Abstract
Purpose
This study was designed to evaluate the mid-term results and efficacy of subtalar distraction double bone-block arthrodesis for calcaneal malunion.
Materials and Methods
From January 2004 to June 2007, we operated on 6 patients (10 cases). There were 5 males (9 cases) and 1 female (1 case), four of which presented with bilateral calcaneal malunion. Seven cases were operated on initially. The period between initial injury and arthrodesis was 23 months, and the average follow up period was 58 months. In operation, we applied an extensile lateral approach and arthrodesis was performed through a tricortical double bone-block and cannulated screws. The American Orthopaedic Foot and Ankle Society (AOFAS) Ankle-Hindfoot scale was used for clinical evaluation. In radiologic analysis, plain X-ray and CT were examined to assess union and various parameters.
Results
The mean age of the patients was 41 years. All cases achieved radiologic union at the final follow-up. The mean AOFAS Ankle-Hindfoot scale (maximum of 94 points) increased from 43.3 points preoperatively to 85.4 points at the final follow-up. The radiologic analysis of the pre- and postoperative standing lateral radiographs showed improvements of 5.6 mm in talo-calcaneal height, 1.8° in talocalcaneal angle, 5.1° in talar declination angle and 5.3° in talo-first metatarsal angle.
Conclusion
Subtalar distraction two bone-block arthrodesis provides overall good results not only in the short term but also the mid-term with significant improvement in clinical and radiologic outcomes. This procedure warrants consideration for managing calcaneal malunion with loss of height and subtalar arthritis.
Calcaneal malunion causes complications of traumatic subtalar arthritis, peroneal tendon lesions like as tendinitis, entrapment, anterior ankle impingement syndrome and varus or valgus hindfoot deformity.1,2,3,4,5,6,7,8,9 Although subtalar arthrodesis is capable of relieving subtalar arthritic pain, if arthritis is accompanied by severe deformity, it is difficult to correct calcaneal height, talar declination angle, or talocalcaneal angle caused by malunion.
Subtalar distraction arthrodesis for restoration of calcaneal height was introduced by Carr, et al.4 This involves a combined surgery with subtalar arthrodesis and realignment surgery for hindfoot deformity using iliac crest bone block graft. Since the operation was introduced, many researchers have reported it to be effective.
Previous authors reported the results of subtalar distraction arthrodesis using a single bone block; however, we experienced subsidence of grafted bone during long-term follow-up.10 In order to solve this problem, we performed subtalar distraction arthrodesis using double bone-blocks and analyzed the results at mid-term follow up.
From January 2004 to June 2007, we carried out retrospective analysis on 6 patients (10 cases) who underwent operation for calcaneal malunion and subtalar arthritis resulting from a complication of intra-articular calcaneal fracture. The average follow-up period was 58 months (from 32 to 113 months). There were 5 males (9 cases) and 1 female (1 case), four of which presented with bilateral calcaneal malunion. The average age thereof was 41 years (ranging from 26- to 64-years-old).
The initial treatments for calcaneal fracture comprised three conservative approaches with a cast and seven surgical approaches, including four percutaneous pinnings and three open reductions and internal fixation with a plate and screws. The average period until they received arthrodesis after their initial injury or surgery was 23 months, except for 1 patient who visited the hospital because of complication due to a fracture that occurred 30 years prior.
All patients complained of severe pain along the distal fibula and subtalar joint. Also, decreased talo-calcaneal height and subtalar arthritis were found radiographically. The patients reported being treated with conservative treatments, such as medication, physical therapy, and orthopedic shoes, but these were ineffective. Severe range of motion limitations of the subtalar joint were found in all cases upon physical examination, and severe range of motion limitations of the ankle in the sagittal plane were found in three of these. Two cases of valgus deformity of the hindfoot and 1 case of flatfoot deformity was observed. Also, hammer toe deformity of the second, third, and fourth toes were observed in another 1 case.
