Abstract
Purpose
The aim of the present study was to investigate the relationship between three major allergic diseases, asthma, allergic rhinitis (AR), and atopic dermatitis (AD), and psychological and behavioural problems in preschoolers based on a community survey.
Methods
A cross-sectional survey was conducted using a modified International Study of Asthma and Allergies in Childhood questionnaire to determine the prevalence of symptoms and diagnosed allergic diseases, and a Korean version of the Child Behaviour Checklist to assess internalizing, externalizing, and sleep problems among 780 preschoolers. Five-hundred and seventy-five preschoolers with valid data were included in this study.
Results
The prevalence of lifetime diagnosis and treatment in the past 12 months was 8.7% and 4.4% for asthma, 24.4% and 19.2% for AR, and 35.1% and 16.6% for AD, respectively. Scores for internalizing and sleep problems were significantly higher in those diagnosed with AR. Preschoolers who had been treated for AD in the past 12 months had higher attention problem and attention-deficit/hyperactivity disorder scores. Sleep problems were more severe in moderate to severe AD compared to control and mild AD groups, categorised according to SCOring index of AD. The severity of sleep problems correlated positively with the percentage of eosinophils in peripheral blood.
Conclusions
Psychological and behavioural problems differed among the three major allergic diseases, weaker association for asthma and stronger association for AR and AD. The results of this study may lead to the identification of potential underlying shared mechanisms common to allergic diseases and psychological and behavioural problems.
The prevalence of allergic diseases has continued to escalate worldwide in the past four decades, especially in highly developed countries.1 Pediatric allergic diseases are particularly important for society due to their chronic course and high healthcare costs.2 In Korea, asthma-related costs rank number one among childhood illness, and the socioeconomic burden of the disease is increasing in all ages.3,4 Clinicians have long known that allergic and psychological symptoms tend to co-exist. In 1930, Rowe described "allergic toxemia", a syndrome characterised by fatigue, slowed psychomotor and thought processes, poor memory, irritability and depression.5 Before the underlying inflammatory basis of allergic diseases was discovered, allergic diseases were even considered to be purely psychogenic in origin, with Freud claiming that asthmatic symptoms were a symbolic expression of unconscious conflicts and repressed desires.6 It is now clear that the pathogenesis of allergic diseases is primarily driven by interactions between the immune system and environmental exposure to allergen.7 Meanwhile, a number of studies have discovered the pathophysiological links between stress and allergic disease, thus attempting to explain the overlap.8,9
Previous studies in this area have generally focused on the relationship between specific allergic diseases, such as asthma, allergic rhinitis (AR) or atopic dermatitis (AD), and psychological disturbances. Only two studies have investigated a homogeneous general population sample for the relationship between all three major allergic diseases and psychological problems. Slattery et al.10 conducted a cross-sectional study on 7th grade students and found that "pure" anxiety was associated with asthma and AR, but not AD. Park et al.11 conducted a Child Behaviour Checklist on children from one elementary school with ages ranging from 7 to 11 and found significantly higher internalizing problems in children with asthma and AR. However, no similar study has been conducted on preschool-age children and it is important to evaluate this early age group in order to identify possible mechanisms to explain the relationship between allergic diseases and psychological problems. To our knowledge, this is the first study to systematically investigate the relationship between the three major allergic diseases (asthma, AR and AD) and a broad spectrum of psychological and behavioural problems (including internalizing and externalizing problems) in a general population of preschoolers. The objectives of the present study are 1) to investigate the relationship between allergic diseases and psychological and behavioural problems in preschool children, 2) to reveal the pattern of interaction between psychological and behavioural problems and biomarkers of allergic diseases in this population, and 3) to investigate the relationship between severity of AD, as determined by a physician, and psychological and behavioural problems.
This study recruited 986 preschool children aged 3-7 years old from 17 preschools that were randomly selected from Seoul and Ilsan and Gwacheon in Gyeonggi-do province in Korea. A modified International Study of Asthma and Allergies in Childhood (ISAAC) questionnaire12 was used to determine the prevalence of symptoms and diagnosis of allergic diseases. Parents of 780 preschoolers from 13 preschools consented to participate in psychological evaluation using a Korean version of the Child Behaviour Checklist (CBCL)13 to assess internalizing, externalizing and sleep problems and Diagnostic and Statistical Manual (DSM )-oriented scales. Of the 780 children, 732 (93.8%) parents responded to the ISAAC questionnaire and 575 (73.7%) parents responded to the CBCL questionnaire.
