Abstract
The aim of this study was to compare nutrient intakes, serum hormones (leptin, adiponectin, insulin), salivary cortisol and α-amylase of middle-aged women by the percentage of body fat (% fat). Subjects were assigned to 3 groups by body fat (%) group I (27.5%), group II (32.5%), group III (37.7%). WHR of group II (0.97) was significantly higher than of group I, III (0.95) (p < 0.05). Nutrient intakes were not different among 3 groups. Serum leptin levels of group III (16.53 µg/ml) were higher than in group I (10.07 µg/ml), group II (12.24 µg/ml) (p < 0.05). Salivary cortisol levels of group II (0.39 µg/dl) were higher than in group I (0.17 µg/dl) and group III (0.15 µg/dl) (p < 0.05). Adiponectin concentrations were negatively correlated with TAS (r = -0.29) and positively correlated with HDL cholesterol (r = 0.27). Insulin levels were negatively correlated with total cholesterol (r = -0.33), Zn intake (r = -0.31) and positively correlated with WHR (r = 0.31). The overall anthropometric indices showed positive relations with leptin levels. Salivary cortisol levels were positively corelated with WHR (r = 0.28), total cholesterol (r = 0.31), MDA (r = 0.29) and intakes of SFA (r = 0.35) and MUFA (r = 0.3). Salivary amylase levels were positively correlated with overall nutrient intakes (energy, CHO, fat, cholesterol. Fe, SFA, MUFA, Zn, Na, vitamin B2, r = 0.24-0.5) and was negatively correlated with HDL cholesterol (r = -0.34). These results suggested that 1) WHR would be a helpful index in the assessment of metabolic risk diseases. 2) Understanding of individual stress exposure should be considered in developing strategies for prevention and treatment of obesity.
Figures and Tables
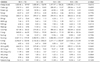
Table 1
Anthropometric measurements by the fat% of the subjects

Subject were assigned to 3 groups by % fat: group I (27.5%), group II (32.5%), group III (37.7%)
WC: Waist circumference
HC: Hip circumference
TST: Triceps skinfold thickness
SST: Suprailliac skinfold thickness
AST: Abdomen skinfold thickness
ICF: Intracellular fluid
ECF: Extracellular fluid
1) Mean ± SE (Age : Mean ± SD)
a,b,c: Alphabet letters mean significant difference statistically
References
1. Bełtowski J. Leptin and the regulation of endothelial function in physiological and pathological conditions. Clin Exp Pharmacol Physiol. 2012. 39(2):168–178.
2. Bosy-Westphal A, Brabant G, Haas V, Onur S, Paul T, Nutzinger D, Klein H, Hauer M, Müller MJ. Determinants of plasma adiponectin levels in patients with anorexia nervosa examined before and after weight gain. Eur J Nutr. 2005. 44(6):355–359.
3. Bruun JM, Lihn AS, Verdich C, Pedersen SB, Toubro S, Astrup A, Richelsen B. Regulation of adiponectin by adipose tissue-derived cytokines: in vivo and in vitro investigations in humans. Am J Physiol Endocrinol Metab. 2003. 285(3):E527–E533.
4. Canas JA, Damaso L, Altomare A, Killen K, Hossain J, Balagopal PB. Insulin resistance and adiposity in relation to serum β-carotene levels. J Pediatr. 2012. 161(1):58–64.
5. Chang HS. Nutrient intakes and blood lipids according to obesity degree by body fat percentage among middle-aged women in gunsan city. Korean J Community Nutr. 2010. 15(1):15–26.
6. Daimon M, Oizumi T, Saitoh T, Kameda W, Hitra A, Yamaguchi H, Ohnuma H, Igarashi M, Tominaga M, Kato T. Decreased serum levels of adiponectin are a risk factor for the progression to type 2 diabetes in the japanes population. Diabetes Care. 2003. 26(7):2015–2020.
7. Dockray S, Susman EJ, Dorn LD. Depression, cortisol reactivity, and obesity in childhood and adolescence. J Adolesc Health. 2009. 45(4):344–350.
