Abstract
Backgrounds/Aims
There is debate on the timing of cholecystectomy in acute cholecystitis. Although there is a recent trend toward early laparoscopic cholecystectomy (eLC), that is, within 72 hours of symptom onset, some surgeons still prefer delayed operations, or operations after several weeks, expecting subsidence of the inflammation and therefore a higher chance of avoiding open conversion and minimizing complications. Our experience of LC for 10 years was reviewed retrospectively for the timing of the operation and perioperative outcomes, focusing on evaluating the feasibility of delayed LC (dLC).
Methods
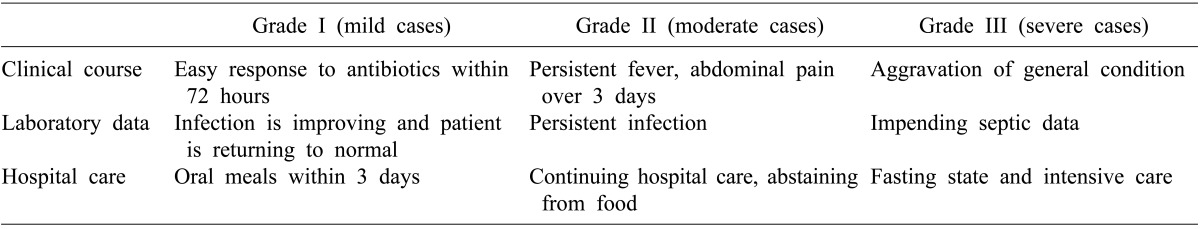
The severity of the acute cholecystitis was classified into three grades: easily responding to antibiotics and mostly symptom-free (mild, grade I), symptoms persisting during the treatment (moderate, grade II), and worsening into a septic state (severe, grade III).
Results
Among 353 cholecystectomy patients, grade I (N=224) patients had eLC in 152 cases and dLC in 72 cases. Grade II (N=117) patients had eLC in 103 cases and 12 had dLC. All grade III patients (N=12) underwent open cholecystectomy. In Grade I patients, when the operation was delayed, there were fewer open conversion cases compared to eLC patients (20.45% vs 7.69%) (p<0.05), and complications also were decreased (p>0.05). Grade II patients' rate of open conversions (58.3% vs 44.2%) and complications (25.0% vs 19.5%) increased when the operations were delayed compared with eLC patients (p<0.05). In grade I and II patients, the most common reason for open conversion was bleeding, and the most common complication was also bleeding.
Conclusions
For patients with cholecystits that easily responds to antibiotics (grade I), dLC showed a higher laparoscopic success rate than eLC at the expense of prolonged treatment time and examinations, With moderate to severe cholecystitis (grade II, III), however, there was no room for delayed operations.
Nowadays, according to recent accumulating experience of laparoscopic cholecystectomy (LC) and related techniques, early LC is recommended as a standard management method for acute cholecystitis,1-7 except when percutaneous transhepatic gallbladder drainage (PTGBD) is employed8 which is done when an operation is not feasible because of sepsis or a serious associated underlying disease. But there is still ongoing debate on early LC versus delayed LC, with some surgeons preferring to delay the operation as much as possible in acute cholecystitis, with the expectation that there will be subsidence of inflammation around the gallbladder with antibiotic use, believing that this will increase the success rate of the laparoscopic procedure and decrease the postoperative complication rate.9,10
Many reports are being published on this matter, but still, methods of classifying the degree of seriousness of the cholecystitis and the time frame of cholecystectomy have yet to be firmly determined for use in further systematic studies. Many reports classify patients into the one single entity of "acute cholecystitis", not taking into account the diversity of severity of the inflammation or the clinical course,3-5,7,11,12 and even when classifications are practiced and studies report the results, the criterion on which the classification was made is yet to be well-established. On the timing of the cholecystectomy, recently, however, most reports generally quote a time frame of less than 72 hours as an early operation and more than 6 weeks as a delayed operation.1,13
In our experience, many patients who had symptom onset for more than 3 days before they visited the hospital, or who had epigastric intermittent pain and fever when they were being treated by other clinics, or who were hesitant about having an operation experienced subsidence of their symptoms during the evaluation period at the hospital. All those patients urged us to manage them by delayed cholecystectomy. So we observed such patients, focusing on their clinical outcome, for over 10 years.
