Abstract
A 54-year-old woman with long-lasting pleural effusion developed abdominal distention due to ascites from bilateral ovarian tumors. The patient had undergone breast-conserving surgery and axillary lymph node dissection for left breast cancer in October 2000, and had developed left pleural effusion in July 2006. Cytological examination of the pleural effusion found no malignant cells. Thoracic drainage with intrathoracic administration of OK-432 (Picibanil) had failed to control the pleural effusion. Positron emission tomography taken at the abdominal distention showed bilateral ovarian tumors. After failure to control the ascites with systemic and intra-abdominal chemotherapy, bilateral oophorectomy resulted in normalization of elevated serum tumor-marker levels and the disappearance of both the ascites and pleural effusions (i.e., pseudo-Meigs' syndrome). Pathological examination showed the tumors to be estrogen receptor-positive metastatic ovarian tumors from her breast cancer. The patient remained well with no further recurrence for 40 months under aromatase inhibitor therapy.
Meigs' syndrome is characterized by ascites and pleural effusion associated with benign ovarian tumors such as fibroma, thecoma, Brenner's tumor, or granulosa cell tumor [1-3]. Its characteristic symptoms generally disappear after removal of the ovarian tumor. Pseudo-Meigs' syndrome is defined as a syndrome which shows similar symptoms to Meigs' syndrome in patients with malignant ovarian tumors [4]. However, pseudo-Meigs' syndrome from breast cancer is extremely rare and very poor prognoses after clinical manifestation of pseudo-Meigs' syndrome have been reported [5,6].
Breast cancer often develops pleural metastases, especially in the ipsilateral pleura, resulting in pleural effusion. Pleural effusion in the ipsilateral thorax caused by pseudo-Meigs' syndrome can thus mislead physicians and complicate treatment decisions. We report here a very rare case of pseudo-Meigs' syndrome originated from breast cancer, which was treated successfully with oophorectomy.
A 54-year-old woman complained of abdominal fullness in February 2009. She had undergone breast-conserving surgery and axillary lymph node dissection for left breast cancer in October 2000, and had subsequently developed left pleural effusion (Figure 1A) in July 2006. Thoracic drainage with intrathoracic administration of OK-432 had failed to control the pleural effusion, which contained no cancer cells. The patient experienced variable amounts of pleural effusion and was followed on an outpatient basis for the next 30 months.
The patient then developed abdominal distention with elevated serum levels of carcinoembryonic antigen (CEA) and carbohydrate antigen (CA) 15-3 (Figure 2). Positron emission tomography/computed tomography (PET/CT) showed bilateral ovarian tumors (Figure 3) with ascites. Systemic chemotherapy (weekly paclitaxel 80 mg/m2) and intra-abdominal chemotherapy (carboplatin 100 mg/m2) with repeated aspirations (4,000-8,500 mL) failed to control the ascites. Bilateral oophorectomies were performed to provide a definitive diagnosis of the ovarian tumors and to establish some therapeutic clues for controlling the ascites. The right and left ovaries were weighed 15 and 250 g (left tumor), respectively and were lobulated. No tumor dissemination was observed in the abdomen and the ascites contained no cancer cells cytologically. Pathological examination showed that the tumors were composed of solid and luminal structures (Figure 4A) and were positive for estrogen receptor (Figure 4B), progesterone receptor, cytokeratin (CK)-7, and gross cystic disease fluid protein-15 (Figure 4C), and negative for HER2 overexpression and CK20. These pathological findings suggested that the bilateral ovarian tumors originated from the patient's breast cancer.
The patient was discharged 9 days after surgery. The left pleural effusion disappeared (Figure 1B) and serum CEA and CA 15-3 levels decreased below the normal upper limit (Figure 2). The patient remained well under aromatase inhibitor therapy with no further recurrence for 40 months after the oophorectomies.
The etiology of ascites and pleural effusion in Meigs' syndrome remains unclear [7]. Meigs himself suggested that hard ovarian tumors could irritate the peritoneum and stimulate the production of peritoneal fluid. Abramov et al. [8] suggested that inflammatory cytokines such as interleukin (IL)-6, IL-1β, and IL-8 play an important role in the formation of ascites and pleural effusion in Meigs' syndrome. The most common etiology of pleural effusion is thought to involve facilitated migration of ascites to the thoracic cavity via the trans-diaphragmatic lymphatic system [7]. However, because the onset of pleural effusion preceded the onset of ascites, we were unable to confirm the etiology of the pleural effusion in the present case.
The prognosis of ovarian metastasis is generally poor [9]. Shiromizu et al. [10] reported overall survival rates in patients with ovarian metastases of 42%, 25%, and 13% at 6 months, 1 year, and 2 years, respectively, but these survival rates were improved to 75%, 63%, and 25% in patients without extraovarian metastases after oophorectomies. Patients with ovarian metastases often experience a reduction or complete disappearance of ascites and pleural effusion after oophorectomy, leading to an improved quality of life.
Several reports have suggested that intra-abdominal injection of anticancer drugs might provide effective treatment for ovarian cancer and peritoneal dissemination [11,12]. The vast majority of patients with metastatic ovarian cancer develop intra-abdominal dissemination after oophorectomy, which supports the use of intra-abdominal chemotherapy with oophorectomy when possible. However, systemic and intra-abdominal chemotherapy failed to control the ascites before oophorectomy in the present patient, and we were therefore unable to draw any conclusions about the clinical importance of intra-abdominal chemotherapy.
Breast cancer often develops metastases to the lung, bone, liver, and brain, but the ovary is not a common target organ for breast cancer metastasis; however, breast cancer is the leading cause of ovarian metastasis from extra-abdominal malignancies. Unfortunately, the presence of ipsilateral pleural effusion in this case was misinterpreted as being caused by pleural metastasis from breast cancer, despite the lack of distinct pleural nodules on CT. It seems appropriate to interpret the pleural effusion and ascites in this case caused by pseudo-Meigs' syndrome because of the absence of malignant cells both in the pleural effusion and the ascites.
Metastatic breast cancers are usually treated according to Hortobagyi's algorithm [13], which aims for long-term symptom relief with possible elongation of survival, rather than for cure. However, potentially curative multidisciplinary therapies can now be used for oligometastatic breast cancers [14,15]. Although the volume of the ovarian metastasis was bulky in this case, surgical intervention to the ovaries seems to be a feasible measure under the concept of oligometastatic breast cancer because no cancer cells were detected in the pleural effusion or the ascites.
In conclusion, bilateral oophorectomy led to complete remission for 40 months in a patient with ovarian metastasis from breast cancer and this is the first case of pseud-Meigs' syndrome treated successfully. Breast oncologists should thus consider oophorectomy in patients with presumed pseudo-Meigs' syndrome without extraovarian metastatic foci.
Figures and Tables
Figure 1
Chest computed tomography (CT). (A) Chest CT before thoracic drainage. Massive pleural effusion in the left thorax causing deviation of the mediastinum. (B) Chest CT after bilateral oophorectomies. The pleural effusion disappeared completely.

