Abstract
Background
Achilles tendon thickness (ATT) has been associated with increased cardiovascular risk in patients with familial hypercholesterolemia (FH). The aim of this study is to establish the correlation among ATT, obesity and established cardiovascular risk factors such as diabetes mellitus, hypertension, coronary artery disease, peripheral artery disease, smoking, and dyslipidemia.
Methods
In total, 19 patients (male 31.5%, mean age 60.0±12.5) with dyslipidemia and 96 control (male 64.6%, mean age 62.3±8.5) were enrolled. ATT was measured by ultrasonography. Anterioposterior diameter which represents the ATT was measured bilaterally, 4 cm above the insertion of Achilles tendon to the tuber calcite. Dyslipidemia was defined as elevated total cholesterol, triglyceride, or LDL cholesterol, or low levels of HDL cholesterol.
Results
There was no significant differences including ATT between the two groups (for ATT, dyslipidemia group, 0.44±0.04 vs control, 0.45±0.02 cm, p=0.783). There was no significant correlation between ATT and other cardiovascular risk factors except weight (r=0.34, p=0.007) and body mass index (r=0.63, p<0.001). Dyslipidemia was not significantly correlated with ATT (r=0.02, p=0.783). Use of statin was not significantly correlated with ATT (r=0.04, p=0.605).
The reduction of risk factors for cardiovascular disease can prevent the incidence of the cardiovascular diseases. So, the evaluation of an individual's risk of experiencing a future cardiovascular event increasingly forms the basis of clinical guidelines for the prevention of cardiovascular diseases worldwide.1
Life style risk factors including obesity are strongly associated with established cardiovascular risk factors.2-4 The harmful impact of obesity on the incidence of subsequent cardiovascular disease is partly mediated by increased levels of cardiovascular risk factors, in particular hypertension, dyslipidemia and diabetes.5
Tendon pathology inclusive of Achilles tendon thickness (ATT) has been shown to be associated with fat distribution in some previous investigations.6-8 And ATT has been associated with increased cardiovascular risk in patients with familial hypercholesterolemia (FH).9-11
Imaging techniques that have been used for the evaluation of ATT are ultrasonography (US), computed tomography (CT)12,13 and magnetic resonance imaging (MRI).14 Among them, the advantages of ultrasonography are that it is noninvasive, relatively inexpensive, and does not irradiate; hence this measure can be repeatedly performed with no adverse effects on the participant.
We report that assessment of the correlation between ATT and cardiovascular risk factors, especially dyslipidemia, not FH.
During 2009 and 2010, patients who visited cardiovascular center of National Health Insurance Service (NHIS) Ilsan hospital for chest pain, hypertension, dyslipidemia, coronary artery occlusive disease (CAOD) or peripheral artery occlusive disease (PAOD) were enrolled. A total of 19 patients (male 31.5%, mean age 60.0±12.5) with dyslipidemia and 96 control (male 64.6%, mean age 62.3±8.5) were enrolled and patients treated with statin were also included. Dyslipidemia was defined if there was at least one of these: high total cholesterol (>240 mg/dL), triglyceride (TG) (>200 mg/dL), LDL-cholesterol (LDL-C, >160 mg/dL) or low HDL-cholesterol (HDL-C, <40 mg/dL) for low risk group. And the criteria for LDL-C is adapted for very high, high, moderate groups.15
Demographic variables, laboratory data and medication histories were collected. Patients who were diagnosed with or suspected to have familiar hypercholesterolemia were excluded.
This research protocol was complied with ethical principles for medical research involving human subjects from the World Medical Association Declaration of Helsinki. And the Institutional Review Board of the National Health Insurance Corporation Ilsan Hospital approved this study.
The ultrasonographic examination was performed with a real time B-mode scanner with a 5-10MHz electronic linear array transducer (iE33 imaging system, Philips, Andover, MA, US). The optimal focal zone of the transducer was placed at the level of the tendon to assess the tendon structure optimally. Special care was taken to ensure that the probe was parallel to the tendon to avoid the potential artifact of focal hypoechoic areas due to anisotropy. Each ATT was examined ultrasonographically according to a standardized protocol in transverse and longitudinal scans.16,17 Patients were examined in a prone position with both feet hanging free over the edge of the scanning table; the US was performed statically and dynamically. Pressure on the imaged tissue was avoided as much as possible. ATT was measured as the short diameter at the level where the tendon was most thickened. The echo structure of the ATT was considered normal when the typical hypoechoic collagen (fiber bundles) with its hyperechoic internal peritendinea could be seen. US of the patients was performed by one investigator with extensive experience in musculoskeletal ultrasound.
The SPSS software was used for statistical analyses (release 18.0 for Windows; SPSS, Inc., Chicago, IL, USA). Between group comparisons were performed using the independent t-test or the Mann-Whitney U test for continuous variables, and the chi-square test or Fisher's exact test for categorized variables, as appropriate.
