wise RA, Rand CS. The Madison Avenue effect: how drug presentation style influences adherence and outcome in patients with asthma. J Allergy Clin Immunol. 2011. 127:406–411.

27. Elliott RA, Barber N, Clifford S, Horne R, Hartley E. The cost effectiveness of a telephone-based pharmacy advisory service to improve adherence to newly prescribed medicines. Pharm World Sci. 2008. 30:17–23.

28. Park J, Jackson J, Skinner E, Ranghell K, Saiers J, Cherney B. Impact of an adherence intervention program on medication adherence barriers, asthma control, and productivity/daily activities in patients with asthma. J Asthma. 2010. 47:1072–1077.

29. Bender BG, Apter A, Bogen DK, Dickinson P, Fisher L, Wamboldt FS, Westfall JM. Test of an interactive voice response intervention to improve adherence to controller medications in adults with asthma. J Am Board Fam Med. 2010. 23:159–165.

30. Laforest L, El Hasnaoui A, Pribil C, Ritleng C, Osman LM, Schwalm MS, Le Jeunne P, Van Ganse E. Asthma patients' self-reported behaviours toward inhaled corticosteroids. Respir Med. 2009. 103:1366–1375.

31. Bender BG, Long A, Parasuraman B, Tran ZV. Factors influencing patient decisions about the use of asthma controller medication. Ann Allergy Asthma Immunol. 2007. 98:322–328.

32. Adams RJ, Appleton S, Wilson DH, Ruffin RE. Participatory decision making, asthma action plans, and use of asthma medication: a population survey. J Asthma. 2005. 42:673–678.

33. Gamble J, Stevenson M, Heaney LG. A study of a multi-level intervention to improve non-adherence in difficult to control asthma. Respir Med. 2011. 105:1308–1315.

34. Apter AJ, Wang X, Bogen DK, Rand CS, McElligott S, Polsky D, Gonzalez R, Priolo C, Adam B, Geer S, Ten Have T. Problem solving to improve adherence and asthma outcomes in urban adults with moderate or severe asthma: a randomized controlled trial. J Allergy Clin Immunol. 2011. 128:516–523.e1-5.
35. Canonica GW, Baena-Cagnani CE, Blaiss MS, Dahl R, Kaliner MA, Valovirta EJ. Unmet needs in asthma: Global Asthma Physician and Patient (GAPP) Survey: global adult findings. Allergy. 2007. 62:668–674.

36. Wilson SR, Strub P, Buist AS, Knowles SB, Lavori PW, Lapidus J, Vollmer WM. Shared treatment decision making improves adherence and outcomes in poorly controlled asthma. Am J Respir Crit Care Med. 2010. 181:566–577.

37. Janson SL, McGrath KW, Covington JK, Baron RB, Lazarus SC. Objective airway monitoring improves asthma control in the cold and flu season: a cluster randomized trial. Chest. 2010. 138:1148–1155.
38. Morisky DE, Kominski GF, Afifi AA, Kotlerman JB. The effects of a disease management program on self-reported health behaviors and health outcomes: evidence from the "Florida: a healthy state (FAHS)" Medicaid program. Health Educ Behav. 2009. 36:505–517.

39. Armour C, Bosnic-Anticevich S, Brillant M, Burton D, Emmerton L, Krass I, Saini B, Smith L, Stewart K. Pharmacy Asthma Care Program (PACP) improves outcomes for patients in the community. Thorax. 2007. 62:496–502.

40. Kritikos V, Armour CL, Bosnic-Anticevich SZ. Interactive small-group asthma education in the community pharmacy setting: a pilot study. J Asthma. 2007. 44:57–64.

41. Wang KY, Chian CF, Lai HR, Tarn YH, Wu CP. Clinical pharmacist counseling improves outcomes for Taiwanese asthma patients. Pharm World Sci. 2010. 32:721–729.

42. Janson SL, McGrath KW, Covington JK, Cheng SC, Boushey HA. Individualized asthma self-management improves medication adherence and markers of asthma control. J Allergy Clin Immunol. 2009. 123:840–846.

43. Tousman SA, Zeitz H, Bond D, Stewart D, Rackow R, Greer R, Hatfield S, Layman K, Ganjwala P. A randomized controlled behavioral trial of a new adult asthma self-management program. J Asthma Allergy Educ. 2011. 2:91–96.

44. Gillespie R. Manufacturing knowledge: a history of the Hawthorne experiments. 1991. Cambridge: Cambridge University Press.
45. Otsuki M, Clerisme-Beaty E, Rand CS, Riekert KA. Shumaker SA, Ockene JK, Riekert KA, editors. Measuring adherence to medication regimens in clinical care and research. The handbook of health behavior change. 2009. New York: Springer Publishing Company;309–325.
46. McCrae RR, Costa PT Jr. Personality in adulthood: a five-factor theory perspective. 2003. 2nd ed. New York: Guilford Press.
47. Axelsson M, Brink E, Lundgren J, Lötvall J. The influence of personality traits on reported adherence to medication in individuals with chronic disease: an epidemiological study in West Sweden. PloS One. 2011. 6:e18241.

48. Axelsson M, Emilsson M, Brink E, Lundgren J, Torén K, Lötvall J. Personality, adherence, asthma control and health-related quality of life in young adult asthmatics. Respir Med. 2009. 103:1033–1040.

49. Emilsson M, Berndtsson I, Lötvall J, Millqvist E, Lundgren J, Johansson A, Brink E. The influence of personality traits and beliefs about medicines on adherence to asthma treatment. Prim Care Respir J. 2011. 20:141–147.

50. Costa PT, McCrae RR. Revised NEO Personality Inventory (NEO-PI-R) and NEO Five-Factor Inventory (NEO-FFI) professional manual. 1992. Odessa: Psychological Assessment Resources.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download