This article has been
cited by other articles in ScienceCentral.
I. INTRODUCTION
Tissue engineering science has been in varying stages of development and progress to provide an alternative method for repairing damaged tissues. The dental pulps have long been considered a vulnerable tissue to infection and trauma which frequently leads to irreversible inflammatory conditions. The root canal treatment by removing the diseased pulps has been the most common treatment option. While some investigators in the past attempted to regenerate the pulp tissue, no desirable results were obtained and these efforts have not been actively pursued in the recent decades. Even the more conservative approach such as vital pulp therapy has not been a popular clinical choice due to lack of predictable results.
Dental pulp is a loose connective tissue, with extensive vascular and nerve supply, containing predominantly fibers and ground substance that make up the extracellular matrix (ECM), and cellular component including mainly fibroblasts and undifferentiated mesenchymal cells. The uniquely specialized pulp cells(odontoblasts) are lining against the dentinal wall and their processes extend into the dentinal tubules. The volume of the mature pulp tissue is very small and so it appears relatively less difficult to regenerate this small volume of soft tissue than larger organs or tissues. However, it is considered rather difficult to regenerate the entire pulp tissue due to the following reasons: 1) the unique anatomical location of pulp tissue-enclosed in dentin having limited blood supply from one end for the in-growth of new tissue elements; 2) the small size of the pulpal canal space rendering a technically sensitive procedure to implant the regenerated pulpal tissue in vitro into the canal; and 3) the unique microscopic anatomy of pulp tissue, e.g., the odontoblasts and their relationship with the nerve fibers and vessels. While trying to regenerate the exact pulp tissue to its pristine condition appears difficult to achieve, regenerating a pulp connective tissue with vascular structure and nerve fibers appears not impossible.
The goal of tissue engineering is to regenerate living tissue substitutes in order to replace or enhance lost tissue function or structure. To accomplish this, the cells out of tissue must be organized and behave as if they are part of the original tissue by interacting with the surrounding ECM which acts as a supporting material created by the cells as a scaffolding on which to reside
1). The ECM is composed of a variety of macromolecules which can be grouped into four major classes (collagens, proteoglycans, cell interactive glycoproteins, elastic fibers), each of which is responsible for specific ECM characteristics. Type I collagen is the most abundant type of collagen isolated from many adult connective tissues (skin, bone, tendon). Pulp fibroblasts can produce both type I and type III collagens, whereas the majority of collagen molecules produced by odontoblasts are type I
2).
Synthetic matrices fabricated from naturally-derived (e.g., collagen) or synthetic materials (e.g., polyglycolic acid or PGA) are often utilized as a delivery vehicle for these cells and to guide the process of tissue formation
3). It has been shown by Rutherford's group (1999) that the fibroblast cultured from human adult dental pulps seeded onto PGA formed new tissue similar to that of native pulp after implanted into mouse dermis
4). They also found that when pulp cells seeded onto the three different synthetic matrices (PGA fibers, type I collagen hydrogel, or alginate), the growth of the cells was moderate in collagen gel
5). Type I collagen gel has been used to measure the contraction of the collagen gel matrix mixed with bovine aortic endothelial cell
6) or human lung fibroblast
7).
In this study, to characterize the growth behavior of pulp cells in collagen matrix, rat tail type I collagen was mixed with pulp cells from human dental pulp tissue, and the growth of pulp cells and contraction of the collagen gel was estimated. The result of this investigation may help to establish pulp tissue engineering protocol in vitro and in vivo.
II. MATERIALS AND METHOD
Sample collection and Cell culture
Freshly extracted, intact, caries-free third molars (n=10) were obtained from healthy individuals (15-25 years of age) in the Department of Oral Surgery at the UCLA School of Dentistry according to a protocol approved by the UCLA Medical Institutional Review Board. Immediately after extraction, teeth were stored in phosphate buffered saline (PBS) and transported to the laboratory. Teeth were split open and the maximal amount of pulp tissue extracted was divided into several small fragments approximately 2×2 mm in size each. Repeated washing with PBS, pulp fragments were placed in a 60 mm culture dish containing Dulbecco's Modified Eagle Medium (DMEM; Life Technologies/GIBCO BRL, Gaithersburg, MD) supplemented with 10% fetal bovine serum (FBS). Pulp cells outgrown from pulp fragments exhibited a fibroblast-like phenotype and they were allowed to reach confluence and passed at 1:2 ratio until used for experiments (passages 3-8 were used). Cell culture media were supplemented with 100 units/ml penicillin-G, 100 µg/ml streptomycin, and 0.25 µg/ml fungizone (Gemini Bio-Products, Inc., Woodland, CA). In this study, primary pulp cells of fibroblast-like phenotype outgrown from human pulp tissue(passage 3-5) were used for experiments and NIH 3T3 cells grown in the same culture medium for pulp cells were used as a comparison.
