Abstract
Objective
The aim of this study was to measure tumor necrosis factor-α (TNF-α) levels around miniscrews used for anchorage during a 3-month period of canine distalization.
Methods
Sixteen patients (8 boys, 8 girls; mean age, 16.6 ± 2.4 years) whose upper first premolars were extracted for orthodontic treatment were included in this study. Miniscrews were used as an anchorage unit in canine distalization. Thirty-two (32) miniscrew implants were placed bilaterally in the alveolar bone between the maxillary second premolars and first molars. The treatment, miniscrew, and control groups comprised upper canines, miniscrew implants, and upper first premolars, respectively. Peri-miniscrew implant crevicular fluid and gingival crevicular fluid were obtained before applying force and at 1, 24, and 48 hours, and at 7 and 21 days, and 3 months after applying force.
The appearance of osteoclasts and bone resorption are essential factors that initiate tooth movement during orthodontic treatment. At the beginning of orthodontic tooth movement, the mechanical stimulus causes an acute inflammatory reaction within the periodontal tissues. This inflammatory reaction may trigger biologic processes that result in bone resorption.1,2 Various cytokines and hormones regulate this process.3
Proinflammatory cytokines play important roles in bone resorption as in any root resorption process.4 Tumor necrosis factor-α (TNF-α) is a proinflammatory cytokine produced by activated monocytes, macrophages, and osteoblasts.5 In addition to bone resorption, TNF-α stimulates fibroblasts to produce collagenase.6 Lowney et al.7 attributed the increase in TNF-α to orthodontic force.
Cytokines such as TNF-α have an important role in regulating and amplifying the inflammatory response in periodontal and peri-implant tissues.8-10
Implant anchorage was recently established as an effective treatment for a wide variety of adult malocclusions.11 Dental implants, miniplates, and titanium screws have been used for implant anchorage in orthodontic treatment.12,13 These materials can provide absolute anchorage for tooth movement even without the patient's cooperation. In particular, miniscrews are most commonly used for skeletal anchorage.14,15
Following osseointegration and loading, failing implants develop peri-implant inflammation known as peri-implantitis, which is similar to periodontitis.16 Clinical signs of peri-implantitis are soft tissue inflammation, bleeding on probing, suppuration, pain, increased probing depth, and radiographic evidence of bone loss.17 The increase in TNF-α levels in peri-implant crevicular fluid (PICF) is reported to cause peri-implantitis.10 To our knowledge, there are no published studies in which TNF-α levels around miniscrew implants were measured.
Therefore, the goal of this study was to measure TNF-α levels around miniscrews during a 3-month period of canine distalization and to compare the results with the cytokine levels around healthy teeth.
Sixteen patients (8 boys, 8 girls; mean age, 16.6 ± 2.4 years) who required extraction of their upper first premolars for orthodontic treatment were included in this study from the Department of Orthodontics, School of Dentistry, Dicle University. The inclusion criteria were a healthy systemic condition, no use of anti-inflammatory drugs in the 6 months preceding the beginning of the study, and no radiographic evidence of periodontal bone loss after a full-mouth radiographic periapical examination. The periodontal health of the patients was also evaluated using the plaque index (PI), gingival index (GI), pocket depth (PD), and bleeding on probing (BOP). Informed consent was obtained from all of the patients and the parents of the patients under 18 years of age.
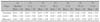
Thirty two miniscrew implants with a gingival index score of 0 (Normal gingiva) or 1 (mild inflammation, slight change in color, slight edema, no BOP) around them were included in this study. Gingival index was measured as recommended by Loe and Silness.18 The GI measurements for all groups are shown in Table 1.
The maxillary first premolars were extracted from each participant and a completely fixed, preadjusted, edgewise appliance with 0.018-inch slots was attached, and a 0.014-inch nickel-titanium (NiTi) archwire was placed for initial leveling. After the maxillary anterior teeth were aligned, a 0.016 × 0.022-inch stainless steel archwire with molar toe-ins and tip-back bends was placed, and the second maxillary premolars and first molars were ligated together before beginning distal movement of the canines.
Thirty two miniscrew implants (12 mm long, 1.6 mm in diameter, Anchor Plus, Buk-gu, Gwangju, Korea) were placed bilaterally into the inter-radicular bone between the maxillary second premolars and the first molars of all 16 patients under local anesthesia. The miniscrews were placed in the attached gingiva near the mucogingival junction. To reduce the root contact, miniscrew-implants were placed in an oblique direction buccolingually, 30° to 40° to the long axis of the teeth in the maxillary posterior area, as described in previous reports.19,20 Two weeks after placement, distal movement of the maxillary canines was begun with a 150-g force delivered by a NiTi closed-coil spring (7-mm Sentalloy closed coil spring, GAC International, Bohemia, NY, USA) between the miniscrew implants and canines.
The treatment, miniscrew, and control groups consisted of upper canines, miniscrew implants, and upper second premolars, respectively.
Gingival crevicular fluid (GCF) samples were obtained from the maxillary canines (treatment) and the maxillary second premolar teeth (controls) with paper strips (Periopaper®, Pro Flow, Amityville, NY, USA) using the method described by Rüdin et al.21 Peri-miniscrew implant crevicular fluid (PMICF) samples were also collected with paper strips over 3 months according to the following schedule:
GCF and PMICF samples were collected in the early hours of the day. Sample sites were isolated with cotton rolls, plaque was removed, and the tooth surfaces were air-dried. GCF and PMICF were collected as described in Sari and Uçar.22 PMICF samples were collected from the mesiobuccal aspects of the miniscrew implants. Two strips of filter paper were used to take PMICF samples from miniscrew implants, and the samples were placed in Eppendorf tubes. GCF samples were also obtained from distobuccal sites of the maxillary canines. Two filter papers used to collect GCF were placed in additional Eppendorf tubes. Similarly, two filter papers were used for the control teeth. The first strip was inserted into the base of the pocket for 30 seconds. After a 1-minute interval, a second strip was inserted into the base of the pocket for 30 seconds and after waiting 30 seconds, an apparatus (Periotron 8000, Ora Flow Inc., Plainview, NY) was used to determine the GCF and PMICF volume. Paper strips were stored in sterile tubes at -20℃ until the day of the experiment. Saliva- and blood-contaminated samples were excluded from the study. GCF and PMICF samples were obtained before all other clinical examinations were performed to prevent an increase in fluid volume. Before examining the GCF and PMICF, 1000 µL sterile NaCl (9 mg/mL) was added to the paper strips, and the GCF and PMICF were centrifuged at 3000 g at 5℃ for 20 minutes.23 An immunoassay kit was used to measure TNF-α concentrations (Immulite, Diagnostic Products, Los Angeles, CA, USA, Fig 1). A TNF-α free nonhuman buffer matrix was used to manually dilute the patient samples.