We reviewed 353 traceable operated cholecystectomy patients from March, 1998 to February, 2007 among a total of 460 cases, excluding patients who underwent coincidental operative treatment or procedures like choledochotomy and or endoscopic sphincterotomy or cases of previous upper abdominal operation, considering the possible effects of their treatment on the complication rates or postoperative course.
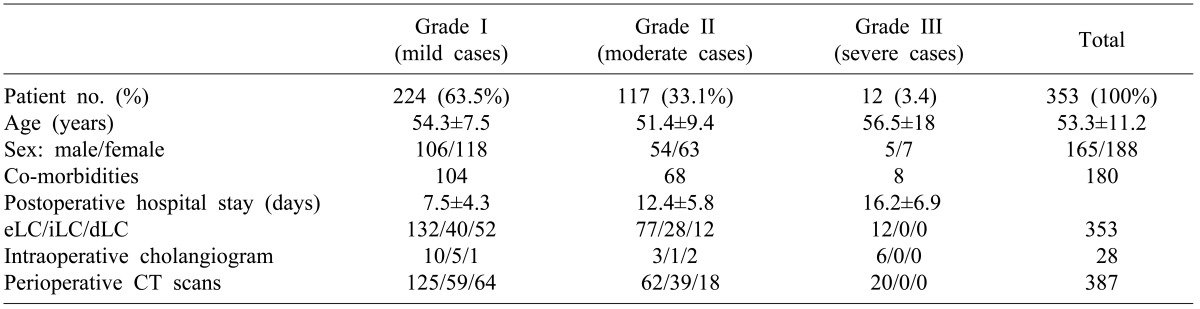
The mean age of total patients undergoing cholecystectomy was 53.3±11.2 years, and the span of hospital stay was evaluated on the postoperative period needed for recovery as shown on Table 1.
We classified the cholecystitis patients into three grades according to their clinical response to treatment: 224 cases (63.5%) who easily responded to antibiotic coverage were grade I (mild case), 117 cases (33.1%) who sustained clinical symptoms under antibiotic coverage in hospital were grade II (moderate case), and 12 cases (3.4%) who experienced aggravation of their condition and developed sepsis requiring emergent measures were grade III (severe case). The clinical features of each group are shown in Table 2.
Classification of cholecystitis was set by remotely applying the Tokyo Guide lines reported in 2007,2 which focuses on the differences in the clinical course of the patients before the operation.
Diagnosis was made mainly using computed tomography (CT) scan, which was performed 387 times for 353 patients, with ultrasound and endoscopic retrograde cholangiopancreratography (ERCP) used as needed. In 25 patients, only ultrasound was carried out before the operation. In 28 cases, 7.9% of the 353 patients receiving an operation, operative cholangiogram was performed, and all of them were open conversion cases who showed negative results for common bile duct (CBD) stones.
The necessity for operative treatment and the timing of the operation were explained to every patient, and the decision to have an operation was decided by the patient. LC was the standard first choice of operation, but antibiotic coverage was continued in patients who were hesitant about operative management; these patients were discharged on antibiotics. Antibiotic coverage was started on most patients on admission and continued throughout the evaluation period.
Early LC (eLC) was defined as an operation performed within 3 days of symptom onset. Delayed LC (dLC) was defined as an operation that was performed after the patient had gone home without having surgery after the first visit and that was delayed for 6 weeks or more, regardless of whether the patient was under antibiotic coverage or not. And the so-called interim LC (iLC) was defined as an operation that fell between the two other types of operations in features. Interim LC patients were patients who needed an urgent operation because of recurrent symptoms at home or persistent symptoms during their admission.
Except for complicated cases, successful LC patients were routinely discharged by postoperative day 3 with medications.
