Abstract
Background
Dental fear is usually associated with hemodynamic changes. Fear of pain during the surgical removal of a lower impacted third molar might cause patients anxiety, thereby leading to avoidance of any future dental therapy. This study aimed to determine the effect of experiencing a surgical impacted-tooth removal on the pain perception-related anxiety and hemodynamic status.
Methods
Twenty-seven healthy patients aged 15–30 years (mean age, 24 years), for whom surgical removal of bilateral lower third molars was advised, were included. This prospective, randomized, controlled, split-mouth study involved operations on both sides of the mandibular arch, with a 1-month washout period in between. Blood pressure and heart rate were measured before the surgical procedure, during and after the injection, preoperatively, and postoperatively. Pain perception was evaluated using a 100-mm visual analog scale during the injection, preoperatively, and postoperatively after the numbness disappeared. Differences in the blood pressure, heart rate, and pain perception between the two appointments were analyzed using the paired t-test. For all statistical analyses, SPSS version 11.5 was used.
Results
The mean pain perception values during the injection and preoperatively showed no significant differences between the two appointments (P > 0.05); however, significant differences in the blood pressure and heart rate were noted before the surgical procedure; preoperatively, the blood pressure alone showed a significant difference (P < 0.05).
Dental fear is commonly found in the population, especially in those with previous unpleasant dental experiences. Dental fear is usually associated with the pain caused during the procedure; thereafter, patients avoid future dental treatments, which can lead to more dental problems, thus complicating the diagnosis, treatment planning, and overall well-being [1].
The common procedure that causes fear of dental treatment is the local anesthetic injection [23]. Although the main purpose of the local anesthetic injection is to relieve the pain during the dental treatment procedure, the injection itself causes pain; hence, the majority of patients fear local anesthetic injection. Further, dental fear is associated with hemodynamic changes in humans [4], and the reality of the surgery (especially removal of the lower impacted third molar) causes severe pain. Visual analog scale (VAS) has been used to measure the pain and dental anxiety associated with the surgical procedure or dental treatment [567]. Dental fear associated with a surgical procedure causes anxiety in most patients.
Locker et al. [8] found that the relationship between a terrible dental experience and future dental treatment was related to anxiety. This study had included 6,360 patients aged over 18 years; random questionnaires dealing with the dental experience, feeling toward the dentist, anxiety during the dental therapy, and overall attitude toward the dental appointment were used. In the study by Edmund et al. [9], 74 subjects aged 17–65 years were divided into 3 groups based on the level of dental fear and anxiety. Kleinknecht et al. [10] also studied the level of fear in patients to test the concept of anxiety, and assessed the level of concern in dental patients. In 1985, Steven et al. evaluated the anxiety and level of fear in patients, and found that there was a relationship between these two factors [11]. Moreover, in 2004, a questionnaire-based study by Klages et al. [12] on patients receiving dental treatment claimed that there was a relationship between anxiety and pain associated with dental treatment.