Linear correlation analysis was performed between established predictors of cardiovascular disease and ATT in all participants. Pearson correlation coefficients were calculated to assess the validity of the patients, other values compared to the ATT. Statistical hypothesis tests with p less than 0.05 were considered significant. Values are presented as mean±standard deviation or number (%).
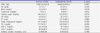
The baseline characteristics of the normal (n=96) and dyslipidemia (n=19) groups are shown in Table 1. Most demographic characteristics were similar in the two groups (p>0.05), including age, sex, height, weight, BMI, DM, hypertension, CAOD, systolic blood pressure, diastolic blood pressure, heart rate. The proportion of those treated with statin, percutaneous coronary intervention and ischemic stroke showed significantly higher in group of dyslipidemia (p<0.05).
Laboratory data were similar in the two groups (p>0.05), including total cholesterol, TG, HDL-C and LDL-C.
There was no significant difference between two groups (for ATT, dyslipidemia group, 0.44±0.04 vs control, 0.45±0.02 cm, p=0.783). ATT was not significantly increased in patients with dyslipidemia (Table 2).
Correlations of ATT and various values were showed in Table 3. Linear correlation analysis revealed a significant correlation between weight, BMI and ATT (for weight, r=0.34, p=0.007; for BMI, r=0.63, p<0.001) (Fig. 1 A and B). ATT was not significantly correlated withage, DM, hypertension, CAOD, PAOD, percutaneous coronary intervention, stroke, dyslipidemia, use of statin. And ATT was not significantly correlated with total cholesterol (r=-0.09, p=0.356), TG (r=-0.04, p=0.629), HDL-C (r=-0.06, p=0.501) and LDL-C (r=-0.03, p=0.694) (Fig. 1 C-F).
Carotid intima-mediathickness (IMT) is very useful and validated marker of atherosclerosis18 and there was a positive correlation between ATT and IMT.19 For the first time higher ATT was found in FH patients with more advanced carotid atherosclerosis, these results may suggest that ATT is associated with carotid atherosclerosis. Moreover, abnormal Achilles tendon echogenicity may be also associated with carotid atherosclerosis. These results may explain why Achilles tendon xanthomas are associated with premature cardiovascular disease.19 For statin treatment, a study presented that statin reduces ATT in FH patients with normal Achilles tendon echostructure.20-23 Atherosclerotic plaque and tendon xanthomas share common mechanisms of lipid accumulation.24 The clue indicating a possible correlation between atherosclerosis and formation of Achilles tendon xanthoma is that patients with both lesions have a similar clinical and biochemical profile.25 Some studies showed lipid profile characteristics of dyslipidemia in subjects who had been with chronic painful midportion Achilles tendinopathy or with Achilles tendon rupture. It showed the possibility of lipid blood levels predisposing individuals to Achilles tendon ruptures. A higher risk for patients with a pathological lipid status has been described by several authors.25 For metabolic syndrome, there was a study revealed that subjects with chronic painful midportion Achilles tendinopathy have a lipid profile characteristic of a dyslipidemia that is most commonly seen a long side the insulin resistance syndrome.26,27 So we can suppose that there might be more than simple inflammation of Achilles tendon and also correlate dyslipidemia or metabolic syndrome with Achilles tendon pathology.
Our study tried to show the difference of ATT between normal and dyslipidemia groups and the correlation between ATT and cardiovascular risk factors (Age, Weight, BMI, DM, Hypertension, CAOD, PAOD, smoking, dyslipidemia, total cholesterol, TG, HDL-C, LDL-C and statin use). However, there was no significant difference of ATT between two groups and no significant correlation between ATT and other cardiovascular risk factors except weight and BMI.
The correlation between obesity and ATT has been previously investigated6-8 and Achilles tendon pathology was reported to be correlated with central or peripheral fat distribution.8 Expansion of adipose tissue depots in the upper body and, in particular the abdominal area, is associated with metabolic dysfunction and increased cardiovascular risk.28 As both lipids and insulin resistance play a central role in this relationship, recent findings associating dyslipidemia and Achilles tendinopathy implicate abdominal fat in the pathoaetiology of Achilles tendinopathy among men.8 Limitations of this study must be acknowledged. First, it was approximately not equal numbers of normal group and dyslipidemia group. The group of dyslipidemia is relatively much smaller than normal group. Second, the sonographic data was performed by a well experienced sonographer but single examiner can cause bias of data and make it difficult to correct the wrong values. And further prospective studies about causality with a larger number of patients are needed.
In conclusion, this study demonstrated that ATT was only significantly positive correlated with BMI and weight however, dyslipidemia was not significantly correlated with ATT. Lipid accumulation of Achilles tendon in dyslipidemia, not FH does not seem to be distinct in this study.
Figures and Tables
Fig. 1
Correlation of Achilles tendon thickness and cardiovascular risk factors.
(A and B) Correlation analysis revealed a significance between weight, BMI and Achilles tendon thickness (for weight, r=0.34, p=0.007; for BMI, r=0.63, p<0.001). (C-F) There was no significant correlation between Achilles tendon thickness and other lipid levels.