8. Duclos M, Gatta B, Corcuff JB, Rashedi M, Pehourcq F, Roger P. Fat distribution in obese women is associated with subtle alterations of the hypothalamic-pituitary-adrenal axis activity and sensitivity to glucocorticoids. Clin Endocrinol. 2001. 55(4):447–454.
9. Duclos M, Marquez Pereire P, Barat P, Gatta B, Roger P. Increased cortisol bioavailability, abdominal obesity, and the metabolic syndrome in obese women. Obes Res. 2005. 13(7):1157–1166.
10. Fernández-Sánchez A, Madrigal-Santillán E, Bautista M, Esquivel-Soto J, Morales-González A, Esquivel-Chirino C, Durante-Montiel I, Sánchez-Rivera G, Valadez-Vega C, Morales-González JA. Inflammation, oxidative stress, and obesity. Int J Mol Sci. 2011. 12(5):3117–3132.
11. Fried SK, Ricci MR, Russell CD, Lafferrere B. Regulation of leptin production in humans. J Nutr. 2000. 130(12):3127S–3131S.
12. Fukui T, Yamauchi K, Maruyama M, Yasuda T, Kohno M, Abe Y. Significance of measuring oxidative stress in lifestyle-related diseases from the viewpoint of correlation between d-ROMs and BAP in Japanese subjects. Hypertens Res. 2011. 34(9):1041–1045.
13. García-Prieto MD, Tébar FJ, Nicolás F, Larqué E, Zamora S, Garaulet M. Cortisol secretary pattern and glucocorticoid feedback sensitivity in women from a mediterranean area: relationship with anthropometric characteristics, dietary intake and plasma fatty acid profile. Clin Endocrinol (Oxf). 2007. 66(2):185–191.
14. Gavrila A, Chan JL, Yiannakouris N, Kontogianni M, Miller LC, Orlova C, Mantzoros CS. Serum adiponectin levels are inversely associated with overall and central fat distribution but are not directly regulated by acute fasting or leptin administration in humans: cross-sectional and interventional studies. J Clin Endocrinol Metab. 2003. 88(10):4823–4831.
15. Groesz LM, McCoy S, Carl J, Saslow L, Stewart J, Adler N, Laraia B, Epel E. What is eating you? Stress and the drive to eat. Appetite. 2012. 58(2):717–721.
16. James PT, Leach R, Kalamara E, Shayeghi M. The worldwide obesity epidemic. Obes Res. 2001. 9:Suppl 4. 228S–233S.
17. Kadowaki T, Yamauchi T, Kubota N, Hara K, Ueki K, Tobe K. Adiponectin and adiponectin receptors in insulin resistance, diabetes, and the metabolic syndrome. J Clin Invest. 2006. 116(7):1784–1792.
18. Kang SJ, Shin YA, Kim KJ. The differences of ghrelin, adiponectin, and aerobic capacity by menopause and obesity and its inter-correlation with body composition indexes. Korean J Sport Sci. 2008. 19(2):51–59.
19. Kim SJ, Park KG, Kim HK, Kim MK, Lee SW, Hwang JS, Han SW, Hur SH, Lee IK. Serum adiponectin concentration according to visceral fat amount and its relationship of metabolic risk factors in premenopausal obese women. Korean J Med. 2004. 66(3):259–266.
20. Lee HJ, Lee DH, Kim KO, Kim YJ, Lee HY. Analysis of serum antioxidant materials concentration and their relation with blood lipids and anthropometric indices in middle-aged adult in Korea. Korean J Nutr. 2009. 42(5):464–473.
21. Lee MY, Kim JH. Association of serum lipids and dietary intakes with serum adiponectin level in overweight and obese Korean women. Korean J Community Nutr. 2010. 15(1):27–35.
22. Lee MY, Kim JH. Comparison of serum insulin, leptin, adiponectin and high sensitivity c-reactive protein levels according to body mass index and their associations in adult women. Korean J Community Nutr. 2011. 16(1):126–135.