In 2011, a remarkable study [1314] showed that music reduced patients' anxiety, and their vital signs changed significantly throughout the surgery according to the stage of the procedure. The changes in blood pressure and heart rate could be used to determine the anxiety of the patients receiving treatment. Kim et al. [13] made the patients in the study group listen to their favorite music, while those in the control group were not made to listen to any music during the surgery. The evaluation of anxiety was done by assessing the changes in the vital signs. The results showed that there were alterations in the hemodynamic parameters of the patients (blood pressure and heart rate) measured during the surgery. Thus, Kim et al. [13] concluded that patients who listened to music had significantly less intraoperative anxiety than the control group, after controlling all the preoperative anxiety levels. In 2011, Mobilio et al. studied the pain experienced by patients after a lower third molar extraction and compared it with the preoperative pain; they measured the pain threshold level using the VAS [15]. Previous studies have shown that anxiety is related to pain due to surgical removal of an impacted lower third molar [161718]. Removal of lower impacted third molars cause severe pain compared to other dental treatments, and this can cause anxiety in most patients. The purpose of this study was to evaluate the change in pain perception after a previous surgical experience by measuring the hemodynamic changes; surgical removal of impacted lower third molars was performed in this study.
The study protocol was approved by the research ethics committee of the Mahidol University Institutional Review Board (MU-IRB; COA No. MU-DT/PY-IRB 2012/049.0310). Written informed consent was obtained from all patients prior to the study.
This prospective, randomized, controlled, split-mouth study included 27 patients aged 15–30 years (mean age, 24 years), who underwent bilateral lower third molar surgery.
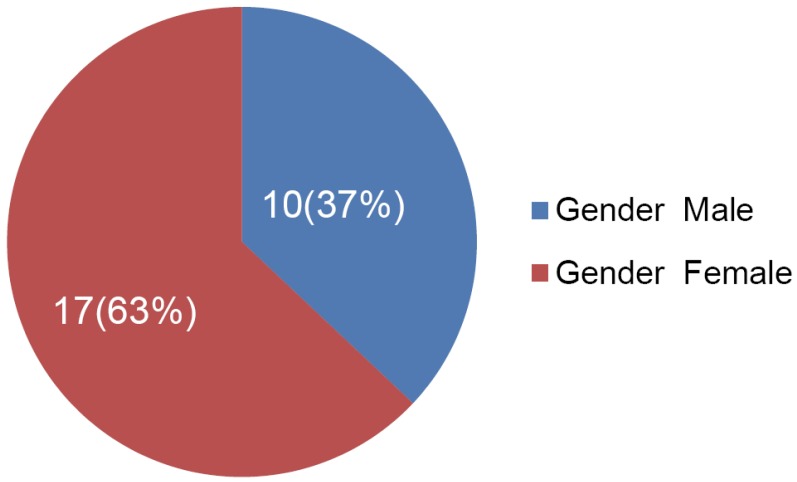
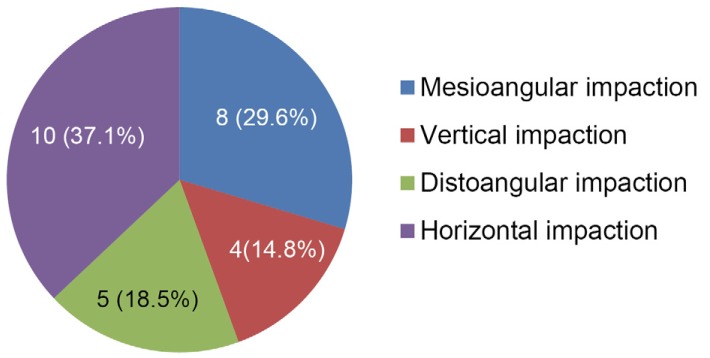
Table 1 shows the inclusion and exclusion criteria that were used for selecting the patients. A total of 10 male and 17 female patients were enrolled, as shown in Fig. 1; these subjects underwent different lower third molar surgeries (Fig. 2, 3). The surgery was performed twice using the randomized split-mouth design. The first appointment constituted the control group, which consisted of patients with no previous experience of surgical tooth removal. The study group was constituted by the same patients, who were operated on again after a 1-month washout period.
At the beginning of each procedure, the hemodynamic parameters, such as the heart rate and blood pressure, were recorded. Subsequently, the surgeon administered the injection for blocking the inferior alveolar nerve on the side of the planned surgery. An assistant measured the hemodynamic conditions again, during and after the injection. Furthermore, measurement of the heart rate and blood pressure were performed at the start of the surgery and at the end of the standard surgical removal of the lower impacted third molar. After completing the surgical procedure, the patient was rested in the same position for a while, and subsequently, the heart rate and blood pressure were measured again. Thereafter, the patients were requested to complete the pain assessment form (VAS) [517] for grading the pain during the injection, surgery, and after the disappearance of numbness postoperatively. On the opposite side, 1 month after the first surgical procedure, the heart rate and blood pressure measurement, pain assessment, and surgical removal were performed in a similar manner as for the control group by the same surgeon and assistant. All postoperative complications were managed appropriately and recorded.