Laparoscopic cholecystectomy was carried out by the typical 4-hole method, and clipping of the cystic duct and cystic vasculature was carried out by applying a single Titanium clip.
When there were concerns about the risk of bleeding or when massive irrigation was necessary, a suction drain (Jackson-Pratt drain) was left in the operation field selectively.
Conversion to the open method was inevitable when the operation field was blurred by bleeding, or when the operation field could not be secured due to inflammatory tissue adhesions and swelling, or when the anatomy around Calot's triangle could not be clearly determined due to fibrous adhesive change, or when the gallbladder had been severely destroyed by inflammatory change, as listed on Table 3.
Open cholecystectomy was carried out in grade III patients (n=12) and in also 4 cases of LC because of the difficulty in visualizing the gallbladder due to inflammation.
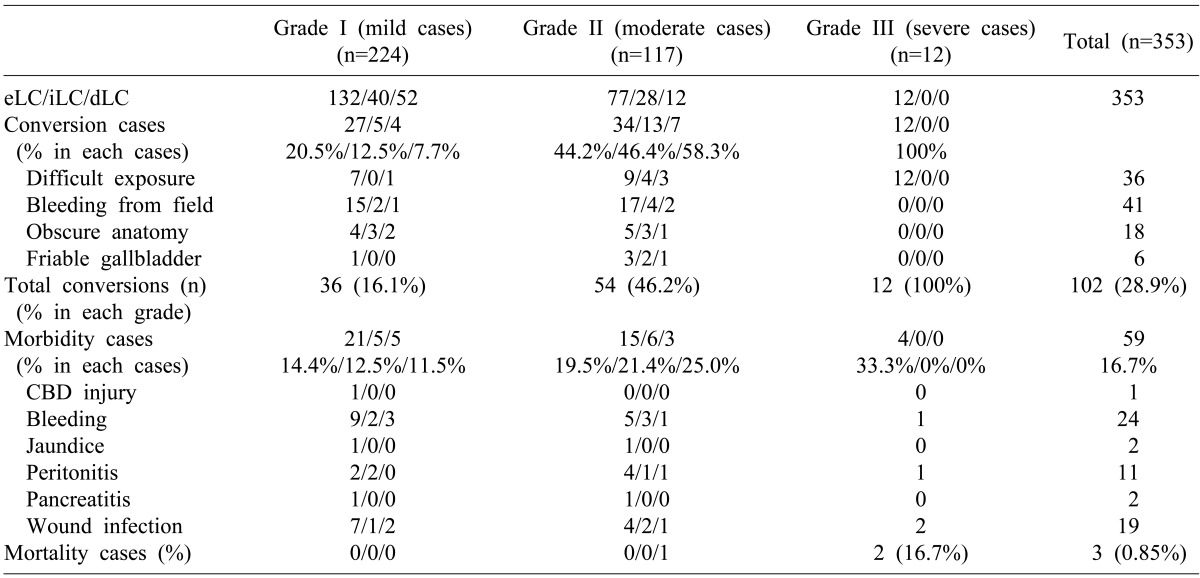
Open conversion or open cholecystectomy was carried out on 102 cases (28.9%) among the 353 cholecystitis patients in total, and complications occurred in 59 cases (16.7%).
The constitution of the patients in regard to the severity grade was 224, 117 and 12 cases for grade I, II and III respectively, accounting for 63.5%, 33.1% and 3.4% of the total population of our study, meaning more than half of the patients in the study were easily controlled by antibiotics before surgery.
Early response to antibiotics with a return to normal condition was seen in 224 cases of grade I patients, and symptoms continued in 117 cases of grade II, and aggravating symptoms lead to a preseptic condition on laboratory data and clinically in 12 cases of grade III patients.
In grade I patients, or mild cases, the rate of open conversion and complications decreased with a delay in operation time. For 132, 40, and 52 cases of early, interim, and delayed LC patients of grade I, open conversion occurred in 27, 5, 4 cases respectively, representing 20.45%, 12.5% 7.69% of the open conversion rate (p<0.05). The complication rate also decreased among grade I patients from eLC 21 (14.4%) and iLC 5 (12.5%), to dLC 5 (11.5%), although the differences were insignificant (p>0.05) (Table 3).
