Abstract
Backgrounds/Aims
Fatigue is common in chronic hepatitis and end-stage liver disease. However, little is known about fatigue after liver transplantation (LT). We therefore evaluated the prevalence, severity, and related factors of fatigue after LT.
Methods
We retrospectively reviewed adult recipients who responded to our survey at outpatient clinics between April and May 2013. Fatigue and its severity were assessed using a questionnaire with the Fatigue Severity Scale (FSS). We defined fatigue as FSS of 4.0 or more and severe fatigue as FSS of 5.1 or more. The related factors including hepatocellular carcinoma and complications were analyzed.
Results
A total of 93 patients were included in this study. The mean age was 54.9 (19-76) years and two-thirds were men (67.7%). Living donor LT was 77.4%. Hepatitis B related liver disease was the main underlying disease (77.4%), with hepatocellular carcinoma accompanied in 33.3%. The mean follow-up period was 66.8±43.2 (2-171) months. The mean FFS was 2.83±1.48 (1.0-6.7) overall and 5.10±0.82 (4.0-6.7) in the fatigue group. Of the 93 adult patients, fatigue was presented in 20 patients (21.5%). Among these, 9 patients (45.0%) showed severe fatigue. Even though post-LT complications tended to be greater in the fatigue group (50.0% vs. 30.1% in the non-fatigue group, p=0.098), there were no significant related factors of fatigue after LT, including hepatocellular carcinoma and major complication.
Fatigue is considered to be common in chronic liver disease including liver cirrhosis.12 Although several studies showed that liver transplantation (LT) was associated with an improvement in fatigue in recipients,34 fatigue remains a troublesome and persistent symptom after LT.25678 Fatigued recipients report lower levels of health-related daily functioning and health-related quality of life compared to non-fatigued recipients.8
The pathogenesis of fatigue in chronic diseases and LT recipients is not clear and is usually multifactorial.2 According to previous studies, age, gender, level of physical activity, and cardiorespiratory fitness were related factors of fatigue after LT.8910 Poor sleep quality, anxiety, and depression were also hypothesized to be related factors of fatigue in chronic patients and LT recipients.1011 Kalaitzakis et al.2 reported that psychological distress, severity of cirrhosis, and low levels of cortisol determine general fatigue, whereas anemia and impaired renal function also contribute to physical fatigue.
Little is known about the prevalence and related factors of fatigue after LT, and to our knowledge, there are no reports about fatigue after LT in Korea. We therefore designed the present study to evaluate the prevalence, severity, and related factors of fatigue after LT.
We retrospectively reviewed adult recipients who responded to our survey at outpatient clinics between April and May 2013. In the present study, we excluded patients with any of the followings: <18 year of age at the time of survey, <1 month between survey time and LT, and ongoing treatment at the time of survey because of complications related to LT.