The amounts of TNF-α in each sample were compared with standard curves for TNF-α, which showed a direct relationship between optical density and cytokine concentration.
Normality of the data was assessed using the Kolmogorov-Smirnov test, and statistical homogeneity was checked by the Levene test. A paired sample t-test for within-group changes was used. A one-way ANOVA was applied for the between-groups comparison, while Dunnett's test and Tukey's HSD test were used for the between-groups multiple comparisons. All data were analyzed using SPSS version 15.0 (SPSS Inc., Chicago, IL, USA). A p value of 0.05 was considered statistically significant.
The Kolmogorov-Smirnov test showed that the data was normally distributed (p = 0.094 - 0.931), and Levene's test showed homogeneity of variances (p = 0.123 - 0.915).
The changes in the concentration of TNF-α during the observation period are shown in Fig 2. The TNF-α level increased beginning from the 1st hour in the treatment group and continued until the 7th day. The increase in TNF-α level was significant only at 24 hours (p < 0.01; Table 2). An increase beginning from the 1st hour and proceeding until the 7th day were observed in the miniscrew group, but the increase was not significant (p = 0.417 - 0.990). No significant changes were observed in the control group (p = 0.117 - 0.997). No significant differences were detected in the between-group evaluation (p = 0.137 - 0.999).
Anchorage control is one of the most important aspects of orthodontic treatment. Microscrew implants are frequently used for anchorage control. There are many advantages to the use of microscrews for anchorage, such as the lack of a requirement for patient compliance, ease of placement and removal, small size, and low cost.24 Miniscrews can provide absolute anchorage for guiding tooth movement. Despite their small diameter and short length, miniscrews can provide stable anchorage for various tooth movements, including intrusion, retraction, and protraction.14,15
Chemical analysis of GCF is useful for investigating changes at a single site during a specific period and the response of dental and paradental tissues to orthodontic tooth movement. Because this is a noninvasive method and repetitive sampling from the same side is possible, it is used especially for human studies.21,25
As Serra et al.26 reported that age and sex have no effect on enzymatic activity, these factors were not considered and the samples were pooled in this study.
Cytokines, produced by the cells of the immune system in response to stimulation, mediate acute inflammation and are present inperiodontal diseases, bone destruction, and bone response to orthodontic treatment.25 Cytokines are classified as proinflammatory and anti-inflammatory. Previous studies reported that proinflammatory cytokines, especially TNF-α, play an important role in the formation and distrubution of inflammation in periodontal and peri-implant structures.8,9 Thus, we aimed to measure the levels of these proinflammatory cytokines around miniscrews, which are frequently used in orthodontics and to compare the results with the cytokine levels around healthy teeth.
TNF-α is a critical cytokine in the inflammatory response to infection.27 Accordingly, any genetic variability in the production of TNF-α after an infectious stimulus could significantly affect the degree of the inflammatory response and the clinical outcome.28 To our knowledge, there are no reports of measurements of TNF-α levels around miniscrews used as an anchorage unit in orthodontics. TNF-α levels around teeth during orthodontic treatment, however, were measured in a previous study.4 Başaran et al.4 reported increases in TNF-α levels on days 7 and 21 during canine distalization. In our study, TNF-α levels around the canines began to increase from the first hours and the increase was statistically significant at 24 hours, which is consistent with the results of Başaran et al.4
In the present study, TNF-α levels around miniscrews began to increase in the initial hours, but the increase was not statistically significant. In addition, there were no differences between miniscrew implants and teeth in the between-group comparision. Machtei et al.29 compared TNF-α levels between dental implants and teeth and reported similar results. Further, TNF-α levels around miniscrew implants were higher than those around the teeth during the baseline period in our study, although the increase was not significant. This finding is consistent with the results reported by Nowzari et al.30
In the present study, cytokine levels around the miniscrews and canines increased in the initial periods. We attribute these increases to an acute response against the forces applied at the beginning of distalization. Cytokine levels decreased towards baseline levels in both groups, however, beginning on day 21. This decrease might be attributed to the adaptation of periodontal tissues to the orthodontic force, and feedback mechanisms might prevent an excessive increase in the inflammation mediators, thereby preventing harmful consequences.31
In the absence of good oral hygiene, oral microbiota may cause chronic inflammation of the peri-implant tissues. Like periodontitis, peri-implantitis can lead to implant loss.32 Schierano et al.10 found that TNF-α levels around peri-implant tissues were significantly increased by poor oral hygiene and decreased by good oral hygiene. In the present study, the patients' good oral hygiene may have prevented a significant increase in TNF-α levels around the miniscrew implants.
In conclusion, TNF-α levels around miniscrews used for anchorage in canine distalization increased in the initial period by the application of force to the miniscrew. The TNF-α levels around the miniscrews returned to baseline levels, however, after 7 days if physiologic forces were applied and proper oral hygiene was maintained.
Figures and Tables
Fig. 2
Changes in the concentration of TNF-α during the observation period. T1, Before distalization (baseline); T2, T3, T4, T5, T6 and T7, 1 hour, 1 day, 2 days, 1 week, 3 weeks and 3 monts after activation, respectively.

