Abstract
Background
We present here the oncological and functional outcomes of limb salvage with or without reconstruction for primary sarcomas in the pelvic bone.
Methods
Forty-four patients who underwent pelvic resection for primary sarcomas involving the pelvis were reviewed. The average follow-up period was 39 months (range, 0 to 146 months). Chondrosarcoma (n = 17) and osteosarcoma (n = 10) were the most common diagnoses. Various clinicopathologic factors were analyzed in relation to the oncological outcomes of overall survival and local recurrence. The Musculoskeletal Tumor Society functional scores and complications were compared according to the tumor location, pelvic continuity and the type of resection.
Results
The overall 5-year survival rate was 40%. Metastasis at the time of diagnosis, the surgical margin and the histologic grade were the independent prognostic factors for survival. The surgical margin was an independent prognostic factor for local recurrence. An ischiopubic location of the tumor, restoration of pelvic continuity and hip joint reconstruction with total hip replacement arthroplasty were related with higher functional scores. Complications occurred in 50% of the patients and the complications varied according to the tumor location with infection being the most common complication.
Conclusions
Achieving an adequate surgical margin is necessary for improving the oncological outcome of pelvic sarcomas. Restoration of the pelvic continuity and the hip joint improves the functional outcome. However, complications are common and so careful selection of the reconstruction method is needed.
Primary pelvic sarcomas are difficult to surgically treat because of the anatomic proximity of the pelvis to many neurovascular structures and the urinary and intestinal tracts. In addition, extensive resection of pelvic sarcomas often necessitates reconstruction to avoid severe functional disabilities from the impairment of the load-bearing axis.1,2) Therefore, decisions on the surgical treatment of pelvic sarcomas should be based on consideration in terms of both the resection and reconstruction, with the primary treatment goal being complete tumor resection and the secondary goal being preservation of the lower limb function.3) Limb-salvage surgery has currently become a possible option for many patients due to the advances in adjuvant treatments such as chemotherapy and radiation therapy. In addition, the developments in imaging techniques have allowed accurate visualization of the tumor extent and this helps to perform appropriate surgical resection.4,5)
Different reconstruction techniques that result in a variety of functional outcomes and complications are performed according to the anatomical location and the extent of resection of pelvic tumors. Since the adoption of the limb-salvage techniques for the treatment of pelvic sarcomas, arthrodesis or pseudoarthrosis techniques have been used for reconstruction.6-9) Allografts, recycled autografts,7) bone cement10) and tumor prostheses4,9) have recently been employed in proper combinations to obtain joint mobility. Likewise, various surgical techniques have been attempted to improve the patients' quality of life by the reducing the bed rest time and promoting early ambulation.
In this study, we assessed the oncological outcomes and prognostic factors of limb-salvage surgery and we analyzed the functional outcomes and complications according to the location and extent of resection in patients with primary pelvic sarcomas.
Forty-four patients who had been surgically treated for primary sarcomas of the pelvis between October 1991 and December 2006 were included in this study. There were 18 males and 26 females with a mean age of 39 years (range, 11 to 74 years). Five of them had undergone surgical treatment before being admitted to our institution for relapse. Metastasis was noted in 7 patients at the time of diagnosis. According to Enneking's classification,11) 1 patient had a stage IA tumor, 9 had stage IB tumors, 1 had a stage IIA tumor, 26 had stage IIB tumors and 7 had stage III tumors. The histological diagnosis was chondrosarcoma in 17 patients, osteosarcoma in 10, malignant fibrous histiocytoma in 6, Ewing sarcoma in 3, synovial sarcoma in 3, giant cell tumor in 2, liposarcoma in 1, malignant peripheral nerve sheath tumor in 1 and undifferentiated sarcoma in 1. The histological grade was low in 10 patients, high in 33 and unidentified in 1 patient. Soft tissue sarcoma involving bone structures was observed in 7 patients (3 patients with a synovial sarcoma, 2 patients with a malignant fibrous histiocytoma, 1 patient with a liposarcoma and 1 patient with a malignant peripheral nerve sheath tumor). The tumor size was measured as the maximum diameter on the MRI or pathological examination, and the average tumor size was 9.9 cm (range, 3.5 to 25.0 cm). The surgical margin was wide in 25 patients, marginal in 8 and intralesional in 11. Adjuvant therapies were carried out according to the histological diagnosis and the tumor stage. Preoperatively, chemotherapy was done in 12 patients and radiation therapy was done in 2 patients. Postoperatively, chemotherapy was done in 13 patients, radiation therapy was done in 9 and both were done in 3. The mean follow-up period was 39 months (range, 0 to 146 months) and the survivors were followed up for an average of 61 months (range, 12 to 146 months).
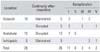
The locations of the tumors were classified into 3 types based on a modification of the system established by Enneking and Dunham.11) The iliosacral type was defined as a tumor involving the ilium or the sacrum and not the acetabulum, the actabular type was defined as the one invading the acetabulum and the ischiopubic type was defined as a tumor involving the pubis and not the acetabulum in this study. There were 20 tumors of the iliosacral type, 19 tumors of the acetabular type and 5 ischiopubic type tumors.
