Abstract
Objectives
It is to evaluate the effect of black cohosh on genital atrophy and its adverse effect in postmenopausal women.
Methods
A total of 100 postmenopausal women having moderate to severe degree of climacteric symptoms were randomly allocated to receive black cohosh combined proparation (n = 50) or placebo (n = 50) daily for 12 weeks. A total of seventy eight subjects completed the study. The effect of black cohosh on vaginal atrophy was evaluated by measuring Maturation value (MV). MV was determined from vaginal smear at 0 and 12 weeks of treatment. Safety assessment included vital signs, physical examinations, adverse events, and routine laboratory parameters. Assessments were carried out at the beginning, and after 4, 8, and 12 weeks of treatment.
Results
The mean (± standard deviation) MV decreased 0.18 (0.48 ± 0.33 to 0.30 ± 0.24) in the black cohosh group and 0.13 (0.44 ± 0.31 to 0.31 ± 0.22) in the placebo group. There was no statistical difference between the groups. But adverse events were observed in 7 (14%) patients in the black cohosh group and 6 (12%) patients in the placebo group, without statistical significance. No significant effects were observed on blood pressure, heart rate, body temperature, physical findings, and laboratory values. Black cohosh was well tolerated.
Women live in a menopausal state after approximately age 50, which is for one third of their lifespan. Thus the menopausal phase has increased in length with the extension of the average life span. Therefore, postmenopausal diseases, including menopausal disorders, have become an important issue in the field of public health. Hormonal replacement therapy, which has been considered the best solution for solving these problems, has been used for decades. However, concerns about the safety and efficacy of existing hormonal replacement therapy became serious after the Women's Health Initiative (WHI)1,2 and Women's Health Initiative Memory Study (WHIMS)3 studies reported that the risk of breast cancer, cardiovascular diseases, thromboembolism, and dementia were increased by hormone replacement. As a result, a large number of menopausal women have discontinued taking hormones, and have turned to herbs, phytoestrogens, and dietary supplements instead because they worry about their reactions to hormones. These alternatives have been advertized as natural plant hormones that function like estrogen in selected tissues. Thus, they have been recognized as safer substitutes for hormones in terms of complications such as breast cancer.
Black cohosh has been most commonly used as a hormone substitute in western countries, and has been studied widely for treatment of menopausal symptoms. Black cohosh, a plant of the family of ranunculuses, is native to North America, and its root and rhizome have been used for medical treatments of conditions such as gynecological diseases over the past several hundred years. Black cohosh, which was first used by Native Americans, has been used as phytotherapy for the treatment of menopausal symptoms for 50 years in Europe. The German Commission E, which is a committee on herbal medicines in Germany, approved cohosh as a medicine for menopausal symptoms as well as premenstrual syndrome and menstrual pain. Recently, an effect of cohosh on menopausal symptoms such as febrile flushing has been proven in double-blind, placebo-controlled studies.4~13 Thus, cohosh has been used as a substitute for hormone replacement therapy. Although cohosh has been widely used to reduce menopausal symptoms for a long time, the effect of atrophy on the urogenital system has not yet been clarified, and controversy over the mechanism of action and characteristics of its estrogen remain. Recently, 4 cases of acute hepatic failure were reported in women who took varieties of cohosh; therefore, a concern over hepatotoxicity was raised. Cohosh's hepatotoxicity, which has been previously reported, was reviewed at the National Institutes of Health Workshop on the Safety of Black Cohosh in Clinical Studies in 2004, and it was recommended that safety assessment checklists such as liver function tests be included in clinical research on cohosh.14
Therefore, following existing studies on the effects of cohosh complex medication on menopausal symptoms, this study investigated the effect of cohosh on vaginal atrophy in menopausal women by observing changes in the vaginal maturation value, which is the secondary outcome variable of this study. Whether a cohosh complex medication was safe to use for menopausal women over the short term was investigated by comparing side effects and laboratory tests including liver enzymes of placebo and control groups.
The subjects were 100 menopausal women who had visited any of 3 university hospitals within 13 months, from June 2007 to July 2010. The study design was retrospective chart review.
Among the naturally menopausal women over 40 who had experienced amenorrhea for at least a year, and those with amenorrhea for at least 6 months with an follicle-stimulating hormone (FSH) blood concentration of 40 mIU/mL, women were included as subjects who had menopausal symptoms above the moderate level, with a Kupperman index score of over 20. The following cases were excluded: those with a current or past history of malignancy, bilateral ovariectomy, hysterectomy, chemotherapy, radiotherapy on the pelvis, psychiatric treatment, hormonal replacement therapy within the 3 months before taking the medication of this study, cardiovascular disease, cerebrovascular disease, hepatic dysfunction (specifically, those with 2 times the upper limit of normal values of liver enzymes), phytosensitivity reaction (a contraindication for St. John's wort), taking other medications in other clinical trials within 30 days before starting this study, and planning to take other medications for other clinical trials during the period of this study.