References
1. Smith SC Jr, Jackson R, Pearson TA, Fuster V, Yusuf S, Faergeman O, et al. Principles for national and regional guidelines on cardiovascular disease prevention: a scientific statement from the World Heart and Stroke Forum. Circulation. 2004; 109:3112–3121.

2. Wilson PW, D'Agostino RB, Levy D, Belanger AM, Silbershatz H, Kannel WB. Prediction of coronary heart disease using risk factor categories. Circulation. 1998; 97:1837–1847.

3. Mozaffarian D, Wilson PW, Kannel WB. Beyond established and novel risk factors: lifestyle risk factors for cardiovascular disease. Circulation. 2008; 117:3031–3038.
4. Poirier P. Healthy lifestyle: even if you are doing everything right, extra weight carries an excess risk of acute coronary events. Circulation. 2008; 117:3057–3059.
5. Juonala M, Magnussen CG, Berenson GS, Venn A, Burns TL, Sabin MA, et al. Childhood adiposity, adult adiposity, and cardiovascular risk factors. N Engl J Med. 2011; 365:1876–1885.

6. Malliaras P, Cook JL, Kent PM. Anthropometric risk factors for patellar tendon injury among volleyball players. Br J Sports Med. 2007; 41:259–263.

7. Gaida JE, Cook JL, Bass SL, Austen S, Kiss ZS. Are unilateral and bilateral patellar tendinopathy distinguished by differences in anthropometry, body composition, or muscle strength in elite female basketball players? Br J Sports Med. 2004; 38:581–585.

8. Gaida JE, Alfredson H, Kiss ZS, Bass SL, Cook JL. Asymptomatic Achilles tendon pathology is associated with a central fat distribution in men and a peripheral fat distribution in women: a cross sectional study of 298 individuals. BMC Musculoskelet Disord. 2010; 11:41.

9. Hirobe K, Matsuzawa Y, Ishikawa K, Tarui S, Yamamoto A, Nambu S, et al. Coronary artery disease in heterozygous familial hypercholesterolemia. Atherosclerosis. 1982; 44:201–210.

10. Ferrières J, Lambert J, Lussier-Cacan S, Davignon J. Coronary artery disease in heterozygous familial hypercholesterolemia patients with the same LDL receptor gene mutation. Circulation. 1995; 92:290–295.

11. Mabuchi H, Tatami R, Haba T, Ueda K, Ueda R, Ito S, et al. Achilles tendon thickness and ischemic heart disease in familial hypercholesterolemia. Metabolism. 1978; 27:1672–1679.