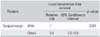
The reconstruction techniques were determined according to the anatomical location of the sarcoma and the presence or absence of continuity of the load-bearing axis extending from the sacrum to the femur (Table 1). Continuity was disrupted after tumor resection for 9 of the 19 iliosacral type tumors and for 16 of the 19 acetabular type tumors. Reconstruction was performed for 7 iliosacral type tumors and for 17 acetabular type tumors. Reconstruction was not carried out despite the absence of continuity after resection in 4 patients who had had a poor general condition preoperatively. All of the patients with ischiopubic type tumors underwent tumor resection without reconstruction. Of the patients with the acetabular type tumors, those with the absence of pelvic ring continuity after tumor resection were reconstructed with a composite reconstruction using low-heat treated recycled autografts and hip replacement arthroplasty with bone cement augmentation,12) or with a saddle prosthesis. Pelvic ring continuity was restored or maintained after reconstruction in 40 patients.
The overall survival rate and the local recurrence rate were calculated for the assessment of the oncological results. The associations with the histopathological factors were examined using the Kaplan-Meier method and the Cox proportional hazards model. The functional results were evaluated according to the Musculoskeletal Tumor Society (MSTS) scoring system13) which assigns 0 to 5 points for each of the following categories: pain, function, emotional acceptance, use of supports, walking ability and gait. Except for the 11 patients whose records were not available, 33 patients were included in the assessment of the functional results. The absence or presence of continuity of the pelvic ring was assessed on 2 occasions, once after resection and then after reconstruction, and the patients were subdivided according to the presence of continuity of the pelvic ring on each occasion. The MSTS scores of the patients grouped according to the presence of continuity of the pelvic ring, the kind of the inserted implants and the anatomical location of the tumor were compared. The associations between 5 major complications (local wound problems, implant failure, nerve injury, internal organ damage and vascular problems) and the anatomical location of the tumor and the continuity of the pelvic ring after surgery were evaluated.
Overall, 22 patients died until the last follow-up and the mean 5-year overall survival rate, which was calculated using the Kaplan-Meier method, was 40% (± 9%) for the 43 patients, with excluding 1 patient who was not available for follow-up. Of the 21 survivors, 18 had no evidence of disease and 3 were alive with disease. Twenty patients died due to the consequences of metastasis or local recurrence, 1 patient died due to intra operative hemorrhage and 1 patient died due to sepsis during chemotherapy. The mean interval from surgery to death was 20 months (range, 0 to 55 months). The age, the presence of metastasis at the time of diagnosis, the histological grade and the surgical margin were shown to have statistically significant relationships with the survival rate on the analysis using the Kaplan-Meier method (Table 2). The Cox multivariable analysis revealed that metastasis at the time of diagnosis, the histological grade and the surgical margin were the independent prognostic factors (Table 3).
Local recurrence was identified in 20 patients until the last follow-up. The mean 5-year local recurrence-free survival rate was 45% (± 9%) in the 42 patients, with excluding 1 patient who was unavailable for follow-up and excluding another 1 who had died of intraoperative hemorrhage. The Kaplan-Meier analysis showed that the surgical margin had a statistically significant correlation with local recurrence (Table 4) and it was identified as an independent prognostic factor on the Cox multivariable analysis (Table 5).
The mean MSTS score was higher in the patients with the presence of continuity of the pelvic ring after resection (75.4%) than in those with the absence of the continuity (65.8%). The score was also higher in the patients with continuity that was restored via reconstruction after resection than in those with the absence of continuity (Fig. 1). The mean functional score was higher in the patients with the ischiopubic type tumors (83.9%) than in those with the acetabular type tumors (64.8%) or those with the iliosacral type tumors (70.5%). Of the patients with the acetabular type tumors, the mean MSTS score was higher in the total hip replacement arthroplasty group (74.4%) than that in the saddle prosthesis group (63.3%).
Overall, 26 major complications occurred in 22 patients (50%). The incidence of complications was 40% in the patients with iliosacral type tumors (10 in 8 patients), 58% in the patients with acetabular type tumors (13 in 11 patients) and 60% in the patients with ischopubic type tumors (3 in 3 patients). The most common complications were related with wound healing such as an infection (9 cases) (Table 6). Implant failure and internal organ damage were the most common complications in the patients with acetabular type tumors and ischiopubic type tumors, respectively. The incidence of complications was higher in the patients in which resection resulted in the loss of pelvic continuity than those patients in which resection did not result in the loss of pelvic continuity; 60% (15 patients) with loss of continuity and 37% (7 patients) without loss of continuity.