Among the 100 naturally menopausal women, cohosh complex medication and a placebo were allotted randomly to groups of 50 women each. Two tablets of the placebo or two tablets of the cohosh complex medication were prescribed twice a day for groups of 50 women for 12 weeks. The placebo consisted of lactose, microcrystalline cellulose, and sodium starch glycolate. A tablet of Feramin-Q® (Dongkook Pharmaceutical, Seoul, Korea) contained 0.0364Ml (Food and Drug Administration [FDA] notice) cohosh extract (84 mg) and 80% St. John's wort methanol extract (exhibit specifications).
Pap smears were performed before and after the 12-week prescription. At least 100 squamous cells from the vaginal cell smears were classified into 3 groups based on morphological characteristics: parabasal cells, intermediate cells, and superficial cells. The percentage of each cell was calculated. The vaginal maturation value was calculated by multiplying the percentage of the parabasal cells by 0, the intermediate cells by 0.5, and the superficial cells by 1.0. The range of the vaginal maturation value was from 0 to 1. Values close to 0 mean severe vaginal atrophy, and values close to 1 reflect the effect of estrogen; most of the smeared cells were squamous cells. The difference in vaginal maturation values between the baseline and treatment data after 12 weeks was analyzed for each group.
The incidence rate, severity, and types of adverse reactions that were observed during this study, and reported by subjects in intention-to-treat (ITT) patients, 50 women with Feramin-Q, and 50 women with placebo, were analyzed. Vital signs including blood pressure, pulse, and temperature were taken, and a physical examination were performed. All adverse reactions were recorded from data at baseline and after 4, 8, and 12 weeks of treatment. Laboratory tests, such as routine blood tests, routine chemistry, and routine urinalysis were performed before and after the 12 weeks of administration.
The article have studied from patients under institutional review board (IRB) approval of Kosin medical center (IRB No.KMC IRB 11-07).
Statistical Analysis System (SAS) version 8.1 (SAS Institute Inc., Cary, NC, USA) was used for statistical analysis. The difference in vaginal maturation values between baseline and treated data was analyzed with an unpaired Student's t-test. The incidence rate of adverse reactions in each group was analyzed with Fisher's exact test. An unpaired Student's t-test was used to analyze differences in vital signs. The difference in laboratory tests between baseline and treated data was also analyzed with an unpaired Student's t-test. P < 0.05 was considered statistically significant.
Among the 100 patients who were randomly assigned to a cohosh or placebo group, excepting 22 patients who discontinued this trial, the number of Pre-Protocol (PP) patients who completed the clinical trial for 12 weeks was 78: 40 patients taking the cohosh complex medication, and 38 patients taking the placebo.
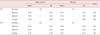
There were no significant differences in age, weight, height, blood pressure, or pulse between the two groups (Table 1). There were no significant differences in the combined drugs or medical history.
The vaginal maturation value in the PP group taking the cohosh complex medication had decreased by an average 0.18 after 12 weeks of administration, and the value of the placebo group had decreased an average of 0.13 from baseline data. There was no significant difference between the two groups. The vaginal maturation value in the ITT group taking the cohosh complex medication had decreased an average of 0.19 after 12 weeks of administration, and the value of the placebo group had decreased an average of 0.11 from baseline data. There was no significant difference between the two groups (Table 2).
The most frequent adverse reaction was a gastrointestinal disorder, with 4 patients (10.0%), followed by reproductive system and breast disorders with a single patient (2.5%), and a systemic disorder, local disorder, clinical tests, skin, and subcutaneous tissue disorder with a patient (2.5%) in the cohosh-complex medication group.
In the placebo group, the most frequent adverse reaction was a gastrointestinal disorder, with 3 patients (7.8%), and next was reproductive system and breast disorders, with 2 patients (13.2%).
None of the 15 patients who dropped out early did so due to adverse reactions. The number of patients who had adverse reactions related to the prescribed medication was 7 (14%), in the cohosh-complex medication group, which was somewhat higher than the placebo group, in which 6 (12%) had adverse reactions. The types of adverse reactions in the cohosh-complex medication and the placebo groups were equal. It is thought that the causes of adverse reactions were not related to the cohosh-complex medication.
