Dear Editor:
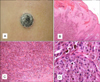
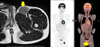
The lack of reliable pathological criteria for distinguishing between benign and malignant melanocytic lesions makes it very difficult for clinicians and pathologists to diagnosis melanoma. Here, we describe a rare case of a young patient affected by Spitzoid melanoma of the left leg with left superficial inguinal lymph node metastasis. A 13-year-old boy was referred to our hospital for a 19×9-mm cutaneous dome-shaped pigmented nodule on his left lower leg (Fig. 1A). The nodule appeared 3 months prior and was asymptomatic. No lymphadenopathy was found on physical examination. Under the suspicion of Spitz nevus, the tumor was excised with a 2-mm free margin. Histological analysis demonstrated that it was a symmetrical melanocytic tumor; it exhibited prominent pleomorphism and definitely showed changes of maturation (Fig. 1B~D). We detected hemorrhage crusts on the horny layer, but these were caused by the patient's scratching. There was no bleeding in his clinical course. Atypical epithelioid and spindle-shaped melanocytes with large hyperchromatic pleomorphic nuclei were observed. No ulceration was present. These findings were discordant with pigmented epithelioid melanocytoma1. His immunologic profile was consistent with a melanocytic tumor: S-100, Melan-A, and HMB-45 positivity, and CD34 negativity. The presence of diffuse HMB-45 positivity, even deeper in a nest, was considered unusual in a Spitz nevus. The extremely controversial nature of the lesion led to a diagnosis of atypical Spitz neoplasm of indeterminate biologic potential or Spitzoid-type minimal deviation melanoma. After receiving informed consent from the patient's parents, we performed careful observation, considering the possibility of malignant tumor. He had a huge palpable inguinal lymph node on physical examination 4 months postoperatively. Magnetic resonance imaging and positron emission tomography scans showed a large metastatic superficial inguinal lymph node (Fig. 2). Under a diagnosis of Spitzoid melanoma with subsequent lymph node metastasis, we performed wide local excision (2-cm margin including the periosteum) of the lower leg and resurfaced the defect with a local flap procedure. Left inguinal lymph nodes including the superficial and deep node groups were completely dissected. Three of the nine harvested lymph nodes including the large lymph node exhibited metastasis. Atypical melanocytes similar to those in the leg lesion were found within the lymph node parenchyma. The patient was treated with adjuvant dacarbazine, nimustine, and vincristine chemotherapy 5 times over 6 months. At a recent follow-up 2 years later, he did not have any evidence of recurrence or metastasis. The 5-year survival rate of children between 11 and 17 years old with metastatic Spitzoid melanoma is 49%2. Recent studies suggest the prognosis of children with Spitzoid melanoma is better than that in adults even local metastases or positive sentinel lymph nodes are present3,4,5. However, some cases of incomplete excision of Spitzoid melanoma leading to systemic metastasis and death have been reported5. Therefore, in cases in which the diagnosis is uncertain despite further evaluations, it is necessary perform careful observation to prevent recurrence and metastasis as early as possible.
Figures and Tables
Fig. 1
(A) A 10-mm dome-shaped pigmented nodule on the left lower leg. (B) Histopathology of the skin lesion; Breslow's thickness clearly exceeded 4 mm. No ulceration was present (H&E, ×10). (C) Abundant irregular nests of varying size and shape, and asymmetrical proliferation of enlarged atypical epithelioid and spindle-shaped melanocytes in the deep dermis (H&E, ×20). (D) Atypical epithelioid and spindle-shaped melanocytes with large hyperchromatic pleomorphic nuclei were observed (H&E, ×40).
References
1. Zembowicz A, Carney JA, Mihm MC. Pigmented epithelioid melanocytoma: a low-grade melanocytic tumor with metastatic potential indistinguishable from animal-type melanoma and epithelioid blue nevus. Am J Surg Pathol. 2004; 28:31–40.
2. Pol-Rodriquez M, Lee S, Silvers DN, Celebi JT. Influence of age on survival in childhood spitzoid melanomas. Cancer. 2007; 109:1579–1583.

3. Busam KJ, Murali R, Pulitzer M, McCarthy SW, Thompson JF, Shaw HM, et al. Atypical spitzoid melanocytic tumors with positive sentinel lymph nodes in children and teenagers, and comparison with histologically unambiguous and lethal melanomas. Am J Surg Pathol. 2009; 33:1386–1395.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download