References
1. Proffit WR, Fields HW, Sarver DM. Contemporary orthodontics. 2007. 4th ed. St Louis, Mo: Mosby;348–349.
2. Sari E, Olmez H, Gürton AU. Comparison of some effects of acetylsalicylic acid and rofecoxib during orthodontic tooth movement. Am J Orthod Dentofacial Orthop. 2004. 125:310–315.

4. Başaran G, Ozer T, Kaya FA, Kaplan A, Hamamci O. Interleukine-1β and tumor necrosis factor-α levels in the human gingival sulcus during orthodontic treatment. Angle Orthod. 2006. 76:830–836.
5. Aggarwal BB, Samanta A, Feldman M. Oppenheim JJ, Feldman M, editors. TNF receptors. Cytokine. 2003. Vol 2. San Diego, Calif: Academic Press;1619–1632.
6. Bertolini DR, Nedwin GE, Bringman TS, Smith DD, Mundy GR. Stimulation of bone resorption and inhibition of bone formation in vitro by human tumor necrosis factors. Nature. 1986. 319:516–518.

7. Lowney JJ, Norton LA, Shafer DM, Rossomando EF. Orthodontic forces increase tumor necrosis factor α in the human gingival sulcus. Am J Orthod Dentofacial Orthop. 1995. 108:519–524.

8. Delima AJ, Oates T, Assuma R, Schwartz Z, Cochran D, Amar S, et al. Soluble antagonists to interleukin-1 (IL-1) and tumor necrosis factor (TNF) inhibits loss of tissue attachment in experimental periodontitis. J Clin Periodontol. 2001. 28:233–240.