The data were analyzed using the Student's t-test (P < 0.05) with a statistical software (SPSS version 11.5), and interpreted in keeping with the objectives of this study.
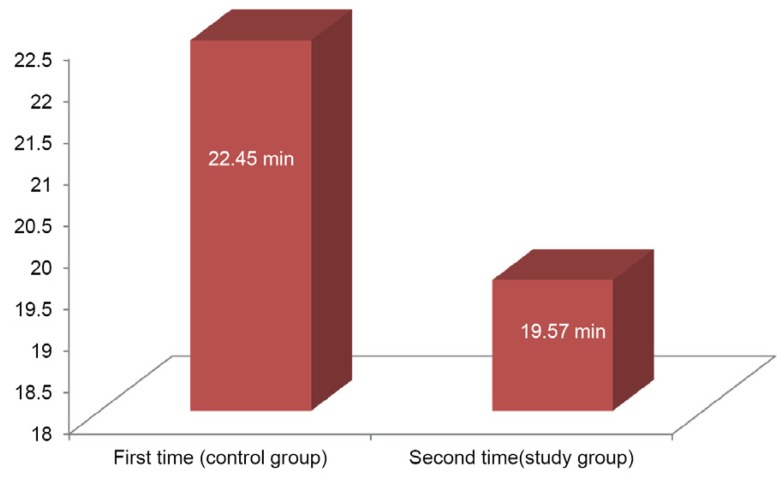
The operating times for the first and second surgical removal of the lower third molars are shown in Fig. 4. The difference was not statistically significant (P > 0.05).
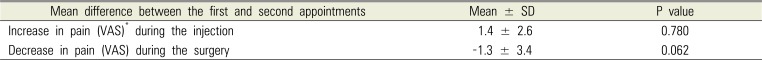
This study also revealed that there was decreased pain during the injection and increased pain during the surgery; however, these findings were not statistically significant (P > 0.05) (Table 2). The interpretation and derivation of pain information from the VAS was based on the study by Jensen [5], which was published in 2003 by the American Pain Society; a score of 0–4 mm was regarded as no pain, 5–44 mm as mild pain, 45–74 mm as moderate pain, and 75–100 mm as severe pain.
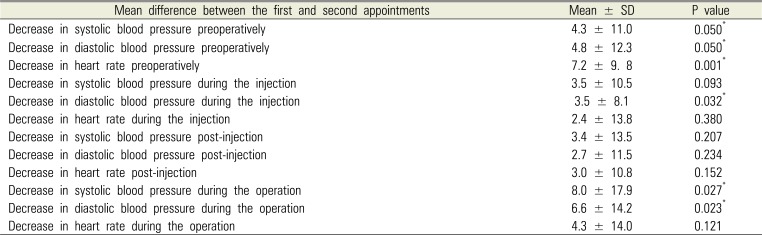
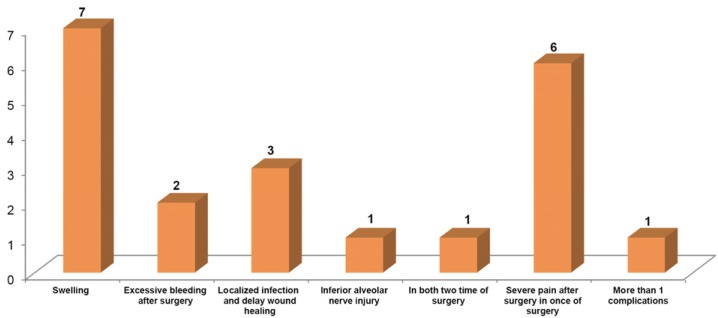
Table 3 shows a significant decrease in the systolic and diastolic blood pressure, and heart rate before the surgery, diastolic blood pressure during the injection, and systolic and diastolic blood pressure during the surgery (P < 0.05). These results were obtained from the analysis of each parameter during the first (control group) and the second (study group) operations. Moreover, Fig. 5 shows the postoperative complications that occurred during this study.
There are previous studies [161718] that report that anxiety and severe pain from dental procedures are related to the hemodynamic changes. Dental procedures can cause fear in patients, which could further complicate oral health care problems. Dental fear is related to hemodynamic changes [161718], and together with the dental pain, hemodynamic changes also cause anxiety in patients.
The reality of surgery, especially removal of lower impacted third molars, causes severe pain. We used the VAS to measure the pain associated with surgery [19], based on the study by Jensen et al. [5], which regarded a score of 0–4 mm as no pain, 5–44 mm as mild pain, 45–74 mm as moderate pain, and 75–100 mm as severe pain.
During the first surgery, the patients did not have any prior experience of surgery and the pain and anxiety experienced might have been due to the increased hemodynamic changes. However, during the second surgery, the patients had a prior experience and hence, the hemodynamic changes did not differ significantly from the preoperative values. Therefore, anxiety had only a slight effect on the hemodynamic changes during the removal of lower impacted third molars.
This study also showed that the difficulty of impacted tooth removal was not different between the study and control groups, as the operating times did not show any statistically significant difference, as seen in Fig. 4.
This study also identified an increase in the pain perception during the second surgery, compared to the first surgery; however, these results were not statistically significant (P > 0.05). Pain perception is subjective; hence, the results might have been affected by the emotions of the patients, environment, and individual experiences. Postoperative complications might also have affected the perception of pain. Some of these factors could not be controlled; however, they were minimized as much as possible, so that the results of pain perception would be least affected.