The growing interest in cancer patients' quality of life has led to an increase of analyzing the functional outcomes of oncological treatments in many orthopedic oncology studies. Although much progress has been made in the diagnostic and treatment methods, sarcomas of the pelvis are more associated with a poor prognosis than are those of the long bones.11,14) Sarcomas of the pelvis are usually detected in the late stages and they are difficult to surgically treat in most cases. Massive tumor resection is unavoidable in such cases and a complete cure and functional recovery after resection are hard to achieve. As studies have shown that limb-salvage techniques and the amputation show no difference in terms of the survival rate of patients with malignant bone tumors, the limb-salvage techniques are now being frequently used even for cases of advanced tumors.14,15)
The possible prognostic factors for survival in patients with sarcomas of the pelvis include the tumor stage, the histological grade, the surgical margin and the tumor location.5,14-16) In this study, the histological grade, metastasis at the time of diagnosis (the tumor stage) and the surgical margin were the independent prognostic factors that were significantly related to survival. Older age was related to the low survival rate on the univariate analysis, but statistical significance was not found for that relationship on the multivariate analysis using the Cox proportional hazards model. The patients with soft tissue sarcomas had poorer results than those with bone sarcomas with 5 of the 7 patients dead, but the difference between the two was not statistically significant. These two factors might turn out to be significant prognostic factors for survival in future studies that will have a larger number of patients.
The local recurrence rate of this study was 45%, which is higher than that reported in most studies. We attributed this to the fact that a wide surgical margin could not be obtained in many cases of this study, with considering that the surgical margin was the factor most closely related to the local recurrence, as was also shown in other studies.1,5,15,17) According to O'Connor and Sim18) iliosacral type tumors had the highest local recurrence rate. Yet in this study, the local recurrence rate and the tumor location did not appear to be related to each other.
The pelvis functions as the axis that transmits the weight of the upper body to the legs and the pelvis contains the hip joint. If bone stock loss occurs due to wide resection of sarcomas, then the focus of the treatment should be set on restoring femorosacral continuity for weight bearing and obtaining mobility of the hip joint.1,8) In this study, satisfactory functional results could be achieved in those cases where pelvic ring continuity was re stored through reconstruction. The patients with ischiopubic type tumors had higher functional scores than those patients with iliosacral and acetabular type tumors. It is believe that the sacrum or ischium had a lesser role in weight bearing and accordingly their loss did not produce notable differences.
Restoration of hip joint mobility results in more satisfying functional outcomes than the pseudoarthrosis technique or amputation does, although it is associated with higher complication rates.1,5,8,17,19) We attempted to restore hip joint mobility in most of the cases with ac e tabular involvement and we found that total hip replacement arthroplasty resulted in higher functional scores than inserting a saddle prosthesis did. It is our understanding that when most of the proximal ilium is removed, a tumor prosthesis cannot be fixed and then inserting a saddle prosthesis, which is associated with inherent instability, would be the only remaining option. In contrast, when most of the proximal ilium is preserved or the bone stock is restored with a low-heat treated autograft, then total hip replacement arthroplasty would be applicable and encouraging postoperative outcomes in terms of stability and function would be attained.
The increased use of a tumor prosthesis in pelvic reconstruction combined with the prolonged survival of patients with sarcomas has led to a rise in the prevalence of a variety of prosthesis-related problems such as an infection and loosening of the prosthesis.20) Besides, as most high grade pelvic sarcomas carry a poor prognosis, there is controversy over the extent of surgery, and strict indications for surgery have been applied due to the high complication rates.2,14,20-22)
The complication rate in this study was 50%, which was similar to the 50 to 60% shown in other studies.2,14,20-22) The postoperative complication rates were related to the extent of surgery. Particularly, complications were prevalent in those cases where continuity of the pelvis was lost during resection. In our opinion, this was attributable to the extensive resection and reconstruction. The tumor location and the type of complication appeared to be related: nerve damage and bowel injury were common in the iliosacral type tumor, every kind of complication was observed after the use of a prosthesis in the acetabular type tumor and bladder injury was notable for the ischiopubic type tumor. Therefore, when an extensive operation is necessary, careful preoperative planning according to the tumor location would be helpful in reducing the complication rates.
In conclusion, achieving an adequate surgical mar gin is important for increasing the survival rate and reducing local recurrence in patients with primary pelvic sarcomas. Restoration of both the pelvic continuity and the hip joint results in better functional outcomes. However, complications are common and so careful selection of a reconstruction method is advised.
Figures and Tables
ACKNOWLEDGEMENTS
This work was supported by the Seoul National University Hospital Fund (04-2008-042-0).
References
1. Wirbel RJ, Schulte M, Mutschler WE. Surgical treatment of pelvic sarcomas: oncologic and functional outcome. Clin Orthop Relat Res. 2001. (390):190–205.
2. Zeifang F, Buchner M, Zahlten-Hinguranage A, Bernd L, Sabo D. Complications following operative treatment of primary malignant bone tumours in the pelvis. Eur J Surg Oncol. 2004. 30(8):893–899.