Plain X-rays were generated for the bilateral foot, taken in the same condition with full weight-bearing to evaluate the degree of deformity. In lateral views, the degree of hindfoot deformity in the sagittal plane was assessed by measuring the talo-calcaneal height, the talo-calcaneal angle, the talar declination angle, and the talo-first metatarsal angle. The talo-calcaneal height comprised the distance from the base of the calcaneus to the dome of the talus. Measurement of the talo-calcaneal angle was made along the long axis of the talus and its intersection with the longitudinal axis of the calcaneus. The talar declination angle was measured at the axis of the talus and the plane of support. The talo-first metatarsal angle was measured from the axis of the talus to the axis of the first metatarsal bone (Fig. 1).4,11 The degree of valgus and varus deformity in the coronal plane of the calcaneus was estimated in the calcaneal axial view. Computed tomography was performed on all patients to examine calcaneofibular impingement due to a bony prominence of the lateral calcaneus or talar arthritis.12 Based on these examinations, we planned surgery taking into consideration the extent of subtalar distraction, removal range of bony prominences, and correction degrees of valgus and varus deformity.13
Radiological parameters were assessed and compared at 12 months after surgery and at final follow-up. In radiologic analysis, we used paired t-test (SPSS 12.0, SPSS Inc., Chicago, IL, USA, p<0.05) and confirmed if there are significant differences between points preoperatively and points at final follow-up.
The patient was placed in the lateral decubitus position with the affected side up and a compressive thigh tourniquet was applied. An extensile lateral approach via an L-shaped incision along the lateral aspect was applied (Fig. 2A).8 After the sural nerve and peroneal tendon were identified and protected, an incision was made to the calcaneal periosteum and bony prominences of the lateral calcaneus were removed. Using a lamina spreader, the subtalar joint was exposed, and then the residual cartilage was debrided and the subchondral surface prepared (Fig. 2B). While holding the subtalar joint in distraction, we paid attention to avoid injury to the flexor digitorum longus tendon and to maintain the hindfoot in a neutral or a little everted position after the medial articular capsule of the subtalar joint was separated enough.
The degree of distraction was determined by measuring the loss of height in comparison with an unaffected site. In bilateral cases, this was determined according to the correction degree of the talo-first metatarsal angle.
After fluoroscopic analysis confirmed the corrected height of the hindfoot, talar declination angle, alignment, and stability, two 6.5 mm cannulated screws were inserted from the posteroinferior calcaneus to the dome of the talus. During screw insertion, the tricortical double bone-blocks needed to be protected (Fig. 2C).
During the operation, we first removed sclerotic portions of the subtalar joint and subchondral surfaces. Then, the subtalar joint space was measured again and tricortical double bone-blocks (Fig. 3) to fit the space were harvested from the iliac crest. Then, the bone block was placed in the subtalar joint with cancellous bone.
The patient started ROM exercises of the ankle at postoperative 4 weeks and was allowed to bear weight gradually from postoperative 8 weeks. Full weight bearing was allowed when radiological findings showed subtalar joint union.
Clinically, the American Orthopaedic Foot and Ankle Society (AOFAS) ankle-hindfoot score was assessed before and after operation. At the final follow-up, physical examination and ankle-hindfoot score were assessed.
AOFAS Ankle-Hindfoot scores (100 points) were obtained both before surgery and at final follow-up. Any pain, function, and alignment were also evaluated. A score of 100 points means that the patient has no pain, no limitation of ROM, is stable, and in good alignment. It also means that the patient can walk over six blocks without any help, and has no problem in performing daily activities. Of the possible 100 points on the hindfoot score, the maximum possible for a patient who has undergone subtalar arthrodesis is 94 because of loss of subtalar movement.14,15
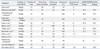
The patient was assessed in regards to pain score and total AOFAS Ankle-Hindfoot score. The mean pain score was 11.4 points before operation and 35.7 points after operation. The mean AOFAS ankle-hindfoot score including the pain score was 43.3 points (12 to 66) before operation and 84.0 points (range, 74 to 91) after operation. These scores were increased and showed favorable results clinically.
At the final follow-up, the mean dorsiflexion of the ankle was 10° and plantar flexion was 25°. Only one patient who developed nonunion of the operation site underwent an additional bone graft surgery.