Measurement of the patient's anxiety in this study was performed using alterations of hemodynamic parameters, such as blood pressure and heart rate [2021222324]; however, the results showed no statistically significant difference in both the groups. Hence, decreased blood pressure and heart rate might not be accurate parameters for determining the anxiety of patients in a clinical setting. The instrument used to measure the vital signs might not have been sensitive enough to differentiate minute changes, which might have affected the statistical analyses. Furthermore, variations in recording the time and human errors during the recording of the vital signs might have affected the results.
The study by Alemany-Martínez et al. in 2008 [15] and other previous studies [1725] claimed that there were statistically insignificant alterations of the vital signs during surgical impacted-tooth removal. This study showed a significantly decreased heart rate, systolic blood pressure, and diastolic blood pressure, especially preoperatively (P < 0.05); however, the data showed a different trend for the other periods. Consistency of the data might be affected by uncontrollable factors, such as the characteristics of the impacted teeth, surgeon skills, and data recording factors. It is impossible to control all these factors in clinical practice; however, the errors can be minimized so that the influence of these factors on the blood pressure and heart rate remains negligible.
In this study, the local anesthetic agents administered contained epinephrine as a vasoconstrictor, which would have maintained the blood pressure and heart rate changes during the operation. According to the studies by Vasconcellos et al. [26] and Carrera et al. [27], anesthetic and vasoconstrictor agents do not significantly affect the alteration of heart rate and blood pressure. This corresponds to the study by Frabetti et al. [20]. Hence, the vital sign measurements could be used since the influence of the vasoconstrictor was minimal.
In 2001, Fernieini et al. [28] reported significant alteration of the hemodynamic parameters measured during a surgical operation using a laser Doppler flowmeter, especially before the local anesthetic injection; this corresponds to our study, in which there was a significant alteration of blood pressure and heart rate before the surgery. We suggest the measurement of alterations in the vital signs using a more sensitive tool than a digital barometer, such as laser Doppler flowmeter, for more accurate results.
This study also found that an experience of surgical impacted-tooth removal affected the hemodynamic parameters. Decreased blood pressure and heart rate were noted before and during the second surgery. The alterations in hemodynamic parameters, such as the blood pressure and heart rate, during surgical impacted-tooth removal was within the normal range and clinically safe. This study indicated that patients who had a prior experience tended to be more relieved of anxiety; however, a clear relation between an experience of surgical impacted-tooth removal and pain perception in patients was not found.
ACKNOWLEDGMENTS
The authors would like to acknowledge the staff and dental assistants, including our colleagues, in the Department of Oral and Maxillofacial Surgery, Faculty of Dentistry, Mahidol University.
References
1. Gatchel RJ, Ingersoll BD, Bowman L, Robertson MC, Walker C. The prevalence of dental fear and avoidance: a recent survey study. J Am Dent Assoc. 1983; 107:609–610. PMID: 6579095.