The presence and severity of fatigue after LT were assessed using the questionnaire with the Fatigue Severity Scale (FSS) which was developed by Dr. Krupp.12 The FSS contains 9 items which were developed to assess disabling fatigue. Patients were asked to read each statement of the questionnaire and choose the number from 1 to 7 that best described their level of agreement with each statement: 1 indicates strongly disagree (no symptom of fatigue) and 7 indicates strongly agree (most disabling fatigue).121314 FSS was the mean value from 9 items. In the present study, we defined fatigue as FSS of 4.0 or more (≥1 standard deviations (SD) of mean value in general population), and severe fatigue as FSS of 5.1 or more (≥2 SD of mean value in general population).10
The fatigue group (FSS ≥4.0) was compared with the non-fatigue group, and the related factors (including age, gender, primary liver disease, hepatocellular carcinoma, living or deceased donor, model for end-stage liver disease score, the time interval between survey time and LT, and post-LT complications) of fatigue after LT were analyzed.
Statistical analyses were performed using SPSS version 21.0. (IBM Co., Armonk, NY). All categorical data were expressed as a number or frequency with percentage in parentheses and all continuous data were given as mean±SD. Continuous variables were compared with Student's t-test, and categorical variables were compared using the Pearson's chi-square test or the Fisher's exact test if suspected cell frequency was less than 5, or using linear by linear association if a variable had more than two categories. All p-values were two-sided, and p<0.05 was considered statistically significant.
This study was approved by the institutional review board at our hospital. Informed consent was waived by the institutional review board.
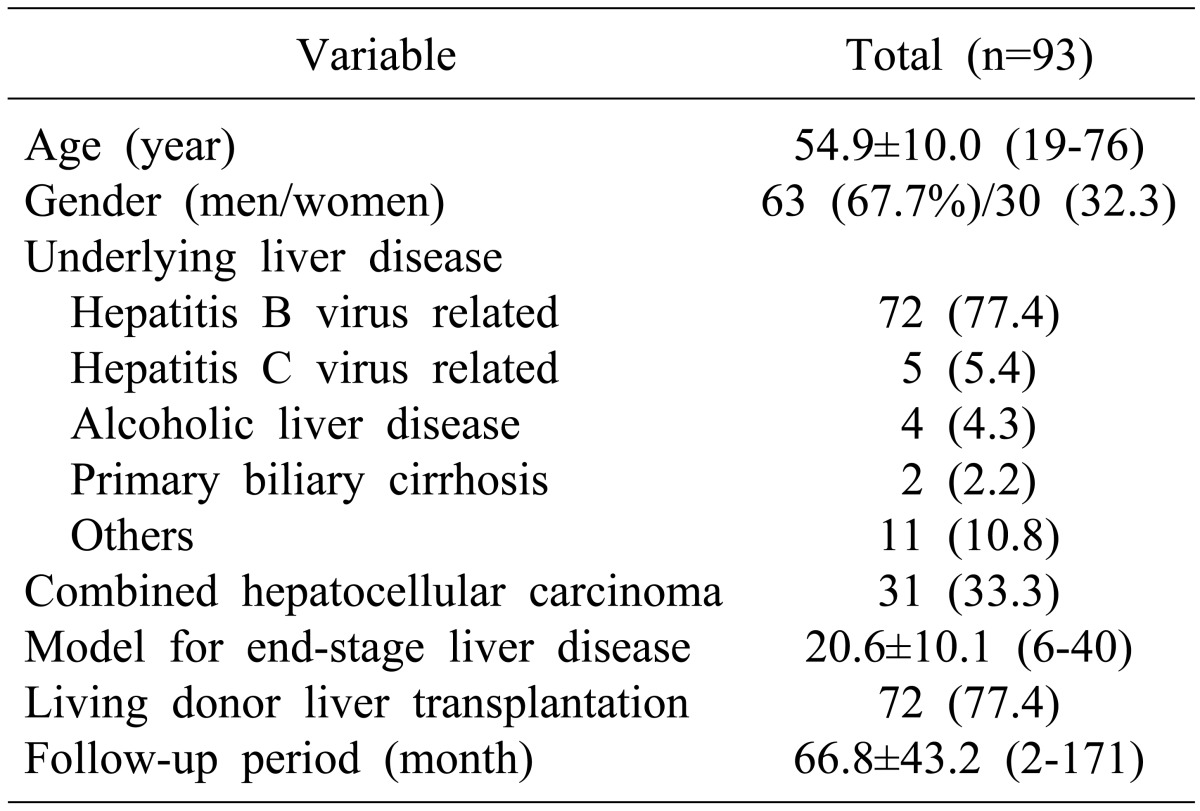
The survey was performed in 93 patients. The baseline characteristics of these patients are presented in Table 1. The overall mean age was 54.9±10.0 (range, 19-76) years and two-thirds were men (67.7%). Hepatitis B related liver disease was the main etiology of LT (77.4%), and hepatocellular carcinoma accompanied in 33.3%. Pre-LT model for end-stage liver disease score was mean 20.6±10.1 (range, 6-46), and living donor LT was 77.4%. The mean follow-up period was 66.8±43.2 (range, 2-171) months.
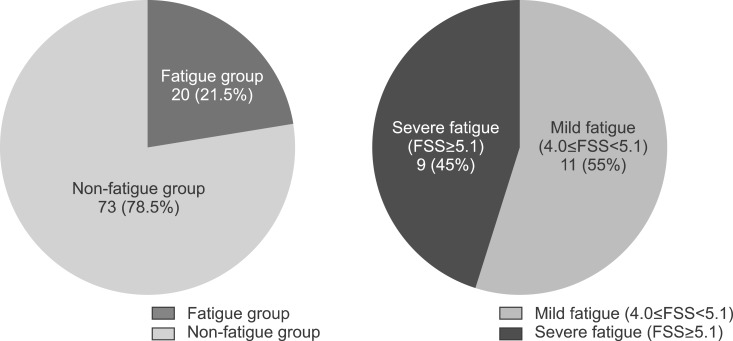
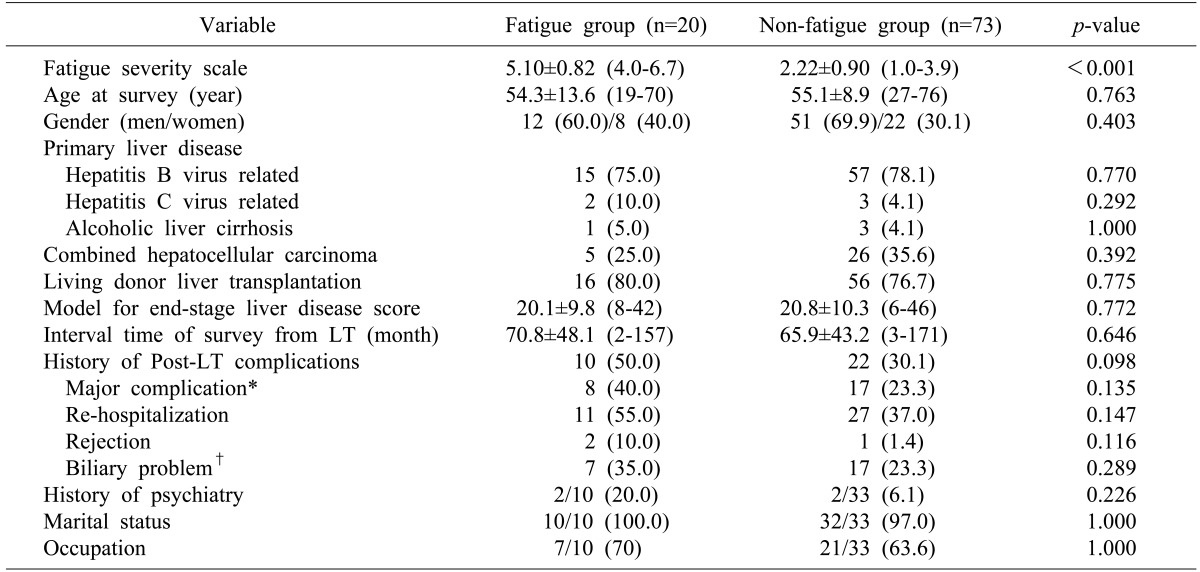
The prevalence and severity of fatigue after LT are summarized in Fig. 1. The overall mean FSS was 2.83±1.48 (range, 1.0-6.7). Of the 93 adult patients, the fatigue after LT was presented in 20 patients (21.5%). Among the fatigued patients, 9 patients (45.0%) showed severe fatigue. The mean value of FSS was 5.10±0.82 (range, 4.0-6.7) in the fatigue group, and it was 2.22±0.90 (range, 1.0-3.9) in the non-fatigue group (p<0.001) (Table 2).