In the radiological analysis, 12 patients, including 1 patient who underwent reoperation because of nonunion, exhibited perfect bone union at the final follow-up.
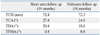
The mean talocalcaneal height increased from 66.7 mm (61.0 to 72.5) preoperatively to 73.1 mm (69.0 to 79.5) postoperatively and to 72.3 mm (55.0 to 78.5) at the final follow-up. The mean talocalcaneal angle increased from 22.2° (16.0 to 30.0) preoperatively to 29.2° (23.0 to 33.0) postoperatively and to 24.0° (15.0 to 33.0) at the final follow-up. The mean talar declination angle increased from 13.5° (7.0 to 19.0) preoperatively to 21.3° (16.0 to 32.0) postoperatively and to 18.6° (9.0 to 26.0) at the final follow-up. The mean talo-first metatarsal angle increased from 6.1° (-2.6 to 12.1) preoperatively to -1.3° (-12.1 to 5.3) postoperatively and to 0.8° (-5.2 to 12.5) at the final follow-up (Table 1).
These results indicated improvement in pre- to postoperative status and somewhat worsening at final follow-up. Nevertheless, statistical analysis showed significant improvement in preoperative to both postoperative and final follow-up results (p<0.05).
A 26-year-old man experienced a right intra-articular calcaneal fracture when he fell from some height, for which he underwent axial pinning as an initial operation. Although he had undergone conservative treatments because of persistent postoperative ankle pain, the symptoms were not relieved. He underwent subtalar distraction arthrodesis using a double bone-block 3 years and 7 months after the initial surgery.
After the surgery, a short leg cast was retained postoperatively for 5 weeks, and then, the patient started ROM exercise of the ankle and was allowed to bear weight gradually. At 10 weeks after surgery, full weight bearing was allowed after radiological subtalar joint union was obtained. Eleven months after surgery, the pinning was removed. At the final follow-up, 72 weeks after surgery, the arthrodesis was well maintained and deformity was corrected. Walking pain was also much better postoperatively. The patient's Ankle-Hindfoot score increased from 52 points (pain score 20 points) preoperatively to 90 points (pain score 40 points) postoperatively.
Subtalar arthrodesis is an effective surgical treatment for symptomatic subtalar arthritis due to calcaneal malunion after calcaneal fracture. This is often combined with decompression of the lateral wall to effectively relieve symptoms.16 Mostly, subtalar arthritis causes anatomical deformities, decreased calcaneal height, and so on. In such cases, in situ subtalar arthrodesis alone is not suitable for relieving these symptoms and can result in poor prognosis and limitations in functional aspects.17,18,19 Therefore, correction of deformities via arthrodesis has received attention.
In 1943, Gallie20 introduced subtalar distraction arthrodesis using a bone-block as a new solution for treating such deformity. The bone-block was harvested from the middle of the tibia in the affected site. In 1977, Kalamchi and Evans21 introduced a new way to get a bone-block from the lateral wall of the calcaneus, improving upon Gallie's method. This method can correct coronal sections, but not sagittal sections. In 1988, Carr, et al.4 introduced subtalar distraction arthrodesis using an iliac crest bone-block, and reported good results in 6 of 8 patients.
Calcaneal malunion patients with traumatic subtalar arthritis with anterior ankle impingement syndrome due to loss of hindfoot height and talar declination angle are commonly indicated for subtalar distraction arthrodesis.22,23 Many studies have reported favorable results for such patients (Table 2).1,6,7,11,13,15,16,24 Myerson and Quill7 suggested guidelines for subtalar distraction arthrodesis using a bone block: the indications for surgery included a loss of talo-calcaneal height more than 8 mm and radiologically proven anterior tibiotalar impingement because of an abnormal talar declination angle. Pain in the anterior aspect of the ankle was not prerequisite for this surgery.
Several operative techniques have been suggested with increasing research on subtalar bone block distraction. The posterolateral approach or the lateral extensile approach is one such technique. The goal of posterolateral Gallie incision is to restore the talo-calcaneal height and lateral talo-calcaneal angle.15,16,19,20,25,26,27,28,29 However, this approach cannot expose the lateral wall enough and it is difficult to operate on the calcaneocuboidal joint and impossible to approach peroneal tendon dislocation problems. Meanwhile, a lateral extensile approach is favorable for exposing the lateral wall and to correct alignment with insertion a bone block.29,30,31 Also, there is no significant difference in the correction of talo-calcaneal angle between the lateral extensile approach and Carr's way of surgery. In the present study, we experienced no complications with this procedure, such as a problem of wound repair after subtalar distraction, necrosis of the wound after surgery, and infection.