2. Kaufman E, Epstein JB, Naveh E, Gorsky M, Gross A, Cohen G. A survey of pain, pressure, and discomfort induced by commonly used oral local anesthesia injections. Anesth Prog. 2005; 52:122–127. PMID: 16596910.

3. Nusstein J, Steinkruger G, Reader A, Beck M, Weaver J. The effects of a 2-stage injection technique on inferior alveolar nerve block injection pain. Anesth Prog. 2006; 53:126–130. PMID: 17177591.

4. Liau FL, Kok SH, Lee JJ, Kuo RC, Hwang CR, Yang PJ, et al. Cardiovascular influence of dental anxiety during local anesthesia for tooth extraction. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2008; 105:16–26. Epub 2007 Jul 25. PMID: 17656135.

5. Jensen MP, Chen C, Brugger AM. Interpretation of Visual Analog Scale ratings and change scores: a reanalysis of two clinical trials of postoperative pain. J Pain. 2003; 4:407–414. PMID: 14622683.

6. Luyk NH, Beck FM, Weaver JM. A visual analogue scale in the assessment of dental anxiety. Anesth Prog. 1988; 35:121–123. PMID: 3166350.
7. Okawa K, Ichinohe T, Kaneko Y. Anxiety may enhance pain during dental treatment. Bull Tokyo Dent Coll. 2005; 46:51–58. PMID: 16598181.

8. Locker D, Shapiro D, Liddell A. Negative dental experiences and their relationship to dental anxiety. Community Dental Health. 1996; 13:86–92. PMID: 8763138.
9. Edmunds R, Buchanan H. Cognitive vulnerability and the aetiology and maintenance of dental anxiety. Community Dent Oral Epidemiol. 2011; 40:17–25. PMID: 21895734.

10. Kleinknecht RA, Thornlike RM, McGlynn FD, Harkavy J. Factor analysis of the dental fear survey with cross-validation. J Am Dent Assoc. 1984; 108:59–61. PMID: 6582116.

11. Reiss S, Rolf AP, David MG, Richard JM. Anxiety sensitivity, anxiety frequency and the prediction of fearfulness. Behav Res Ther. 1986; 24:1–8. PMID: 3947307.

12. Klages U, Ulusoy O, Kianifard S, Wehrbein H. Dental trait anxiety and pain sensitivity as predictors of expected and experienced pain in stressful dental procedures. Eur J Oral Sci. 2004; 112:477–483. PMID: 15560829.

13. Kim YK, Kim SM, Myoung H. Musical intervention reduces patients’ anxiety in surgical extraction of an impacted mandibular third molar. J Oral Maxillofac Surg. 2011; 69:1036–1045. PMID: 20708320.

14. Klassen JA, Liang Y, Tjosvold L, Klassen TP, Hartling L. Music for pain and anxiety in children undergoing medical procedures: a systematic review of randomized controlled trials. Ambul Pediatr. 2008; 8:117–128. PMID: 18355741.

15. Mobilio N, Gremigni P, Pramstraller M, Vecchiatini R, Calura G, Catapano S. Explaining pain after lower third molar extraction by preoperative pain assessment. J Oral Maxillofac Surg. 2011; 69:2731–2738. PMID: 21835529.

16. Baum C, Huber C, Schneider R, Lautenbacher S. Prediction of experimental pain sensitivity by attention to pain-related stimuli in healthy individuals. Percept Mot Skills. 2011; 112:926–946. PMID: 21853779.

17. Alemany-Martínez A, Valmaseda-Castellón E, Berini-Aytés L, Gay-Escoda C. Hemodynamic changes during the surgical removal of lower third molars. J Oral Maxillofac Surg. 2008; 66:453–461. PMID: 18280377.

18. Rivat C, Becker C, Blugeot A, Zeau B, Mauborgne A, Pohl M, et al. Chronic stress induces transient spinal neuroinflammation, triggering sensory hypersensitivity and long-lasting anxiety-induced hyperalgesia. Pain. 2010; 150:358–368. PMID: 20573451.

19. DeLoach LJ, Higgins MS, Caplan AB, Stiff JL. The visual analog scale in the immediate postoperative period: intrasubject variability and correlation with a numeric scale. Anesth Analg. 1998; 86:102–106. PMID: 9428860.
20. Frabetti L, Checchi L, Finelli K. Cardiovascular effects of local anesthesia with epinephrine in periodontal treatment. Quintessence Int. 1992; 23:19–24. PMID: 1631266.
21. de Morais HH, de Santana Santos T, da Costa Araújo FA, de Freitas Xavier RL, Vajgel A, de Holanda Vasconcellos RJ. Hemodynamic changes comparing 2% lidocaine and 4% articaine with epinephrine 1: 100,000 in lower third molar surgery. J Craniofac Surg. 2012; 23:1204–1211. PMID: 22801130.
22. Ping B, Kiattavorncharoen S, Saengsirinavin C, Im P, Durward C, Wongsirichat N. The efficacy of an elevated concentration of lidocaine HCl in impacted lower third molar surgery. J Dent Anesth Pain Med. 2015; 15:69–76.