23. Lee SE, Moon JH, Ahn JH, Oh YS, Shinn SH. The association between plasma adiponectin and the components of metabolic syndrome in adults with abdominal obesity. Korean J Obes. 2007. 16(4):147–153.
24. Lee SW, Kim MR, You YO. Recent clinical review : Adipokines, the obesity and metabolic complications in the postmenopausal women. Korean J Obstet Gynecol. 2009. 52(12):1204–1211.
25. Melissas J, Malliaraki N, Papadakis JA, Taflampas P, Kampa M, Castanas E. Plasma antioxidant capacity in morbidly obese patients before and after weight loss. Obes Surg. 2006. 16(3):314–320.
26. Mohn A, Catino M, Capanna R, Giannini C, Marcovecchio M, Chiarelli F. Increased oxidative stress in prepubertal severely obese children: effect of a dietary restriction-weight loss program. J Clin Endocrinol Metab. 2005. 90(5):2653–2658.
27. Münzberg H, Myers MG Jr. Molecular and anatomical determinants of central leptin resistance. Nat Neurosci. 2005. 8(5):566–570.
28. Schwarz NA, Rigby BR, La Bounty P, Shelmadine B, Bowden RG. A review of weight control strategies and their effects on the regulation of hormonal balance. J Nutr Metab. 2011. 2011:237932.
29. Ali N, Pruessner JC. The salivary alpha amylase over cortisol ratio as a marker to assess dysregulations of the stress systems. Physiol Behav. 2012. 106(1):65–72.
30. Oltmanns KM, Dodt B, Schultes B, Raspe HH, Schweiger U, Born J, Fehm HL, Peters A. Cortisol correlates with metabolic disturbances in a population study of type 2 diabetic patients. Eur J Endocrinol. 2006. 154(2):325–331.
31. Ouchi N, Kihara S, Arita Y, Maeda K, Duriyama H, Okamoto Y, Hotta K, Nishida M, Takahashi M, Nakamura T, Yamashita S, Funahashi T, Matsuzawa Y. Novel molecules: adipocyte-derived plasma protein adiponectin. Circulation. 1999. 100(25):2473–2476.
32. Ozata M, Mergen M, Oktenli C, Aydin A, Sanisoglu SY, Bolu E, Yilmax MI, Sayal A, Isimer A, Ozdemir IC. Increased oxidative stress and hypozincemia in male obesity. Clin Biochem. 2002. 35(8):627–631.
33. Park SB, Blumenthal JA, Lee SY, Georgiades A. Association of cortisol and the metabolic syndrome in Korean men and women. J Korean Med Sci. 2011. 26(7):914–918.
34. Reaven GM. Role of insulin resistance in human disease. Diabetes. 1988. 37(12):1595–1607.
35. Rolland YM, Perry HM 3rd, Patrick P, Banks WA, Morley JE. Leptin and adiponectin levels in middle-aged postmenopausal women: associations with lifestyle habits, hormones, and inflammatory markers--a cross-sectional study. Metabolism. 2006. 55(12):1630–1636.
36. Rosmond R, Björntorp P. Endocrine and metabolic aberrations in men with abdominal obesity in relation to anxio-depressive infirmity. Metabolism. 1998. 47(10):1187–1193.
37. Roubenoff R. Sarcopenic obesity: The confluence of two epidemics. Obes Res. 2004. 12(6):887–888.
38. Srdic B, Stokic E, Polzovic A, Babovic S. Abdominal adipose tissue-significance and methods of defection. Med Pregl. 2005. 58:258–264.
39. Steptoe A, Kunz-Ebrecht SR, Brydon L, Wardle J. Central adiposity and cortisol responses to waking in middle-aged men and women. Int J Obes Relat Metab Disord. 2004. 28(9):1168–1173.
40. Sung CJ, Kim EY. A study of nutritional status and antioxidant capacity according to obesity index in postmenopausal women. J Korean Soc Study Obes. 2003. 12(3):193–202.




 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download