1. Collagen gel preparation and collagen gel contraction assay
Rat tail type I collagen was purchased from BD Biosciences (Bedford, MA). Pulp cells were mixed with collagen gel solution [9 parts type I collagen (3.97 mg/ml), 0.023 part 1N NaOH and 1 part 10×PBS] and placed in a microcentrifuge tube kept on ice. This neutralized, isotonic collagen solution was used to minimize injury of pulp cells. The mixture of pulp cells and collagen gel were placed into 96-well plates (0.1 ml/well) and incubated at 37℃ for 30 min to allow gelation. Culture medium (0.2 ml/well) was then added into each well rendering cell/collagen mixture lifted from the bottom and suspended in the medium. The plates were incubated at 37℃ with 5% CO2 and the medium changed every 2-3 days. The area of the gels was measured daily using the grid of the microscope.
2. Cell proliferation on the culture dish and tooth surface
After the pulp tissue from the human 3rd molar were collected, the tooth surface was prepared with diamond bur to fit the 96-well plates and ground with #600 SiC paper, and then sterilized with one hundred times more concentrated penicillin, streptomycin, and fungizone than those used for cell cultures, followed by Betadine, 2% chlorohexidine, and 5.25% NaOCl, in sequence. Trypsinized human dental pulp cells and NIH 3T3 cells (120 cells/mm2) were seeded on the tooth surface and 96 well-plates to compare the proliferation of the two cells. The seeded cells on the tooth surface were trypsinized in every two days for 9 days, and those in 96 wells were trypsinized everyday for 10 days. Detached cells were counted with the Coulter counter.
3. Cell proliferation in the collagen gel matrix
Dental pulp cells and NIH 3T3 cells (3×104 cells/well) were mixed in the collagen gel solution (0.1 ml) prepared as mentioned above and incubated at 37℃, 5% CO2 for 30 minutes. 0.2 ml of a 3 mg/ml solution of type I collagenase (Sigma) in PBS was used for 45 minutes to detach the cells from the cast collagen gel and the number of the cells was counted with the Coulter counter at the different time point for 18 days.
III. RESULTS
1. Collagen gel preparation and collagen gel contraction assay
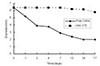
There was no contraction of the collagen gel matrix with NIH 3T3 cells until after day 7. Only minimal contraction (down to 90%) was observed after 17 days. In contrast, the contraction was dramatic with pulp cells through out the course of observation (down to 45% on day 7 and to 31% on day 17) (
Fig. 1).
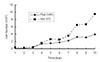
To determine the contraction of the collagen gel matrix affected by the concentration of pulp cells, various numbers of cells were mixed with the collagen and cultured in 96-well plates. The results showed that the collagen matrix with 1.5×10
5 cells/well and 5×10
4 cells/well, contracted down to 30% after 21 days, the matrix with 10
4 cells/well to 35%, and the collagen gel without cells had no contraction (
Fig. 2). It took 3, 5, and 15 days for collagen gel matrix with 1.5×10
5, 5×10
4, and 10
4 cells/well to be half size of the original matrix respectively.
2. Cell proliferation on the culture dish and tooth surface
When cells grown in 96-well plates, the dental pulp cells and NIH 3T3 cells had a similar growth rate up to 4 days after seeding, after which NIH 3T3 cells grew at a faster rate than pulp cells till the end of experimental period (10 days) as demonstrated in
Fig. 3. NIH 3T3 cells had a 25.4-fold increase of the number of the cells, while pulp cells had 19.7-fold increase compared with original number of the cells plated on the 96 well-plates after 10 days(
Fig. 3).
The pulp cells plated on the ground dentin surface proliferated less than the ones grown on the culture dish after 9 days, whereas NIH 3T3 cells proliferated significantly on the tooth surface than on the culture dish. There was a significant increase of NIH 3T3 cells (185-fold) and less increase of pulp cells (7.7-fold) grown on the dentin surface after 9 days (
Fig. 4).
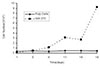
3. Cell proliferation in the collagen gel matrix
Pulp cells showed either minimal or no proliferation in collagen gel matrix up to 18 days after plating, whereas NIH 3T3 started to proliferate significantly after 8 days and continued to grow till 18 days (
Fig. 5).
IV. DISCUSSION
This is the first investigation to compare the contraction of type I collagen in Vitro by culturing pulp-derived human fibroblasts and mouse skin fibroblast(NIH 3T3 cells) three dimensionally. The use of type I collagen gels did not lead to the development of new tissues which resembled native pulp, while the cells adhered and proliferated in the collagen gel.