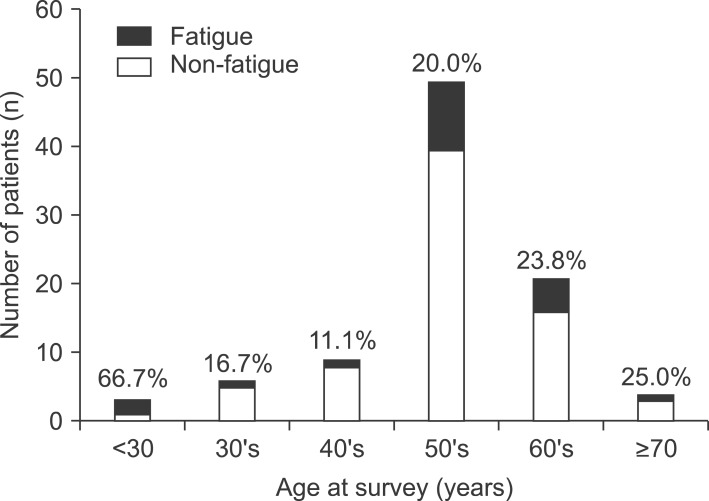
The distribution of patients and prevalence of fatigue after LT according to age at the time of survey are shown in Fig. 2. The prevalence was highest in the group less than 30 years of age (66.7%), and it was decreasing to 16.7% in patients in their 30s and then to 11.1% in patients in their 40s. It gradually increased again from 20.0% in patients in their 50s to 25.0% in patients in their 70s. However, these differences in prevalence of fatigue according to age were not significant (p=0.661).
Various clinical parameters (including age, gender, underlying liver disease, hepatocellular carcinoma, model for end-stage liver disease score, living or deceased donor, time interval between survey and LT, post-LT complications, history of psychiatry, marital status, and occupation) were compared between the fatigue group and the non-fatigue group (Table 2). Even though post-LT complications tended to be greater in the fatigue group (50.0% vs. 30.1% in the non-fatigue group, p=0.098), there were no significant related factors of fatigue after LT, including hepatocellular carcinoma and major complications (Table 2).
Recently, outcomes after LT continue to improve and most centers report 5-year survival exceeding 85%.4 According to the report by one of the major transplant centers in Korea, the 1-, 2-, and 5-year patient survival rates were 96, 95, and 94% in living donor LT, respectively, and graft survival rates were 99, 99, and 98% respectively.15 The quality of life after LT has become a major concern. In spite of improved quality of life after LT, fatigue remains one of the most distressing symptoms after LT, and fatigued recipients report poorer quality of life compared to non-fatigued recipients.12345678 In a previous longitudinal study of liver transplant recipients, 20% reported being fatigued, 40% reported being severely fatigued, and the remaining 40% reported no fatigue. These percentages did not decrease during the 2-year follow-up, suggesting that fatigue is a chronic problem following LT.10 However, there are only a few studies on fatigue after LT. Furthermore, previous studies about it have been performed mainly in patients with hepatitis C virus related liver disease, primary biliary cirrhosis, or primary sclerosing cholangitis in Western countries.24781016
To the best our knowledge, this is the first study about fatigue after LT in Korea. In the present study, the prevalence of fatigue after LT was 21.5%, and that of severe fatigue was 9.7%. These were relatively lower than the results of a previous study (60% and 40%, respectively).10 The reason for this may be due to the following characteristics in our cohort: 1) hepatitis B virus related liver cirrhosis as dominant baseline (77.4%) rather than hepatitis C virus related liver cirrhosis or primary biliary cirrhosis; 2) consented patients who underwent the survey at outpatient clinics; 3) elective living donor LT dominant (77.4%). However, the severity of fatigue was considerable. The mean FSS of overall fatigue group was 5.10±0.82, exceeding the criteria of severe fatigue. Among the fatigue group, 45% of patients suffered from severe fatigue (Fig. 1).