Black cohosh (botanical name: Cimicifuga racemosa), which is native to North America, is a perennial plant. Its root and rhizome have been used for medical treatments such as gynecological diseases over the past few hundred years. Black cohosh, which was first used by the American Indians, has been used as phytotherapy for the treatment of menopausal symptoms for 50 years in Europe. It has been studied widely for the treatment of menopausal symptoms. The treatment effects and safety of cohosh have been studied in over 3,800 menopausal women, and the use of cohosh has been permitted to treat menopausal symptoms by the European Scientific Cooperative on Phytotherapy (2003) and World Health Organization (2002).15 The use of a cohosh with modified lifestyle was recommended by North American Menopause Society to treat mild menopausal symptoms.16 The use of cohosh is encouraged for treating menopausal symptoms including sleep disorders, menopausal depression, and febrile flushing lasting at least 6 months.17
Cohosh consists of actein, cimicifugoside, and triterpene glycoside. In addition, it contains fukiictks, piscidic acid, salicylic acid, alkaloids, flavonoids, and tannins.18,19 However, recently, it has been thought that cohosh does not contain formononetin, which is commonly known as phytoestrogen. Remifemin® had been used in most clinical studies, and contains 20 mg cohosh extract, which means it contains 1 mg triterpene standardized to 27-deoxyactin. The recent recommended daily allowance is a total 40 mg, which is divided into 2 doses of 20 mg a day, and the maximum treatment effect appears within 4-8 weeks.
At least 10 randomized controlled studies have been reported.4~13 The effect of cohosh has been evaluated in most studies by comparing an estrogen and a placebo group with the menopause rating scale (MRS), which consists of 10 menopausal symptoms items. Wuttke et al.4 reported that CR BNO 1055 was prescribed at 40 mg a day for 12 weeks in 62 menopausal women, and the decrease in the MRS score in the cohosh extract group was similar to that in the estrogen group. In addition, there were beneficial changes of bone metabolism, a significant increase in superficial cells, and a significant improvement in menopausal symptoms related to atrophy symptoms such as sexual dysfunction, vaginal dryness, urinary symptoms, and the symptoms in joints and muscles. Moreover, it was assumed that cohosh extracts had a selected estrogen receptor modulator (SERM) function because, unlike estrogen, the cohosh did not affect endometrial thickness. Osmers et al.5 reported that MRS scores were significantly improved in 304 menopausal women by prescribing 40 mg isopropanol for 12 weeks. In particular, it was more effective on early menopausal symptoms, and among them, it was the most effective on the relief of febrile flushing. Frei-Kleiner et al.6 reported that the effect of cohosh was superior to the effect of a placebo in women who had menopausal symptoms with scores over 20 on the Kupperman menstrual index. There was no significant change in the Karyopyknotic index of vaginal mucosa. Most studies have reported that the effect of cohosh was superior to the effect of a placebo or similar to the effect of estrogen for relieving the acute symptoms, such as febrile flushing and depression, that frequently occur in the early menopausal stage. However, past studies were limited in drawing clear conclusions about the effectiveness of cohosh because different types of cohosh medication were used, and various doses were prescribed in these studies. In addition, the mechanism of action, characteristics of estrogen, and the effect of cohosh on urogenital atrophy related to safety have not been clarified.
Cohosh has been used as a safe substitute for febrile flushing and other menopausal symptoms over short periods; however, it has not been prescribed for long periods of time. Therefore, the safety of usage for more than 6 months is unknown. Generally, unlike prescription medications, natural herbal supplements are not controlled. Thus, the quality of products, the safety, and the purity vary. In addition, safety should be considered because herbal supplements can produce interactions with prescribed medications.
In this study, observing changes in vaginal maturation values after prescribing the cohosh and St. John's wort for 12 weeks in natural menopausal women who had menopausal symptoms above the moderate level, it was shown that cohosh did not perform an estrogen-like function on the vagina because there was no significant difference between the cohosh and St, John's wort-complex medication and placebo groups. There was no significant difference in adverse reaction rates between the cohosh-complex medication and placebo groups, and there were no severe adverse reactions which could results in discontinuity of the study. The types of adverse reactions in the two groups were equal, and the cause of adverse reactions in the cohosh-complex group was not related with cohosh-complex medication. In addition, the safety of cohosh in the short term was demonstrated because the cohosh-complex medication did not affect the results of laboratory tests or vital signs.
In conclusion, black cohosh did not exert estrogenic effects on the vaginal atrophy. Further studies on the long-term safety and appropriate doses of cohosh are needed.
Figures and Tables
References
1. Keller KB, Lemberg L. Estrogen plus progestin, benefits and risks: the "Women's Health Initiative" trials. Am J Crit Care. 2005. 14:157–160.
2. Anderson GL, Limacher M, Assaf AR, Bassford T, Beresford SA, Black H, et al. Effects of conjugated equine estrogen in postmenopausal women with hysterectomy: the Women's Health Initiative randomized controlled trial. JAMA. 2004. 291:1701–1712.
