Dear Editor:
Mycosis fungoides (MF) is a mature T-cell non-Hodgkin's lymphoma that presents with persistent and slowly progressive skin lesions of varying size and shape1. As the skin lesions of MF are variable, MF can be misdiagnosed as a benign dermatological condition12.
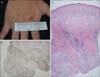
A 21-year-old man presented with a 4-month history of skin lesions on his eyelids. The skin lesions were diffuse erythematous to violet-colored patches on both upper eyelids with multiple 1~2-mm papules scattered on the patches. Both eyelids were edematous, making the patient look like he had swollen eyes (Fig. 1A). The patient did not complain of symptoms at the lesional area but did complain of feeling weak and lethargic over the last few months. We performed laboratory tests and skin biopsy of his right eyelid, and made a preliminary diagnosis of a heliotrope rash in dermatomyositis. We decided to withhold treatment until the diagnosis was confirmed. Laboratory tests including complete blood count, liver function test, fluorescent antinuclear antibody test (FANA), and creatinine kinase showed no abnormalities. Histopathological examination revealed epidermotropic and diffuse dermal infiltration of atypical lymphocytes with some eosinophils (Fig. 1B, C); the epidermotropic and dermal atypical lymphocytes were positive for CD3 and CD4, and some lymphocytes were positive for CD30 and negative for CD20 (Fig. 1D~F).
On the second visit, an erythematous papule 5 mm in diameter (Fig. 2A) had developed on the dorsum of the right hand, and there was no improvement in the skin lesions on the eyelids. Skin biopsy of the papule showed similar histopathological findings to those of the eyelids, i.e., epidermotropism and diffuse dermal infiltration of atypical lymphocytes with some eosinophils (Fig. 2B, C). Nested polymerase chain reaction for T-cell receptor-γ gene rearrangement showed monoclonality.
Bone marrow biopsy, abdominal pelvic computed tomography-multiplanar reformation, and chest computed tomography showed no internal organ involvement. With this histological and immunophenotypic information, the patient was diagnosed with MF and was treated with chemotherapy and total skin electron beam therapy.
MF is the most common type of cutaneous T-cell lymphoma and accounts for half of all primary cutaneous lymphomas1. Clinically, early in the course of MF, the skin lesions may be nonspecific and variable, making the diagnosis difficult even for dermatologists12. A new variant of MF was recently proposed, in which papular lesions are present in the absence of patches with the presence of histopathologic features of the classic patch/plaque stage2. Moreover, advanced MF can infiltrate or metastasiaze to the eye, causing blepharitis and cicatricial ectropion3.
Eyelid lesions must be differentiated from many conditions that can produce redness of the eyelids. Eczematous dermatological conditions such as contact dermatitis, atopic dermatitis, and seborrheic dermatitis commonly involve the eyelids45. Allergic contact dermatitis often affects the upper eyelids, while atopic dermatitis causes dermatitis in both the upper and lower eyelids. Seborrheic dermatitis is accompanied by lesions at other sites. Because the present patient had erythema and edema only on the upper eyelids without any subjective symptoms, we made an initial diagnosis of heliotrope rash in dermatomyositis. The diagnosis of MF should be made carefully on the basis of detailed history taking and physical examination if the skin lesion is persistent without changes in the shape or symptoms after conventional dermatological treatment. The present case illustrates the diversity of the cutaneous manifestations of MF, such as mimicking the heliotrope rash of dermatomyositis or eyelid eczema, and highlights the importance of skin biopsy for correct diagnosis and treatment.
Figures and Tables
Fig. 1
(A) Erythematous papules and patches with edematous swelling on the right eyelid. (B, C) Histological specimen showing diffuse dermal infiltration of atypical lymphocytes (H&E; B: ×40, C: ×400). Atypical lymphocytes infiltrating the dermis stained for (D) CD3 and weakly stained for (E) CD4 and (F) CD20 (D~F: ×40).

ACKNOWLEDGMENT
This research was supported by Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Education, Science and Technology (2012R1A1A1041389).
References
1. Yamashita T, Abbade LP, Marques ME, Marques SA. Mycosis fungoides and Sézary syndrome: clinical, histopathological and immunohistochemical review and update. An Bras Dermatol. 2012; 87:817–828.

2. Noe MH, Drake A, Link BK, Liu V. Papular mycosis fungoides: report of two patients, literature review, and conceptual re-appraisal. J Cutan Pathol. 2013; 40:714–719.

3. Leib ML, Lester H, Braunstein RE, Edelson RL. Ocular findings in cutaneous T-cell lymphoma. Ann Ophthalmol. 1991; 23:182–186.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download