There were no significant differences between participants and non-participants in the CBCL questionnaire (Table 1) in general characteristics, parental allergic disease history and socioeconomic status.
The ISAAC questionnaire is useful as a standardized approach for determining the prevalence of allergic disease. The modified Korean version of ISAAC was previously validated as a tool for assessing allergic symptoms and diagnosis in Korean children.3 The questionnaire consists of three main sections: (1) general characteristics including name, sex, date of birth, height and weight; (2) history of symptoms related to asthma, AR, AD, allergic conjunctivitis and food allergy; and (3) exposure to environmental factors associated with allergic disease. The parents or guardians of the children responded to the questionnaire.
The doctors examined the children at the preschools for the presence of AD. The severity of disease was assessed according to SCORAD (SCOring index of AD) scoring systems. The SCORAD index comprises three parts: extent, intensity (erythema, oedema/papulation, oozing/crusts, excoriations, lichenification, dryness), and subjective symptoms.14 AD was classified into three groups based on the objective SCORAD index: mild (mean score < 15), moderate (15 ≤ mean score ≤ 40), and severe (mean score > 40).15
The CBCL is a scale that is widely used to assess symptoms of mental health and behavioural difficulties among children. CBCL comes in two versions according to the age range of the subjects, and the version for ages 1½-5 was used in this study. The checklist includes subscales assessing symptoms of internalizing, externalizing and sleep problems, and DSM-oriented problem scales.16,17 Studies on the reliability and validity of the CBCL have been extensively summarized in the Achenbach manual, and studies of the Korean-CBCL version have also showed good validity and reliability.18 CBCL has advantage above other psychometrics because it provides standardized T score, thus permitting comparisons between gender and across age groups. These T scores range from 23 to 100. For the Total problem, internalization, and externalization scales, scores of less than 60 are considered non-clinical, 60-63 are borderline, and 64 or more are considered clinical. For DSM-oriented scales, scores of 65 or less are considered non-clinical, 66 through 70 are considered borderline, and 71 or greater are considered clinical. For the internalizing, externalizing and sleep problems, and DSM-oriented scales, the magnitude of the score correlates with the severity of the disorder.
White blood cells and the percentage of peripheral blood eosinophils were measured. Total IgE was measured by fluorescent enzyme immunoassay using the AutoCAP system (Phadia AB, Uppsala, Sweden).
Statistical analysis was carried out using SPSS version 18.0 (SPSS Inc., Chicago, IL, USA). The independent samples t test was used to examine differences in CBCL scores between children with and without symptoms of allergic disorders. The ANOVA test was used to examine differences in CBCL scores and the percentage of eosinophils between three AD groups according to the degree of SCORAD index and the control group. The Pearson's correlation coefficient between eosinophil and CBCL score was obtained by bivariate correlation test.
The prevalence of asthma diagnosis was 7.2% and the prevalence of treatment in the past 12 months was 3.8%. Current asthma, which was defined as previous diagnosis together with asthma symptoms in the past 12 months, affected 3.8% of the study population. The prevalence of AR was as follows: lifetime diagnosis, 25.1%; treatment in the past 12 months, 20.4%; and current AR, 18.8%. With respect to AD, the prevalence of lifetime diagnosis was 34.7%. The prevalence of treatment in the past 12 months and current disease were 15.1% and 20.2%, respectively. The prevalence of asthma diagnosis in CBCL questionnaire participants was lower than in non-participants (Table 2).
Preschoolers diagnosed with asthma did not differ in CBCL scores when compared to non-asthmatic preschoolers. Preschoolers diagnosed with AR showed higher internalizing problems scores (49.73±9.46, 46.64±9.68; P=0.001), sleep problems scores (53.83±5.44, 52.79±4.85; P=0.045), and also higher affective problem DSM-oriented scores (53.94±5.69, 52.64±5.02; P=0.017). There was no difference in CBCL scores between preschoolers diagnosed with AD and those not diagnosed with AD (Table 3).