3. Coker LH, Espeland MA, Rapp SR, Legault C, Resnick SM, Hogan P, et al. Postmenopausal hormone therapy and cognitive outcomes: the Women's Health Initiative Memory Study (WHIMS). J Steroid Biochem Mol Biol. 2010. 118:304–310.
4. Wuttke W, Seidlová-Wuttke D, Gorkow C. The Cimicifuga preparation BNO 1055 vs. conjugated estrogens in a double-blind placebo-controlled study: effects on menopause symptoms and bone markers. Maturitas. 2003. 44:Suppl 1. S67–S77.
5. Osmers R, Friede M, Liske E, Schnitker J, Freudenstein J, Henneicke-von Zepelin HH. Efficacy and safety of isopropanolic black cohosh extract for climacteric symptoms. Obstet Gynecol. 2005. 105:1074–1083.
6. Frei-Kleiner S, Schaffner W, Rahlfs VW, Bodmer C, Birkhäuser M. Cimicifuga racemosa dried ethanolic extract in menopausal disorders: a double-blind placebo-controlled clinical trial. Maturitas. 2005. 51:397–404.
7. Rotem C, Kaplan B. Phyto-Female Complex for the relief of hot flushes, night sweats and quality of sleep: randomized, controlled, double-blind pilot study. Gynecol Endocrinol. 2007. 23:117–122.
8. van der Sluijs CP, Bensoussan A, Chang S, Baber R. A randomized placebo-controlled trial on the effectiveness of an herbal formula to alleviate menopausal vasomotor symptoms. Menopause. 2009. 16:336–344.
9. Uebelhack R, Blohmer JU, Graubaum HJ, Busch R, Gruenwald J, Wernecke KD. Black cohosh and St. John's wort for climacteric complaints: a randomized trial. Obstet Gynecol. 2006. 107:247–255.
10. Wuttke W, Gorkow C, Seidlová-Wuttke D. Effects of black cohosh (Cimicifuga racemosa) on bone turnover, vaginal mucosa, and various blood parameters in postmenopausal women: a double-blind, placebo-controlled, and conjugated estrogens-controlled study. Menopause. 2006. 13:185–196.
11. Bai W, Henneicke-von Zepelin HH, Wang S, Zheng S, Liu J, Zhang Z, et al. Efficacy and tolerability of a medicinal product containing an isopropanolic black cohosh extract in Chinese women with menopausal symptoms: a randomized, double blind, parallel-controlled study versus tibolone. Maturitas. 2007. 58:31–41.
12. Reed SD, Newton KM, LaCroix AZ, Grothaus LC, Grieco VS, Ehrlich K. Vaginal, endometrial, and reproductive hormone findings: randomized, placebo-controlled trial of black cohosh, multibotanical herbs, and dietary soy for vasomotor symptoms: the Herbal Alternatives for Menopause (HALT) Study. Menopause. 2008. 15:51–58.
13. Newton KM, Reed SD, Grothaus L, Ehrlich K, Guiltinan J, Ludman E, et al. Reprint of The Herbal Alternatives for Menopause (HALT) Study: background and study design. Maturitas. 2008. 61:181–193.
14. National Center for Complementary and Alternative Medicine, NIH Office of Dietary Supplement. Workshop on the safety of black cohosh in clinical studies-meeting summary. 2004. cited by 2011 Jul 1. Maryland: National Institutes of Health;Available from: http://nccam.nih.gov/news/events/blackcohosh/blackcohosh_mtngsumm.htm.
15. Osmers R, Kraft K. Phytotherapy in menopausal symptoms. Pharm Unserer Zeit. 2004. 33:384–391.
16. North American Menopause Society. Treatment of menopause-associated vasomotor symptoms: position statement of The North American Menopause Society. Menopause. 2004. 11:11–33.
17. Briese V, Stammwitz U, Friede M, Henneicke-von Zepelin HH. Black cohosh with or without St. John's wort for symptom-specific climacteric treatment--results of a large-scale, controlled, observational study. Maturitas. 2007. 57:405–414.
18. Avula B, Wang YH, Smillie TJ, Khan IA. Quantitative determination of triterpenoids and formononetin in rhizomes of black cohosh (Actaea racemosa) and dietary supplements by using UPLC-UV/ELS detection and identification by UPLC-MS. Planta Med. 2009. 75:381–386.
19. Iwanaga A, Kusano G, Warashina T, Miyase T. Hyaluronidase inhibitors from "Cimicifugae Rhizoma" (a mixture of the rhizomes of Cimicifuga dahurica and C. heracleifolia). J Nat Prod. 2010. 73:573–578.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download