Contrary to our expectations we found no significant related factors of fatigue after LT, including hepatocellular carcinoma and major complication. Regarding the related factors of fatigue after LT, several physical and psychological factors have been reported in previous studies, including pre-LT disease severity, level of physical activity, cardiorespiratory fitness, poor sleep quality, anxiety, and depression, etc.28910111718 Nickel et al.18 and van Ginneken et al.10 indicated that sleep quality, anxiety, and depression are associated with fatigue in recipients. Van den Berg-Emons et al. reported that recipients experience physical fatigue and reduced activity rather than mental fatigue and reduced motivation. They suggested that these findings imply that rehabilitation programs, focusing on improving activity patterns and physical fitness, may reduce complaints of fatigue after LT.819 However, there were still conflicts about factors of fatigue after LT. In addition, no large scale prospective study has been performed in this field.
Limitations of this study should be acknowledged. This study was performed at outpatient clinics and comprised a relatively small number of patients who consented to the survey. Therefore, there is the potential for a selection bias and response bias due to excluding patients not feeling well enough to take part in the study. In addition, selecting items to access fatigue and related factors, we focused on aspects of health status or physical condition and overlooked potentially important predictor variables like psychological condition (especially, anxiety and depression), self-esteem, and perceived social support. Therefore, we may not extend or apply this result to the entire recipient population. Nevertheless, we believe that the present study can serve as the basis for further studies about the factors affecting fatigue and quality of life in LT recipients.
In conclusion, fatigue is present in a considerable number of patients after LT (21.5%), and almost half of fatigued patients suffer from severe fatigue (45.0%). The related factors of fatigue after LT are still vague and complicated, and further efforts are needed to lessen fatigue and improve quality of life for LT recipients.
References
1. Hay JE. Liver transplantation for primary biliary cirrhosis and primary sclerosing cholangitis: does medical treatment alter timing and selection? Liver Transpl Surg. 1998; 4(5 Suppl 1):S9–S17. PMID: 9742489.
2. Kalaitzakis E, Josefsson A, Castedal M, Henfridsson P, Bengtsson M, Hugosson I, et al. Factors related to fatigue in patients with cirrhosis before and after liver transplantation. Clin Gastroenterol Hepatol. 2012; 10:174–181. PMID: 21839709.