Collagen-Glycosaminoglycan matrix seeded with porcine dental pulp cells in Vitro decreased in size to less than half of their original diameter by 28 days and the level of α-Smooth-muscle action (SMA) increased with passage number, so SMA containing pulp cells had the capability to contract a collagen-glycosaminoglycan analog of extracellular matrix
in vitro.
8)
Type I collagen has been widely utilized to engineer a variety of tissue type due to its ability to promote cell adhesion and allow for cell-based remodeling, type I collagen is the most abundant type of collagen isolated from many adult connective tissues (skin, bone, tendon)
1), and out of the collagen molecules occurring in the pulp type I and III represent the bulk of the pulp tissue collagen. Because type I is the predominant type and may contribute to the establishment of the architecture of the pulp, in this study commercial rat tail type I collagen was purchased and used as the scaffolds to grow the pulp cells and NIH 3T3 cells three dimensionally
3).
Human lung fibroblasts were cast into two different density of type I rat tail collagen(0.75 mg/ml and 2 mg/ml), the size of the lower density gel after 15 days was smaller than the higher density one
7). The contraction of type I collagen by bovine aortic endothelial(BAE) cells and human dermal fibroblast was compared in collagen gel contraction assay, the fibroblasts contracted rigid gels more effectively in comparison to BAE cells
9).
In this study, human dental pulp cells contracted significantly comparing with NIH 3T3 cells in rat tail type I collagen, nevertheless the proliferation rate of the NIH 3T3 cells cultured in culture dishes and type I collagen gel increased more than human dental pulp cells. The basis for this reduced cellular proliferation rate on the collagen matrices was not identified but seemed to depend on fibrillar organization and required the native(triple helical) conformation of the collagen molecule
10). The more contraction of the collagen gels were made with the increased number of the pulp cells mixed with the same condition of collagen solution, nor contraction without any cells.
When skin fibroblasts are cultured on or in collagen gels, there was a significant reduction in their rate of proliferation
10). Skin fibroblast cultured in the collagen gel and culture dish with human serum had the more proliferation rate than bovine serum, and platelet-derived growth factor reduced mitotic rate observed with the cells on collagen gels
11).
Human dental pulp cells were expected to grow much better on the prepared human tooth surface than NIH 3T3 cells, but it was surprising that the proliferation rate of NIH 3T3 cells was significantly higher than human dental pulp cells. It is not clear if there is some growth factor in the human tooth surface to induce the proliferation of the mouse skin fibroblast.
The pulp tissue engineering may ultimately find clinical application as a novel approach to repair and/or regenerate dental pulp, and they may also provide a useful system to assess the biocompatibility of chemicals utilized in dental practice which come in contact with native pulp. It is possible that engineered dental pulp tissue will provide a model system in which reparative dentinogenesis can be studied. This work may also provide the first step to engineer an entire tooth, and these cell behaviors on the collagen matrix may provide information needed to establish pulp tissue engineering protocols.
V. CONCLUSION
The purpose of this study is to reveal if the rat tail type I collagen can be used as scaffold to grow human dental pulp cells and mouse skin fibroblasts(NIH 3T3 cells) and to characterize the behaviors of those two cells on the collagen gel matrix and ground tooth surface. For the purpose the contraction of the collagen matrix and proliferation rate after those cells were mixed with the type I collagen solution three dimensionally and on the ground tooth surface.
According to this study, the results were as follows:
The contraction of the collagen mix was minimal with NIH 3T3 cells (down to 90% on 17 days), whereas the contraction was dramatic with pulp cells (down to 45% on 7 days and to 31% on 17 days).
When the different number of pulp cells were cultured in collagen gel, the more contraction of the collagen matrix occurred with the more pulp cells, nor contraction of collagen matrix without any cells.
The pulp cells showed either minimal or no proliferation in Rat tail type I collagen up to 18 days after plating, whereas NIH 3T3 started to proliferate significantly after 3-5 days and continued to grow till 18 days.
NIH 3T3 cells proliferated better than pulp cells on the ground tooth surface and culture dishes, proliferation rate of NIH 3T3 cells were significantly high.
These data indicate that pulp cells contract the collagen fibers extensively, whereas NIH 3T3 cells only minimally contract the collagen matrix. While pulp cells proliferate in culture dishes, they grow minimally on human dentin surface and in collagen matrix. NIH 3T3 cells, in contrast, proliferated significantly in all three conditions tested in our experiment, particularly on dentin surface. These cell behaviors may provide information needed to establish pulp tissue engineering protocols.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download