12. Steinmetz A, Schmitt W, Schuler P, Kleinsorge F, Schneider J, Kaffarnik H. Ultrasonography of achilles tendons in primary hypercholesterolemia. Comparison with computed tomography. Atherosclerosis. 1988; 74:231–239.

13. Durrington PN, Adams JE, Beastall MD. The assessment of Achilles tendon size in primary hypercholesterolaemia by computed tomography. Atherosclerosis. 1982; 45:345–358.

14. Bude RO, Adler RS, Bassett DR. Diagnosis of Achilles tendon xanthoma in patients with heterozygous familial hypercholesterolemia: MR vs sonography. AJR Am J Roentgenol. 1994; 162:913–917.

15. European Association for Cardiovascular Prevention & Rehabilitation. Reiner Z, Catapano AL, De Backer G, Graham I, et al. ESC/EAS Guidelines for the management of dyslipidaemias: the Task Force for the management of dyslipidaemias of the European Society of Cardiology (ESC) and the European Atherosclerosis Society (EAS). Eur Heart J. 2011; 32:1769–1818.
16. Scheel AK, Schettler V, Koziolek M, Koelling S, Werner C, Müller GA, et al. Impact of chronic LDL-apheresis treatment on Achilles tendon affection in patients with severe familial hypercholesterolemia: a clinical and ultrasonographic 3-year follow-up study. Atherosclerosis. 2004; 174:133–139.

17. Backhaus M, Burmester GR, Gerber T, Grassi W, Machold KP, Swen WA, et al. Guidelines for musculoskeletal ultrasound in rheumatology. Ann Rheum Dis. 2001; 60:641–649.

18. Chambless LE, Heiss G, Folsom AR, Rosamond W, Szklo M, Sharrett AR, et al. Association of coronary heart disease incidence with carotid arterial wall thickness and major risk factors: the Atherosclerosis Risk in Communities (ARIC) Study, 1987-1993. Am J Epidemiol. 1997; 146:483–494.

19. Kiortsis DN, Argyropoulou MI, Xydis V, Tsouli SG, Elisaf MS. Correlation of Achilles tendon thickness evaluated by ultrasonography with carotid intima-media thickness in patients with familial hypercholesterolemia. Atherosclerosis. 2006; 186:228–229.

20. Illingworth DR, Cope R, Bacon SP. Regression of tendon xanthomas in patients with familial hypercholesterolemia treated with lovastatin. South Med J. 1990; 83:1053–1057.

21. Lind S, Olsson AG, Eriksson M, Rudling M, Eggertsen G, Angelin B. Autosomal recessive hypercholesterolaemia: normalization of plasma LDL cholesterol by ezetimibe in combination with statin treatment. J Intern Med. 2004; 256:406–412.

22. Inazu A, Koizumi J, Kajinami K, Kiyohar T, Chichibu K, Mabuchi H. Opposite effects on serum cholesteryl ester transfer protein levels between long-term treatments with pravastatin and probucol in patients with primary hypercholesterolemia and xanthoma. Atherosclerosis. 1999; 145:405–413.

23. Tsouli SG, Xydis V, Argyropoulou MI, Tselepis AD, Elisaf M, Kiortsis DN. Regression of Achilles tendon thickness after statin treatment in patients with familial hypercholesterolemia: an ultrasonographic study. Atherosclerosis. 2009; 205:151–155.

24. Tsouli SG, Kiortsis DN, Argyropoulou MI, Mikhailidis DP, Elisaf MS. Pathogenesis, detection and treatment of Achilles tendon xanthomas. Eur J Clin Invest. 2005; 35:236–244.

25. Hata Y, Shigematsu H, Tsushima M, Oikawa T, Yamamoto M, Yamauchi Y, et al. Serum lipid and lipoprotein profiles in patients with xanthomas: a correlative study on xanthoma and atherosclerosis (I). Jpn Circ J. 1981; 45:1236–1242.

26. Mathiak G, Wening JV, Mathiak M, Neville LF, Jungbluth K. Serum cholesterol is elevated in patients with Achilles tendon ruptures. Arch Orthop Trauma Surg. 1999; 119:280–284.





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download