Abstract
Purpose
The purpose of this study is to determine whether or not a patient's results are improved after removal of an internal fixative from a patient with no related symptoms.
Materials and Methods
This prospective study included 87 patients who agreed to participate in the study and satisfied the criteria for selection and exclusion of patients who underwent the operation for removal of internal fixative due to broken bones from March 1st, 2004 to December 31st, 2011 at Daegu Catholic University Medical Center. The average replication period was 27 months (12-64 months) and the average age at the time of the operation for removal was 41.5 years (21-75 years) for 55 males and 32 females. The quality of life for all patients was evaluated using Short Form 36 (SF-36) surveys before the operation for removal and after a minimum of one year.
Results
After an orthopedic operation for removal of internal fixative, physical health status showed statistically significant improvement (p=0.001); however mental health status did not (p=0.411). A satisfaction test for the subjective surgery written by patients indicated an improvement of subjective health status in 52.9% after the surgery for removal but with no difference in 29.9% compared to preoperation.
Conclusion
In case of an operation for removal of internal fixative for patients with no related symptoms with internal fixatives used for treatment of fractures showing agglutination opinions, an improvement was observed in physical health status, not in mental health status. When surgery for removal of internal fixative is performed for patients without related symptoms, consideration that subjective satisfaction of patients shows an improvement only in 52.9% will be helpful.
Figures and Tables
Table 1
Characteristics of Populations
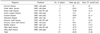
Table 2
Results of Functional Outcome
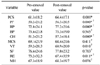
Values are presented as mean±standard deviation. *p<0.05. † Wilcoxon sighed rank test was used for statistical analysis. PCS: Physical component score in Short Form 36 (SF-36), PF: Physical functioning, RP: Role limitation due to physical health problem, BP: Bodily pain, GH: General health, MCS: Mental component score in SF-36, VT: Vitality, SF: Social-functioning, RE: Role limitation due to emotional problems, MH: Mental health.
References
1. Jamil W, Allami M, Choudhury MZ, Mann C, Bagga T, Roberts A. Do orthopaedic surgeons need a policy on the removal of metalwork? A descriptive national survey of practicing surgeons in the United Kingdom. Injury. 2008; 39:362–367.

2. Richards RH, Palmer JD, Clarke NM. Observations on removal of metal implants. Injury. 1992; 23:25–28.

3. Busam ML, Esther RJ, Obremskey WT. Hardware removal: indications and expectations. J Am Acad Orthop Surg. 2006; 14:113–120.

4. Böstman O, Pihlajamäki H. Routine implant removal after fracture surgery: a potentially reducible consumer of hospital resources in trauma units. J Trauma. 1996; 41:846–849.
5. Hanson B, van der Werken C, Stengel D. Surgeons' beliefs and perceptions about removal of orthopaedic implants. BMC Musculoskelet Disord. 2008; 9:73.

7. Böstman OM. Refracture after removal of a condylar plate from the distal third of the femur. J Bone Joint Surg Am. 1990; 72:1013–1018.

8. Deluca PA, Lindsey RW, Ruwe PA. Refracture of bones of the forearm after the removal of compression plates. J Bone Joint Surg Am. 1988; 70:1372–1376.

9. Hidaka S, Gustilo RB. Refracture of bones of the forearm after plate removal. J Bone Joint Surg Am. 1984; 66:1241–1243.

10. Langkamer VG, Ackroyd CE. Removal of forearm plates A review of the complications. J Bone Joint Surg Br. 1990; 72:601–604.

11. Mih AD, Cooney WP, Idler RS, Lewallen DG. Longterm follow-up of forearm bone diaphyseal plating. Clin Orthop Relat Res. 1994; (299):256–258.

12. Rosson JW, Shearer JR. Refracture after the removal of plates from the forearm. An avoidable complication. J Bone Joint Surg Br. 1991; 73:415–417.

13. Beaupre GS, Csongradi JJ. Refracture risk after plate removal in the forearm. J Orthop Trauma. 1996; 10:87–92.

14. Davison BL. Refracture following plate removal in supracondylar-intercondylar femur fractures. Orthopedics. 2003; 26:157–159.

15. Gösling T, Hufner T, Hankemeier S, Zelle BA, Muller-Heine A, Krettek C. Femoral nail removal should be restricted in asymptomatic patients. Clin Orthop Relat Res. 2004; (423):222–226.

16. Brown OL, Dirschl DR, Obremskey WT. Incidence of hardware-related pain and its effect on functional outcomes after open reduction and internal fixation of ankle fractures. J Orthop Trauma. 2001; 15:271–274.

17. Raman R, Roberts CS, Pape HC, Giannoudis PV. Implant retention and removal after internal fixation of the symphysis pubis. Injury. 2005; 36:827–831.

18. Townend M, Parker P. Metalwork removal in potential army recruits. Evidence-based changes to entry criteria. J R Army Med Corps. 2005; 151:2–4.

19. Evers B, Habelt R, Gerngross H. Indication, timing and complications of plate removal after forearm fractures: results of metaanlysis including 635 cases. J Bone Joint Surg Br. 2004; 86:289–294.
20. Chia J, Soh CR, Wong HP, Low YP. Complications following metal removal: a follow-up of surgically treated forearm fractures. Singapore Med J. 1996; 37:268–269.
22. Rumball K, Finnegan M. Refractures after forearm plate removal. J Orthop Trauma. 1990; 4:124–129.

23. Vos D, Hanson B, Verhofstad M. Implant removal of osteosynthesis: the Dutch practice. Results of a survey. J Trauma Manag Outcomes. 2012; 6:6.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download