Figure 2
Serum carcinoembryonic antigen (CEA) and carbohydrate antigen (CA) 15-3 levels. CEA and CA 15-3 levels decreased sharply within the normal upper limits after bilateral oophorectomies.
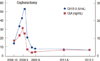
Figure 3
Pelvic computed tomography at abdominal distention showing a large mass (arrow) and ascites in the pelvic cavity.

Figure 4
Pathological examinations. (A) Tumors were composed of solid and luminal structures (H&E stain,×100). (B) Tumors were highly estrogen receptor-rich (immunohistochemistry,×100). (C) Gross cystic disease fluid protein-15 was highly positive, especially in the luminal part of the tumor (immunohistochemistry, ×100).

References
1. Meigs JV, Cass JW. Fibroma of the ovary with ascites and hydrothorax. Am J Obstet Gynecol. 1937. 33:249–267.

2. Rhoads JE, Terrell AW. Ovarian fibroma with ascites and hydrothorax (Meigs's syndrome): report of a case. JAMA. 1937. 109:1684–1687.

3. Meigs JV, Armstrong SH, Hamilton HH. A further contribution to the syndrome of fibroma of the ovary with fluid in the abdomen and chest, Meigs' syndrome. Am J Obstet Gynecol. 1943. 46:19–37.

4. Meigs JV. Pelvic tumors other than fibromas of the ovary with ascites and hydrothorax. Obstet Gynecol. 1954. 3:471–486.

5. Fujii M, Okino M, Fujioka K, Yamashita K, Hamano K. Pseudo-Meigs' syndrome caused by breast cancer metastasis to both ovaries. Breast Cancer. 2006. 13:344–348.

6. Kawakubo N, Okido M, Tanaka R, Mitsugi K, Fukuhara M, Aishima S, et al. Pseudo-Meigs' syndrome associated with breast cancer metastasis to both ovaries: report of a case. Surg Today. 2010. 40:1148–1151.

7. O'Flanagan SJ, Tighe BF, Egan TJ, Delaney PV. Meigs' syndrome and pseudo-Meigs' syndrome. J R Soc Med. 1987. 80:252–253.
8. Abramov Y, Anteby SO, Fasouliotis SJ, Barak V. The role of inflammatory cytokines in Meigs' syndrome. Obstet Gynecol. 2002. 99:917–919.

9. Gagnon Y, Têtu B. Ovarian metastases of breast carcinoma. A clinicopathologic study of 59 cases. Cancer. 1989. 64:892–898.

10. Shiromizu K, Kawana T, Sugase M, Izumi R, Mizuno M. Experience with the treatment of metastatic ovarian carcinoma. Arch Gynecol Obstet. 1988. 243:111–114.

11. Tsubono M, Kaneko I, Kii E, Tanaka T, Murata T, Kamimura K, et al. Weekly paclitaxel administration and intraabdominal CBDCA injection possibly beneficial treatment for recurrent breast cancer associated with metastatic ovarian cancer and peritoneal dissemination after operation: a case report. Gan To Kagaku Ryoho. 2005. 32:365–369.
12. Ishibashi M, Nakayama K, Oride A, Yeasmin S, Katagiri A, Iida K, et al. A case of PEP(BEP)-resistant ovarian dysgerminoma successfully treated by VeIP therapy. Gan To Kagaku Ryoho. 2009. 36:513–517.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download