In grade II patients, or moderate cases, the rate of open conversion and complication rose as the operation was delayed. Open conversion increased from eLC 34 (44.2%) and iLC 13 (44.2%), to dLC 7 (58.3%) (p<0.05). The complication rate also gradually increased from eLC 15 (19.5%) and iLC 6 (21.4%), to dLC 3 (25.0%), but the differences were statistically insignificant (p>0.05) (Table 3).
As for severe cholecystitis patients of grade III, all 12 cases ended up having open cholecystectomy and intensive care. For 4 of them, laparoscopic cholecystectomy was tried initially, but gaining an adequate operation view field was not possible and they were converted. All 12 cases were operated on within 3 days of admission, and complications were seen in 4 cases (33.3%).
Open conversion was caused by bleeding, difficult exposure, obscure anatomy, and friable gallbladder according to incidence sequence. Bleeding, as a primary cause of open conversion, obstructed the view in 50.0% (18 of 36) of grade I, and 42.6% (23 of 54) of grade II patients. Especially the eLC cases faced more bleeding episodes than the dLC cases for both grade I and II. An earlier phase of inflammation, that is, within 3 days of inflammation, was more frequently associated by bleeding causing obstruction of the operating field during the laparoscopic procedure, regardless of the severity of the cholecystitis, but the differences were not significant statistically, however, due to the small parameters of bleeding episodes in the iLC and dLC cases of each grade. In grade II patients, difficult exposure of the operating site and obscure anatomy occurred twice frequently as in grade I, and friable gallbladder occurred 10 times more frequently as in grade I in its incidence, causing open conversion. The results are listed in Table 3.
Causes of postoperative morbidity were bleeding (n=24), wound infection (n=19), peritonitis (n=11), jaundice (n=2), pancreatitis (n=2), and CBD injury (n=1). Out of the total of 353 patients, 59 cases (16.7%) developed the above complications. Though the bleeding was the most frequent postoperative complication that led to open conversion, it was not related with the operative timing, constituting 40.7% of all complication incidences, a figure that is well below 50%. The three most common complications formed 91.53% of all the complications. Wound infection (n=19) happened in 18 cases of open conversion cases, with one case being infection of the umbilical port. Postoperative peritonitis appeared most frequently after grade II eLC (n=4) although this result was not statistically significant.
There were 3 cases of operative death. The first one was a grade II patient who had a delayed operation because of refusal of operation and who subsequently developed postoperative bile peritonitis and sepsis, and the second one was a grade III patient who had multi-organ failure from severe cholecystitis, and the last one was a grade III patient who had postoperative pneumonic complications and had multi-organ failure.
In spite of the recommendations for early laparoscopic cholecystectomy for acute cholecystitis, the diagnostic process which can involve a search for associated CBD stones or evaluation of accompanying diseases often causes a delay in operative treatment. Moreover, hesitation on the part of the patient to have an operation or even refusal by the patient to have operative management also causes the operative treatment to be delayed. Many patients also visit the hospital only when they are past the early operative treatment period, suffering from the symptoms of cholecystitis at home. These patients elicited our attention because the study of these patients can give information about the clinical outcomes of delayed operation.
It goes without saying that open conversion and complication rates increase as the severity grade of the cholecystitis advances from grade I to III (conversion p<0.01, complication p<0.05), as shown in Table 3.
In the cases where the symptoms were easily controled or the patients were grade I patients (n=224), and the operation was delayed or postponed at the request of the patient, patients were symptom-free at home (n=52) in more than 50% of the cases, but 40 cases were called to operation within 6 weeks after initial symptom onset. So when antibiotics were effective in returning the patients to a symptom-free normal condition in one or two days of hospitalization, we can presume (n=40+52) that 43.5% (n=40) of them will need an operation within 6 weeks due to recurrent symptoms, and the other 56.5% (n=52) can be observed at home while they remain in a symptom-free state. Additionally, we can presume that when operation is delayed in grade I patients, as shown in Table 1 and 3, the success rate of laparoscopic operation will gradually rise and the complication rate will fall gradually, as the operation timing is delayed. The difference in the open conversion rate between eLC and dLC was remarkable, 7.7% and 20.5% respectively, with an average rate of 16.1% for total grade I patients. We could not, however, review the number of times the patient experienced symptoms in the past nor review the full treatment history before the patient came to our hospital, factors which can obscure the nature of the severity of symptoms and the best timing for the operation.