Generally, a tricortical bone-block from the iliac crest is usually used as a graft material. Most studies that have used an autograft have reported high rates of union, except for patients who smoke. Fresh frozen or lateral calcaneal wall grafts can also be utilized as graft materials. Studies have reported no complications of donor site pain or infection and the surgical time can be reduced when femoral head allograft materials are used. However, there are concerns for a lower rate of union, compared to an autograft, and loss of talo-calcaneal height may occur during follow-up. As well, allograft rejection or infection should also be considered.27,32
This study used a tricortical bone block from the iliac crest and a harvested double bone-block in the shape of a truncated wedge, which is wider than a single bone block. Considering the width of the surface of the subtalar joint, using a double bone-block can increase the rate of union because it can fix the surface of union more widely, compared to using single bone-block. It could also help to correct varus deformity by using different heights of bone-block and prevent the loss of talo-calcaneal height during follow-up.33 Since the height of grafted bone is determined by the height of sclerotic bone and subchondral bone removed intraoperatively, as well as preoperative measurements of the decreased talo-calcaneal height, a much higher bone-block may be needed than that determined preoperatively.
Screws are used for fixing a bone-block and the subtalar joint to limit movement of the subtalar joint. Mostly, 6.5 mm or larger cylindrical screws, which must bear a tremendous amount of force, that are either partially or fully threaded to obtain sufficient compression force and prevent collapse or subsidence of graft are used. Carr, et al.4 used a fully threaded 6.5 mm stainless-steel lag screw (core diameter 3.2 mm) and it was not enough to compress the union site of non-lag mode. If the screw's size and core diameter are small, bending force on the union site can be weak, causing damage of fixture or malunion. Clare, et al.30 suggested using a 7.3 or 8.0 titanium-alloy large-fragment cannulated screw to complement the problem. Titanium is fit for bone more than stainless steel, in the aspect of modulus of elasticity, and can reduce the chances of damage to internal fixture.30 Meanwhile, Pollard and Schuberth25 reported that partially threaded screws are favorable for bone graft because it fixes the location of bone-block and allows for compression from surrounding tissues. There are two ways to insert screws to complete this procedure: 1) two cannulated screws should be inserted toward talar dome from the posteroinferior calcaneal tuberosity,30 being careful not to break the bone-block during the procedure; and 2) an additional cannulated screw is inserted to put pressure on the anterior aspect of the subtalar joint.25 In this study, two 6.5 mm partially threaded titanium cannulated screws were fixed, considering the size of a typical Korean's calcaneus.
The mean rate of union in the present study was 96% (83 to 100) (Table 2).34 This was similar to 94% for in situ subtalar arthrodesis after calcaneal fracture35 and 97% for primary subtalar arthrodesis.36
Autologous bone is commonly used, but sometimes homologous bone can be used.16,27,37 Trnka, et al.16 noted 4 cases of nonunion among five cases of allograft, while other authors have reported union rates over 90%, even though they used the allograft bone.16,27,37 Chen, et al.13 reported satisfactory rates of union throughout sufficient decortication of cortical bone from the subtalar joint, removal of avascular bone, and cancellous bone graft. In this study, radiological bony union was achieved in all patients at an average of 6 months. One patient who showed nonunion at follow-up also achieved union after a reoperation with autogenous bone graft.
The AOFAS Ankle-Hindfoot scale (maximum 94 points) has been used for clinical evaluation of patients to compare and analyze pre- and postoperative results. Most patients typically show good results clinically, as well as increased scores after surgery, an average of 73 points (64-83) at final follow-up.34 In this study, scores increased from 43.3 preoperatively to 82.8 postoperatively. This result was similar to those in previous studies.