Preschoolers treated for asthma in the past 12 months had higher anxiety problem DSM-oriented scores (54.90±5.94, 52.46±4.78; P=0.024). Preschoolers treated for AR in the past 12 months had higher scores for internalizing problems (50.21±9.71, 46.70±9.61; P=0.001), DSM-oriented affective problems (54.13±5.85, 52.68±5.03; P=0.016) and anxiety problems (53.46±5.79, 52.31±4.51; P=0.049). Preschoolers treated for AD in the past 12 months had higher scores for attention problems (54.46±6.55, 52.97±5.11; P=0.028) and attention-deficit/hyperactivity disorder (ADHD) DSM-oriented scores (54.60±6.11, 53.01±5.18; P=0.027) (Table 4).
The CBCL scores were compared between the control and AD groups according to severity by objective SCORAD index. There was no difference between the groups in internalizing and externalizing problems. In contrast, the sleep problem score in the moderate-severe AD group was higher than in the control or mild AD groups (P=0.034) (Table 5). The percentage of eosinophils in peripheral blood, but not serum total IgE, was positively correlated with sleep problems (Pearson correlation for eosinophils 0.119, P=0.011).
This is the first study, to our knowledge, to investigate the relationship between all three major allergic diseases and psychological and behavioural problems in a preschool population. Internalizing behavioural problem and sleep problem scores were significantly higher in those diagnosed with AR. Preschoolers who had been treated for asthma in the past 12 months had higher anxiety scores, and those treated for AD had higher scores for attention problems and ADHD. Sleep problems were increased in moderate to severe AD compared to the control and mild AD groups, categorised according to SCORAD index. Sleep problems were positively correlated with the percentage of eosinophils in peripheral blood.
AR in preschoolers was strongly associated with internalizing and sleep problems. Most of the previous studies investigating the relationship between internalizing problems, such as anxiety and depression, and AR have been limited to the adult population,19-21 and mental complications of AR studied in children were confined to sleep disturbance, poor school performance and hyperactivity.22 Recently, Park et al.11 reported that elementary school children had a significantly higher prevalence of internalizing problems, which is consistent with our results, and we conclude that AR in both adults and children is associated with internalizing problems.
Impaired sleep is a serious complication of AR caused by nasal congestion and obstruction and often leads to physical fatigue.23 Based on a survey of general practitioners, adult patients with AR have more difficulty in falling asleep, take more sleeping pills, suffer from nocturnal awakenings, do not believe that they wake up thoroughly rested, and feel that they do not get sufficient sleep.24 In a group of adolescents with AR, Juniper and colleagues found that majority of adolescents had sleep problems, 78% not having a good night's sleep, 75% having difficulty in falling asleep, and 64% waking up in the middle of the night.25 Our study is the first to demonstrate sleep disturbance in preschoolers with AR based on a general population survey.
Preschoolers who had been treated for asthma in the past 12 months scored significantly higher in anxiety problems on the DSM-oriented scale, but the overall correlation with internalizing problems was not significant when compared to preschoolers without asthma. A recent meta-analysis of 26 studies on pediatric asthmatic patients, whose ages ranged from 6 to 18 years, found that there was an increase in internalizing problems among asthmatic children.26 In other studies, a history of diagnosed asthma was significantly associated with higher internalizing problems in 5-year-olds in the general population27 and high-risk 6-year-olds.28 The age range in our study population was 3 to 6 years old, which is the youngest population in existing studies on the relationship between allergic diseases and psychological problems. The prevalence of asthma diagnosis was 7.2% and of asthma treatment was 3.8%, both of which are lower than reported in other studies with older subjects. A follow up study including a larger number of subjects with asthma is needed to confirm the relationship between asthma and psychological problems in the preschool population.
Interestingly, preschoolers treated for AD in the past 12 months had significantly higher attention and hyperactivity problems. The relationship between ADHD and allergic diseases in children is highly controversial. Some studies report increased ADHD symptoms in allergic children,29-31 but this has not been a consistent finding.32-34 It is also interesting to note that only AD was associated with ADHD, and not asthma or AR, which suggests that irritability and decreased concentration due to itching and scratching behaviours in AD preschoolers might mimic the phenomenology of ADHD.