9. Graves DT, Cochran D. The contribution of interleukin-1 and tumor necrosis factor to periodontal tissue destruction. J Periodontol. 2003. 74:391–401.

10. Schierano G, Pejrone G, Brusco P, Trombetta A, Martinasso G, Preti G, et al. TNF-α TGF-β2 and IL-1β levels in gingival and peri-implant crevicular fluid before and after de novo plaque accumulation. J Clin Periodontol. 2008. 35:532–538.

11. Roberts WE, Engen DW, Schneider PM, Hohlt WF. Implant-anchored orthodontics for partially edentulous malocclusions in children and adults. Am J Orthod Dentofacial Orthop. 2004. 126:302–304.

12. Fukunaga T, Kuroda S, Kurosaka H, Takano-Yamamoto T. Skeletal anchorage for orthodontic correction of maxillary protrusion with adult periodontitis. Angle Orthod. 2006. 76:148–155.
13. Kuroda S, Sugawara Y, Deguchi T, Kyung HM, Takano-Yamamoto T. Clinical use of miniscrew implants as orthodontic anchorage: success rates and postoperative discomfort. Am J Orthod Dentofacial Orthop. 2007. 131:9–15.

14. Park HS, Kwon TG, Sung JH. Nonextraction treatment with microscrew implants. Angle Orthod. 2004. 74:539–549.
15. Kuroda S, Sugawara Y, Tamamura N, Takano-Yamamoto T. Anterior open bite with temporomandibular disorder treated with titanium screw anchorage: evaluation of morphological and functional improvement. Am J Orthod Dentofacial Orthop. 2007. 131:550–560.

17. Lekholm U, Adell R, Lindhe J, Brånemark PI, Eriksson B, Rockler B, et al. Marginal tissue reactions at osseointegrated titanium fixtures. (II) A cross-sectional retrospective study. Int J Oral Maxillofac Surg. 1986. 15:53–61.
18. Loe H, Silness J. Periodontal disease in pregnancy. I. Prevalence and severity. Acta Odontol Scand. 1963. 21:533–551.

19. Park HS, Bae SM, Kyung HM, Sung JH. Micro-implant anchorage for treatment of skeletal Class I bialveolar protrusion. J Clin Orthod. 2001. 35:417–422.
20. Park HS, Kyung HM, Sung JH. A simple method of molar uprighting with micro-implant anchorage. J Clin Orthod. 2002. 36:592–596.
21. Rüdin HJ, Overdiek HF, Rateitschak KH. Correlation between sulcus fluid rate and clinical and histological inflammation of the marginal gingiva. Helv Odontol Acta. 1970. 14:21–26.
22. Sari E, Uçar C. Interleukin 1β levels around microscrew implants during orthodontic tooth movement. Angle Orthod. 2007. 77:881–884.
23. Tzannetou S, Efstratiadis S, Nicolay O, Grbic J, Lamster I. Interleukin 1β and β-glucuronidase in gingival crevicular fluid from molars during rapid palatal expansion. Am J Orthod Dentofacial Orthop. 1999. 115:686–696.

24. Deguchi T, Takano-Yamamoto T, Kanomi R, Hartsfield JK Jr, Roberts WE, Garetto LP. The use of small titanium screws for orthodontic anchorage. J Dent Res. 2003. 82:377–381.

25. Tuncer BB, Ozmeriç N, Tuncer C, Teoman I, Cakilci B, Yücel A, et al. Levels of interleukin-8 during tooth movement. Angle Orthod. 2005. 75:631–636.
26. Serra E, Perinetti G, D'Attilio M, Cordella C, Paolantonio M, Festa F, et al. Lactate dehydrogenase activity in gingival crevicular fluid during orthodontic treatment. Am J Orthod Dentofacial Orthop. 2003. 124:206–211.

27. Beutler B, Grau GE. Tumor necrosis factor in the pathogenesis of infectious diseases. Crit Care Med. 1993. 21:10 Suppl. S423–S435.

28. Holmes CL, Russell JA, Walley KR. Genetic polymorphisms in sepsis and septic shock: role in prognosis and potential for therapy. Chest. 2003. 124:1103–1115.
29. Machtei EE, Oved-Peleg E, Peled M. Comparison of clinical, radiographic and immunological parameters of teeth and different dental implant platforms. Clin Oral Implants Res. 2006. 17:658–665.

30. Nowzari H, Botero JE, DeGiacomo M, Villacres MC, Rich SK. Microbiology and cytokine levels around healthy dental implants and teeth. Clin Implant Dent Relat Res. 2008. 10:166–173.





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download