Radiological assessment of the talo-calcaneal height and talar declination angle is typically undertaken to evaluate improvement of hindfoot alignment in the sagittal plane. Our results of an increase in talo-calcaneal height after surgery, compared to that before surgery, was and a subsequent decrease at final follow-up is regarded as an outcome from weight-bearing and absorption of the bone-block. Myerson and Quill7 noted unfavorable results in seven of fourteen cases after operation by Carr's method, mainly attributed to loss of talo-calcaneal height due to absorption of bone-block. Chan and Alexander6 improved on Carr's method and grafted a double bone-block. After this procedure, the reported loss of talo-calcaneal height was only 1.4 mm. This was an excellent result in comparison to a reduction in the height of 4.7 mm when a single bone-block was used. Also, Garras, et al.27 have used autograft materials from the homologous femoral head allograft, while Zion, et al.38 have used a ramp cage made of carbon composite materials instead of a bone-block. Both studies reported satisfactory results. In this study, the loss of height was 0.7 mm in the short term (mean 19 months), as previously published.33 The loss of height was 0.8 mm and the decreased width was 0.1 mm at final follow-up. The results seemed favorable because there were seldom differences between the short-term and mid-term follow-up (Table 3).
Limited range of motion was unchanged or barely improved in our study, as in other studies. The average range of motion of ankle was in 10° of dorsiflexion and 25° of plantar flexion. This was unchanged and barely improved after surgery.
Degenerative changes in adjacent joints, usually a talonavicular joint or a calcaneocuboidal joint, are noted in 0 to 26%.30 Generally, additional surgery is not needed and all symptoms of degenerative changes are improved by conservative treatment.
Although patients are able to obtain satisfactory results, such as alleviation of symptoms and development of daily living skills (e.g., walking skills, return to work) after subtalar distraction arthrodesis, a number of complications have been reported as a result of the complexity of the procedure, problems of soft tissue, and so on. Postoperative complications such as wound infection, nonunion, sural nerve neuralgia, varus malunion, persistent heel pain due to implant extrusion, transposition and dislocation of a grafted bone-block, and damage of internal fixture have also been reported.1,4,6,7,14,39 After restoration of height by a bone-block in subtalar distraction arthrodesis, traction neuralgia can occur. Also, the sural and tibial nerves are also at risk for injury. A complex regional pain syndrome may occur or can worsen due to such injuries.15 In most studies, this depends on the severity of lateral calcaneal extrusion, and it is recommended that the lateral wall should be removed in order to reduce the width of the calcaneus and to decompress the peroneal tendon and the sural nerve.29
As described above, there is relatively well formulated indication of subtalar distraction arthrodesis. However, in terms of the number of bone block for distraction according to the type of calcaneal malunion, previous studies21,22 on the specific protocol are still lacking. Therefore, the purpose of this study was to provide useful, mid-term follow up results for developing better indications for surgery.
Subtalar distraction arthrodesis is an effective surgery for patients with various anatomical deformities, including subtalar arthritis and loss of talo-calcaneal height due to malunion after displaced intra-articular calcaneal fracture. As many studies have reported, satisfactory results were obtained from this surgery. The subtalar distraction arthrodesis using a double bone-block that we suggested led to excellent results for not only alleviation of pain but also functional recovery and restoration of the anatomical structures by correcting deformities. Accordingly, this procedure should be considered for patients with serious loss of talo-calcaneal height and severe pain due to subtalar arthritis.
Figures and Tables
Fig. 1
A, talo-calcaneal height; B, talo-calcaneal angle; C, talar declination angle; D, talo-1st metatarsal angle.
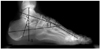
Fig. 2
Procedures of the operation. (A) Surgical approach for distraction arthrodesis. (B) Distraction and preparation of subtalar joint. (C) Insertion of two trapezoidal shaped tricortical bone blocks.