3. Simon MA, Aschliman MA, Thomas N, Mankin HJ. Limbsalvage treatment versus amputation for osteosarcoma of the distal end of the femur. J Bone Joint Surg Am. 1986. 68(9):1331–1337.

4. Natarajan MV, Bose JC, Mazhavan V, Rajagopal TS, Selvam K. The Saddle prosthesis in periacetabular tumours. Int Orthop. 2001. 25(2):107–109.

5. O'Connor MI. Malignant pelvic tumors: limb-sparing resection and reconstruction. Semin Surg Oncol. 1997. 13(1):49–54.
6. Guest CB, Bell RS, Davis A, et al. Allograft-implant composite reconstruction following periacetabular sarcoma resection. J Arthroplasty. 1990. 5:Suppl. S25–S34.

7. Harrington KD. The use of hemipelvic allografts or autoclaved grafts for reconstruction after wide resections of malignant tumors of the pelvis. J Bone Joint Surg Am. 1992. 74(3):331–341.

9. van der Lei B, Hoekstra HJ, Veth RP, Ham SJ, Oldhoff J, Schraffordt Koops H. The use of the saddle prosthesis for reconstruction of the hip joint after tumor resection of the pelvis. J Surg Oncol. 1992. 50(4):216–219.

10. Satcher Jr RL, O'Donnell RJ, Johnston JO. Reconstruction of the pelvis after resection of tumors about the acetabulum. Clin Orthop Relat Res. 2003. (409):209–217.
11. Enneking WF, Dunham WK. Resection and reconstruction for primary neoplasms involving the innominate bone. J Bone Joint Surg Am. 1978. 60(6):731–746.

12. Kim HS, Kim KJ, Han I, Oh JH, Lee SH. The use of pasteurized autologous grafts for periacetabular reconstruction. Clin Orthop Relat Res. 2007. (464):217–223.

13. Enneking WF, Dunham W, Gebhardt MC, Malawar M, Pritchard DJ. A system for the functional evaluation of reconstructive procedures after surgical treatment of tumors of the musculoskeletal system. Clin Orthop Relat Res. 1993. (286):241–246.

14. Campanacci M, Capanna R. Pelvic resections: the Rizzoli Institute experience. Orthop Clin North Am. 1991. 22(1):65–86.

15. Aboulafia AJ, Malawer MM. Surgical management of pelvic and extremity osteosarcoma. Cancer. 1993. 71:10 Suppl. 3358–3366.

16. Windhager R, Karner J, Kutschera HP, Polterauer P, Salzer-Kuntschik M, Kotz R. Limb salvage in periacetabular sarcomas: review of 21 consecutive cases. Clin Orthop Relat Res. 1996. (331):265–276.

17. Mankin HJ, Hornicek FJ, Temple HT, Gebhardt MC. Malignant tumors of the pelvis: an outcome study. Clin Orthop Relat Res. 2004. (425):212–217.
18. O'Connor MI, Sim FH. Salvage of the limb in the treatment of malignant pelvic tumors. J Bone Joint Surg Am. 1989. 71(4):481–494.
19. Ozaki T, Hoffmann C, Hillmann A, Gosheger G, Lindner N, Winkelmann W. Implantation of hemipelvic prosthesis after resection of sarcoma. Clin Orthop Relat Res. 2002. (396):197–205.

20. Senchenkov A, Moran SL, Petty PM, et al. Predictors of complications and outcomes of external hemipelvectomy wounds: account of 160 consecutive cases. Ann Surg Oncol. 2008. 15(1):355–363.





 PDF
PDF ePub
ePub Citation
Citation Print
Print







 XML Download
XML Download