3. Gross CR, Malinchoc M, Kim WR, Evans RW, Wiesner RH, Petz JL, et al. Quality of life before and after liver transplantation for cholestatic liver disease. Hepatology. 1999; 29:356–364. PMID: 9918910.

4. Carbone M, Bufton S, Monaco A, Griffiths L, Jones DE, Neuberger JM. The effect of liver transplantation on fatigue in patients with primary biliary cirrhosis: a prospective study. J Hepatol. 2013; 59:490–494. PMID: 23628322.

5. Levy MF, Jennings L, Abouljoud MS, Mulligan DC, Goldstein RM, Husberg BS, et al. Quality of life improvements at one, two, and five years after liver transplantation. Transplantation. 1995; 59:515–518. PMID: 7878756.
6. Belle SH, Porayko MK, Hoofnagle JH, Lake JR, Zetterman RK. Changes in quality of life after liver transplantation among adults. National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) Liver Transplantation Database (LTD). Liver Transpl Surg. 1997; 3:93–104. PMID: 9346722.
7. Aadahl M, Hansen BA, Kirkegaard P, Groenvold M. Fatigue and physical function after orthotopic liver transplantation. Liver Transpl. 2002; 8:251–259. PMID: 11910570.

8. van den Berg-Emons R, van Ginneken B, Wijffels M, Tilanus H, Metselaar H, Stam H, et al. Fatigue is a major problem after liver transplantation. Liver Transpl. 2006; 12:928–933. PMID: 16528681.

9. van Ginneken BT, van den Berg-Emons RJ, Kazemier G, Metselaar HJ, Tilanus HW, Stam HJ. Physical fitness, fatigue, and quality of life after liver transplantation. Eur J Appl Physiol. 2007; 100:345–353. PMID: 17364193.

10. van Ginneken BT, van den Berg-Emons RJ, van der Windt A, Tilanus HW, Metselaar HJ, Stam HJ, et al. Persistent fatigue in liver transplant recipients: a two-year follow-up study. Clin Transplant. 2010; 24:E10–E16. PMID: 19744096.

12. Krupp LB, LaRocca NG, Muir-Nash J, Steinberg AD. The fatigue severity scale. Application to patients with multiple sclerosis and systemic lupus erythematosus. Arch Neurol. 1989; 46:1121–1123. PMID: 2803071.
13. Kleinman L, Zodet MW, Hakim Z, Aledort J, Barker C, Chan K, et al. Psychometric evaluation of the fatigue severity scale for use in chronic hepatitis C. Qual Life Res. 2000; 9:499–508. PMID: 11190005.
14. Merkies IS, Schmitz PI, Samijn JP, van der Meché FG, van Doorn PA. European Inflammatory Neuropathy Cause and Treatment (INCAT) Group. Fatigue in immune-mediated polyneuropathies. Neurology. 1999; 53:1648–1654. PMID: 10563607.

15. Yi NJ, Suh KS, Suh SW, Chang YR, Hong G, Yoo T, et al. Excellent outcome in 238 consecutive living donor liver transplantations using the right liver graft in a large volume single center. World J Surg. 2013; 37:1419–1429. PMID: 23467924.

16. Kalaitzakis E, Björnsson E. Fatigue and liver transplantation in patients with primary biliary cirrhosis. J Hepatol. 2014; 60:1326–1328. PMID: 24530648.

17. Bryan S, Ratcliffe J, Neuberger JM, Burroughs AK, Gunson BK, Buxton MJ. Health-related quality of life following liver transplantation. Qual Life Res. 1998; 7:115–120. PMID: 9523492.
18. Nickel R, Wunsch A, Egle UT, Lohse AW, Otto G. The relevance of anxiety, depression, and coping in patients after liver transplantation. Liver Transpl. 2002; 8:63–71. PMID: 11799488.

19. van den Berg-Emons RJ, van Ginneken BT, Nooijen CF, Metselaar HJ, Tilanus HW, Kazemier G, et al. Fatigue after liver transplantation: effects of a rehabilitation program including exercise training and physical activity counseling. Phys Ther. 2014; 94:857–865. PMID: 24557657.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download