In the case of grade II patients, the chances of a laparoscopic procedure or the complication rate getting worse increased with increase in delay of operation, as shown on Table 3, leaving no room for debate on the timing of the operation for grade II patients, because the results show that the earlier the operation, the more likely the patient will have a successful recovery. One notable finding was that among patients who had ongoing symptoms of acute cholecystitis, 12 cases (10.3%) among 117 patients had a delayed operation after 6 weeks of initial hospital care. Seven of those cases underwent open conversion mainly due to severe adhesions between the necrotic walls of the inflamed gallbladder and the surrounding organs, and 5 cases underwent conversion because there were difficulties in performing laparoscopic surgery on the patient. This indicates that when moderately severe acute cholecystitis is neglected in any way for more than 6 weeks, about half of them (5 of 12, 41.7%) will have the chance of having a successful LC, and the postoperative complication rate will be 25.0%. Also pertinent is that in 12 grade II patients (n=117), the inflammation of the acute cholecystitis did not progress beyond the localized area of intraperitoneal inflammation around the gallbladder and did not progress onto sepsis regardless of whether the patient was under oral antibiotics or not. Among them, 4 patients who had necrotic gallbladder with surrounding adhesions that closed off the area and prevented the dissemination of inflammation, suffered without intractable subjective symptoms at home, but were open converted during the operation. When comparing eLC and iLC in grade II patients, open conversion and postoperative complication rates were almost similar (p<0.05), so that it is possible to say that in moderately severe acute cholecystitis, a delay of operation of more than 3 days causes no different postoperative clinical outcome compared with eLC in the above aspects. Most of the iLC patients were operated on around 1 week after symptom onset and after prolonged evaluation and preparation for the operation.
The open conversion rate increased, as we expected it would, as the severity of the cholecystitis progressed from grade I to III, with rates increasing from from 16.07%, 46.15% to 100%, irrespective of the timing of the operation in each grade. Bleeding was the leading cause out of the four categories of causes shown in Table 3. In grade I and II patients, bleeding was more frequently encountered in eLC than in iLC or dLC. In grade I eLC, 15 cases out of a total of 27 eLC cases were converted by bleeding, and in grade II eLC, 17 cases out of 34 eLC cases were converted for the same reason. In other words, in grades I and II, more than half of the converted cases in early LC were caused by bleeding. The finding that the early phase of acute cholecystitis was more liable to have bleeding during the operation regardless of the severity of the cholecystitis may not be significant, however, due to the small number of bleeding episodes in the iLC and dLC cases of each grade. Other causes of open conversion throughout the different grades were rather minimal compared with bleeding, and in order of incidence, they were: difficult exposure, obscure anatomy, and friable gallbladder. Difficult exposure or a poor operation field due to inflammatory changes around the gallbladder was the leading cause of open conversion in grade III severe patients.
Causes of morbidity were mainly bleeding (n=24), wound infection (n=19), and peritonitis (n=11), altogether making up 91.5% of the total complications. And the lowest complication rate was seen in grade I with dLC, with 5 cases of complications among 52 patients. Though not significant, the complication rate was the lowest in the delayed operation group of mild cases.
During cholecystectomy for acute cholecystitis, using either open or laparoscopic surgery, 3 operative deaths (0.9%) were observed. Two of the deaths were related directly to inflammation of the gallbladder and one to postoperative pneumonia.