Children with moderate to severe AD categorised by objective SCORAD index by physician examination had increased sleep problems. Disturbed sleep has previously been reported in adults and children with AD.35,36 Patients with AD are more restless in their sleep, wake more often, spend less time asleep, and report more daytime fatigue than those without.37 For example, sleep efficiency evaluated with polysomnography was significantly decreased with increasing symptoms of AD as measured by scratching index (-0.56, P=0.010) and the Rajka and Langeland skin score (0.42, P=0.064).35 However, in another study,38 sleep loss reported by parents only showed a weak correlation with mild, but not moderate or severe, AD categorised by objective SCORAD index. The study authors explained that the results may have been due to the parents not knowing their child's condition at night as they were looked after by a maid. In our study, the children with moderate to severe AD had more sleep problems and higher total IgE and eosinophils in peripheral blood. This latter result indicates that the moderate to severe AD cases had a greater degree of allergic inflammation, which would lead to an increased frequency of pruritus and sleep disturbance.
The mechanisms linking psychological problems to allergic diseases are not well understood. A recent meta-analysis demonstrated a bidirectional relationship between mental health symptoms and allergic diseases,39 suggesting a reciprocally causal relationship. Possible mechanisms to explain how allergic diseases may affect mental health include anxiety and reduced quality of life caused by repeated experiences of breathlessness.26 The impact of stress on the development and expression of allergic diseases may also reflect dysregulation of key neurobiological components of the stress response system. In particular, alterations of the hypothalamic-pituitary-adrenal axis and sympathetic and adrenomedullary system have been reported in children and adults with allergic diseases, as well as those with psychological problems.9 Dysregulation of normal homeostatic neural, endocrine and immunologic mechanisms can occur in the face of chronic stress, leading to chronic hyperarousal or hyporesponsiveness that may affect disease expression.8
Several limitations of this study should be noted. First, the status of allergic diseases and psychological and behavioural problems were all based on parental reporting. Parental reporting has been used in many of the earlier studies investigating the link between psychological problems and allergic disease, and future investigations should attempt to integrate objective measures of allergic disease such as standardised clinical exams. An objective evaluation of psychological and behavioural problems should also be pursued. The Korean versions of the ISAAC questionnaire12 and the CBCL13 are well-established tools for evaluating the prevalence of allergic diseases and psychological and behavioural problems, and have been validated for use in Korea.3,18 We conclude that the use of parental reporting in this study is unlikely to lead to substantial under- or over-reporting of disease severity and prevalence. Second, since this was a cross-sectional survey, it is not possible to assess cause and effect relationships between allergic diseases and psychological and behavioural problems. A prospective general population cohort study starting before the onset of allergic diseases is needed to identify the trajectory and cause and effect relationship of allergic diseases and associated psychological problems. Prospective studies of this nature in the general population are substantially more complicated and difficult to conduct, and cross-sectional studies such as the current one can still make important contributions in suggesting the likelihood of a cause and effect relationship. Third, the prevalence of asthma diagnosis was significantly lower in subjects participating in the psychological assessment, which suggests that the subjects who participated in the assessment may not have been fully representative of the broader study population.
Although there have been a number of previous studies of the link between psychological and allergic diseases, this is the first study to investigate the relationship of all three major allergic diseases to psychological and behavioural disorders during the early, preschool years in the general population. Since allergic diseases are chronic in nature and effect the child extensively, it is important to evaluate the initial period of allergic diseases in this early age group in order to identify possible mechanisms to explain the relationship between allergic diseases and psychological problems. Preschoolers with AR showed significantly higher internalizing and sleep problems, while preschoolers with AD had a greater frequency of ADHD symptoms.
The relationship between allergic diseases and psychological and behavioural problems in preschoolers was different from that in older children11 and adolescents,10 with a weaker association recorded for asthma and a stronger association for AR and AD. This difference may reflect the change in prevalence of allergic diseases with age. The results of this study may lead to the identification of underlying mechanisms common to allergic diseases and psychological and behavioural problems.