23. Lasemi E, Sezavar M, Habibi L, Hemmat S, Sarkarat F, Nematollahi Z. Articaine (4%) with epinephrine (1:100,000 or 1:200,000) in inferior alveolar nerve block: Effects on the vital signs and onset, and duration of anesthesia. J Dent Anesth Pain Med. 2015; 15:201–205.

24. Ping B, Kiattavorncharoen S, Durward C, Im P, Saengsirinavin C, Wongsirichat N. Hemodynamic changes associated with a novel concentration of lidocaine HCl for impacted lower third molar surgery. J Dent Anesth Pain Med. 2015; 15:121–128.

25. Kämmerer PW, Palarie V, Daubländer M, Bicer C, Shabazfar N, Brüllmann D, et al. Comparison of 4% articaine with epinephrine (1:100,000) and without epinephrine in inferior alveolar block for tooth extraction: double-blind randomized clinical trial of anesthetic efficacy. Oral Surg Oral Med Oral Pathol Oral Radiol. 2012; 113:495–499. PMID: 22676931.

26. Vasconcellos RJ, Vasconcelos BC, Genú PR. Influence of local anesthethics with adrenalina 1:100.000 in basic vital constants during third molar surgery. Med Oral Patol Oral Cir Bucal. 2008; 13:E431–E437. PMID: 18587307.
27. Carrera I, Mestre R, Berini L, Gay-Escoda C. Alterations in monitored vita constants induced by various local anesthetics in combination with different vasoconstrictors in the surgical removal of lower third molars. Bull Group Int Rech Sci Stomatol Odontol. 2000; 42:1–10. PMID: 11799734.
28. Fernieini EM, Bennett JD, Silverman DG, Halaszynski TM. Hemodynamic assessment of local anesthetic administration by laser Doppler flowmetry. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2001; 91:526–530. PMID: 11346729.

Fig. 3
Distribution of the levels of the lower third molars in patients included in this study are presented.
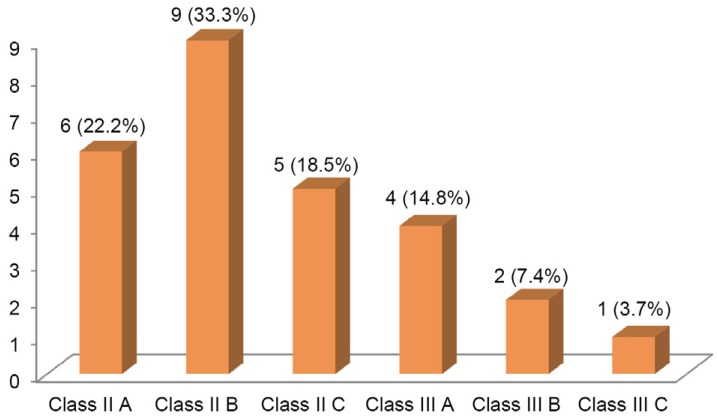
Table 1
The inclusion and exclusion criteria
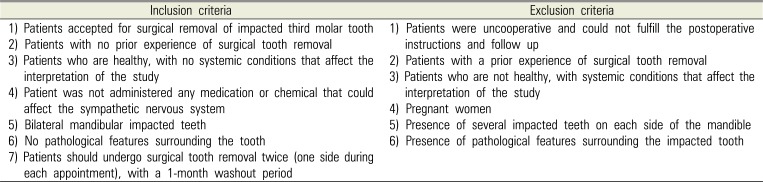
Table 2
Mean pain difference between the first (control group) and second (study group) surgical tooth-removal experiences
| Mean difference between the first and second appointments | Mean ± SD | P value |
|---|---|---|
| Increase in pain (VAS)* during the injection | 1.4 ± 2.6 | 0.780 |
| Decrease in pain (VAS) during the surgery | −1.3 ± 3.4 | 0.062 |
Table 3
Comparison of the mean hemodynamic changes in blood pressure and heart rate between the first (control group) and second (study group) surgical tooth-removal experiences




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download