Many reports claim that early laparoscopic cholecystectomy for acute cholecystitis has the merits of shortening the hospital stay and that the open conversion rate or complication rate is not affected by the timing of the operation,1,14-17 but we found that delayed operation for mild cases had the lowest complication rate and the highest rate of success for laparoscopic cholecystectomy.
References
1. Ohta M, Iwashita Y, Yada K, et al. Operative timing of laparoscopic cholecystectomy for acute cholecystitis in a Japanese institute. JSLS. 2012; 16:65–70. PMID: 22906333.

2. Yamashita Y, Takada T, Kawarada Y, et al. Surgical treatment of patients with acute cholecystitis: Tokyo Guidelines. J Hepatobiliary Pancreat Surg. 2007; 14:91–97. PMID: 17252302.

3. Al-Mulhim AA. A survey of surgical management of acute cholecystitis in eastern Saudi Arabia. Saudi J Gastroenterol. 2009; 15:176–180. PMID: 19636179.

4. González-Rodríguez FJ, Paredes-Cotoré JP, Pontón C, et al. Early or delayed laparoscopic cholecystectomy in acute cholecystitis? Conclusions of a controlled trial. Hepatogastroenterology. 2009; 56:11–16. PMID: 19453020.
5. Condilis N, Sikalias N, Mountzalia L, et al. Acute cholecystitis: when is the best time for laparoscopic cholecystectomy? Ann Ital Chir. 2008; 79:23–27. PMID: 18572735.
6. Pezzolla A, Lattarulo S, Borrello G, et al. The acute cholecystitis: the operative timing for the laparoscopic approach. Ann Ital Chir. 2007; 78:475–480. PMID: 18510025.
7. Catani M, Modini C. Laparoscopic cholecystectomy in acute cholecystitis: a proposal of safe and effective technique. Hepatogastroenterology. 2007; 54:2186–2191. PMID: 18265630.
8. Han IW, Jang JY, Kang MJ, et al. Early versus delayed laparoscopic cholecystectomy after percutaneous transhepatic gallbladder drainage. J Hepatobiliary Pancreat Sci. 2012; 19:187–193. PMID: 21938408.

9. Norrby S, Herlin P, Holmin T, et al. Early or delayed cholecystectomy in acute cholecystitis? A clinical trial. Br J Surg. 1983; 70:163–165. PMID: 6338991.

10. Low JK, Barrow P, Owera A, et al. Timing of laparoscopic cholecystectomy for acute cholecystitis: evidence to support a proposal for an early interval surgery. Am Surg. 2007; 73:1188–1192. PMID: 18092660.

11. Chang TC, Lin MT, Wu MH, et al. Evaluation of early versus delayed laparoscopic cholecystectomy in the treatment of acute cholecystitis. Hepatogastroenterology. 2009; 56:26–28. PMID: 19453022.
12. Catani M, De Milito R, Romagnoli F, et al. The best timing of surgery in laparoscopic cholecystectomy for acute cholecystitis: when and how is to be performed. Hepatogastroenterology. 2008; 55:1993–1996. PMID: 19260465.
13. Cuschieri A. Approach to the treatment of acute cholecystitis: open surgical, laparoscopic or endoscopic? Endoscopy. 1993; 25:397–398. PMID: 8404709.

14. Lee AY, Carter JJ, Hochberg MS, et al. The timing of surgery for cholecystitis: a review of 202 consecutive patients at a large municipal hospital. Am J Surg. 2008; 195:467–470. PMID: 18361924.

15. Lau H, Lo CY, Patil NG, et al. Early versus delayed-interval laparoscopic cholecystectomy for acute cholecystitis: a metaanalysis. Surg Endosc. 2006; 20:82–87. PMID: 16247580.

16. Siddiqui T, MacDonald A, Chong PS, et al. Early versus delayed laparoscopic cholecystectomy for acute cholecystitis: a meta-analysis of randomized clinical trials. Am J Surg. 2008; 195:40–47. PMID: 18070735.

17. Popkharitov AI. Laparoscopic cholecystectomy for acute cholecystitis. Langenbecks Arch Surg. 2008; 393:935–941. PMID: 18299882.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download