Figures and Tables
Table 1
Demographic characteristics of study participants and non-participants
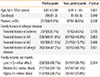
Table 2
Prevalence of allergic diseases from study participants and non-participants
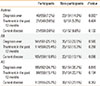
Table 3
Comparison of CBCL scores between preschoolers diagnosed with each allergic disease and preschoolers without diagnosis

Table 4
Comparison of CBCL scores between preschoolers treated for each allergic disease in the past 12 months and preschoolers without treatment

Table 5
Comparison of CBCL scores between controls, children with mild atopic dermatitis and children with moderate to severe atopic dermatitis according to the SCORAD index

ACKNOWLEDGMENTS
This study was supported by a grant of the Korea Healthcare Technology R&D Project, Ministry for Health and Welfares, Republic of Korea (A092076).
References
1. Asher MI, Montefort S, Björkstén B, Lai CK, Strachan DP, Weiland SK, Williams H. ISAAC Phase Three Study Group. Worldwide time trends in the prevalence of symptoms of asthma, allergic rhinoconjunctivitis, and eczema in childhood: ISAAC phases one and three repeat multicountry cross-sectional surveys. Lancet. 2006; 368:733–743.
2. O'Connell EJ. The burden of atopy and asthma in children. Allergy. 2004; 59:Suppl 78. 7–11.
3. Hong SJ, Lee MS, Sohn MH, Shim JY, Han YS, Park KS, Ahn YM, Son BK, Lee HB. Korean ISAAC Study Group. Self-reported prevalence and risk factors of asthma among Korean adolescents: 5-year follow-up study, 1995-2000. Clin Exp Allergy. 2004; 34:1556–1562.
4. Cho SH, Park HW, Rosenberg DM. The current status of asthma in Korea. J Korean Med Sci. 2006; 21:181–187.
5. Rowe AH. Allergic toxemia and migraine due to food allergy: report of cases. Cal West Med. 1930; 33:785–793.
6. Freud S. Inhibitions, symptoms and anxiety. London: Hogarth Press;1959.
7. Anandan C, Sheikh A. Preventing development of allergic disorders in children. BMJ. 2006; 333:485.
8. Wright RJ, Cohen RT, Cohen S. The impact of stress on the development and expression of atopy. Curr Opin Allergy Clin Immunol. 2005; 5:23–29.
9. Wright RJ, Rodriguez M, Cohen S. Review of psychosocial stress and asthma: an integrated biopsychosocial approach. Thorax. 1998; 53:1066–1074.
10. Slattery MJ, Essex MJ. Specificity in the association of anxiety, depression, and atopic disorders in a community sample of adolescents. J Psychiatr Res. 2011; 45:788–795.
11. Park J, Kim BJ, Kwon JW, Song YH, Yu J, Kim HB, Lee SY, Kim WK, Jee HM, Kim KW, Kim KE, Hong SJ, Shin YJ. Patterns of psychosocial adaptation and allergic disorders in Korean schoolchildren. Int Arch Allergy Immunol. 2011; 154:249–257.
12. The International Study of Asthma and Allergies in Childhood (ISAAC) Steering Committee. Worldwide variation in prevalence of symptoms of asthma, allergic rhinoconjunctivitis, and atopic eczema: ISAAC. Lancet. 1998; 351:1225–1232.
13. Oh KJ, Lee H, Hong KE, Ha EH. Manual for the Korean child behavior checklist. Seoul: Joongang Jeokseong Press;1997.
14. Severity scoring of atopic dermatitis: the SCORAD index. Consensus Report of the European Task Force on Atopic Dermatitis. Dermatology. 1993; 186:23–31.
15. Oranje AP, Glazenburg EJ, Wolkerstorfer A, de Waard-van der Spek FB. Practical issues on interpretation of scoring atopic dermatitis: the SCORAD index, objective SCORAD and the three-item severity score. Br J Dermatol. 2007; 157:645–648.
16. Achenbach TM. Manual for the child behavior checklist/4-18 and 1991 profile. Burlington, VT: Department of Psychiatry, University of Vermont;1991.
17. Achenbach TM, Edelbrock C. Manual for the child behavior checklist and revised child behavior profile. Burlington, VT: Department of Psychiatry, University of Vermont;1993.
18. Ha EH, Oh KJ. Standardization of K-CBCL: analysis of validity and reliabiltiy. Seoul: Korean Clinical Psychology Association;1997.
19. Addolorato G, Ancona C, Capristo E, Graziosetto R, Di Rienzo L, Maurizi M, Gasbarrini G. State and trait anxiety in women affected by allergic and vasomotor rhinitis. J Psychosom Res. 1999; 46:283–289.
20. Cuffel B, Wamboldt M, Borish L, Kennedy S, Crystal-Peters J. Economic consequences of comorbid depression, anxiety, and allergic rhinitis. Psychosomatics. 1999; 40:491–496.
21. Marshall PS, O'Hara C, Steinberg P. Effects of seasonal allergic rhinitis on fatigue levels and mood. Psychosom Med. 2002; 64:684–691.
22. Blaiss MS. Pediatric allergic rhinitis: physical and mental complications. Allergy Asthma Proc. 2008; 29:1–6.
23. Santos CB, Pratt EL, Hanks C, McCann J, Craig TJ. Allergic rhinitis and its effect on sleep, fatigue, and daytime somnolence. Ann Allergy Asthma Immunol. 2006; 97:579–586.
24. Léger D, Annesi-Maesano I, Carat F, Rugina M, Chanal I, Pribil C, El Hasnaoui A, Bousquet J. Allergic rhinitis and its consequences on quality of sleep: an unexplored area. Arch Intern Med. 2006; 166:1744–1748.
25. Juniper EF, Guyatt GH, Dolovich J. Assessment of quality of life in adolescents with allergic rhinoconjunctivitis: development and testing of a questionnaire for clinical trials. J Allergy Clin Immunol. 1994; 93:413–423.
26. McQuaid EL, Kopel SJ, Nassau JH. Behavioral adjustment in children with asthma: a meta-analysis. J Dev Behav Pediatr. 2001; 22:430–439.
27. Alati R, O'Callaghan M, Najman JM, Williams GM, Bor W, Lawlor DA. Asthma and internalizing behavior problems in adolescence: a longitudinal study. Psychosom Med. 2005; 67:462–470.
28. Klinnert MD, Nelson HS, Price MR, Adinoff AD, Leung DY, Mrazek DA. Onset and persistence of childhood asthma: predictors from infancy. Pediatrics. 2001; 108:E69.
29. Beyreiss J, Roth N, Beyer H, Kropf S, Shlenzka K, Schmidt A, Roscher G. Coincidence of immune (atopic dermatitis) and behavioral (attention deficit) disorders in children: empirical data. Act Nerv Super (Praha). 1988; 30:127–128.
30. Roth N, Beyreiss J, Schlenzka K, Beyer H. Coincidence of attention deficit disorder and atopic disorders in children: empirical findings and hypothetical background. J Abnorm Child Psychol. 1991; 19:1–13.
31. Blank R, Remschmidt H. Hyperkinetic syndrome: the role of allergy among psychological and neurological factors. Eur Child Adolesc Psychiatry. 1994; 3:220–228.
32. Daud LR, Garralda ME, David TJ. Psychosocial adjustment in preschool children with atopic eczema. Arch Dis Child. 1993; 69:670–676.
33. Gaitens T, Kaplan BJ, Freigang B. Absence of an association between IgE-mediated atopic responsiveness and ADHD symptomatology. J Child Psychol Psychiatry. 1998; 39:427–431.
34. Mitchell EA, Aman MG, Turbott SH, Manku M. Clinical characteristics and serum essential fatty acid levels in hyperactive children. Clin Pediatr (Phila). 1987; 26:406–411.
35. Bender BG, Ballard R, Canono B, Murphy JR, Leung DY. Disease severity, scratching, and sleep quality in patients with atopic dermatitis. J Am Acad Dermatol. 2008; 58:415–420.
36. Bender BG, Leung DY. Sleep disorders in patients with asthma, atopic dermatitis, and allergic rhinitis. J Allergy Clin Immunol. 2005; 116:1200–1201.
37. Reuveni H, Chapnick G, Tal A, Tarasiuk A. Sleep fragmentation in children with atopic dermatitis. Arch Pediatr Adolesc Med. 1999; 153:249–253.
38. Hon KL, Leung TF, Wong Y, Fok TF. Lesson from performing SCORADs in children with atopic dermatitis: subjective symptoms do not correlate well with disease extent or intensity. Int J Dermatol. 2006; 45:728–730.
39. Chida Y, Hamer M, Steptoe A. A bidirectional relationship between psychosocial factors and atopic disorders: a systematic review and meta-analysis. Psychosom Med. 2008; 70:102–116.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download