Fig. 4
Right foot-ankle lateral view & axial view (A) initial, (B) immediate postoperation, (C) postoperative 3 months, and (D) final follow-up (screw removal stage).
References
1. Amendola A, Lammens P. Subtalar arthrodesis using interposition iliac crest bone graft after calcaneal fracture. Foot Ankle Int. 1996; 17:608–614.

3. Buch BD, Myerson MS, Miller SD. Primary subtaler arthrodesis for the treatment of comminuted calcaneal fractures. Foot Ankle Int. 1996; 17:61–70.

4. Carr JB, Hansen ST, Benirschke SK. Subtalar distraction bone block fusion for late complications of os calcis fractures. Foot Ankle. 1988; 9:81–86.

5. Carr JB. Mechanism and pathoanatomy of the intraarticular calcaneal fracture. Clin Orthop Relat Res. 1993; 36–40.

6. Chan SC, Alexander IJ. Subtalar arthrodesis with interposition tricortical iliac crest graft for late pain and deformity after calcaneus fracture. Foot Ankle Int. 1997; 18:613–615.

7. Myerson M, Quill GE Jr. Late complications of fractures of the calcaneus. J Bone Joint Surg Am. 1993; 75:331–341.

8. Yoo CI, Eun IS, Jung YW. Subtalar distraction bone block arthrodesis (five cases). J Korean Foot Ankle Soc. 2004; 8:101–106.
9. Zwipp H, Tscherne H, Thermann H, Weber T. Osteosynthesis of displaced intraarticular fractures of the calcaneus. Results in 123 cases. Clin Orthop Relat Res. 1993; 76–86.
10. Chung HJ, Yum JK, Chung KJ, Jeon JM. Subtalar distraction arthrodesis for calcaneal malunion. J Korean Fract Soc. 2006; 19:34–40.

11. Burton DC, Olney BW, Horton GA. Late results of subtalar distraction fusion. Foot Ankle Int. 1998; 19:197–202.

12. Thompson KR, Friesen CM. Treatment of comminuted fractures of the calcaneus by primary triple arthrodesis. J Bone Joint Surg Am. 1959; 41-A:1423–1436.

13. Chen YJ, Huang TJ, Hsu KY, Hsu RW, Chen CW. Subtalar distractional realignment arthrodesis with wedge bone grafting and lateral decompression for calcaneal malunion. J Trauma. 1998; 45:729–737.

14. Kitaoka HB, Alexander IJ, Adelaar RS, Nunley JA, Myerson MS, Sanders M. Clinical rating systems for the ankle-hindfoot, midfoot, hallux, and lesser toes. Foot Ankle Int. 1994; 15:349–353.

15. Bednarz PA, Beals TC, Manoli A 2nd. Subtalar distraction bone block fusion: an assessment of outcome. Foot Ankle Int. 1997; 18:785–791.

16. Trnka HJ, Easley ME, Lam PW, Anderson CD, Schon LC, Myerson MS. Subtalar distraction bone block arthrodesis. J Bone Joint Surg Br. 2001; 83:849–854.

17. Kitaoka HB, Schaap EJ, Chao EY, An KN. Displaced intra-articular fractures of the calcaneus treated non-operatively. Clinical results and analysis of motion and ground-reaction and temporal forces. J Bone Joint Surg Am. 1994; 76:1531–1540.

18. Lance EM, Carey EJ, Wade PA. Fractures of the os calcis: a follow-up study. J Trauma. 1964; 4:15–56.
20. Gallie WE. Subastragalar arthrodesis in fractures of the os calcis. J Bone Joint Surg. 1943; 25:731–736.
21. Kalamchi A, Evans JG. Posterior subtalar fusion. A preliminary report on a modified Gallie's procedure. J Bone Joint Surg Br. 1977; 59:287–289.

22. Stephens HM, Sanders R. Calcaneal malunions: results of a prognostic computed tomography classification system. Foot Ankle Int. 1996; 17:395–401.

23. Zwipp H, Rammelt S. [Subtalar arthrodesis with calcaneal osteotomy]. Orthopade. 2006; 35:387–398. 400–404.
24. Marti RK, de Heus JA, Roolker W, Poolman RW, Besselaar PP. Subtalar arthrodesis with correction of deformity after fractures of the os calcis. J Bone Joint Surg Br. 1999; 81:611–616.

25. Pollard JD, Schuberth JM. Posterior bone block distraction arthrodesis of the subtalar joint: a review of 22 cases. J Foot Ankle Surg. 2008; 47:191–198.

26. Rammelt S, Grass R, Zawadski T, Biewener A, Zwipp H. Foot function after subtalar distraction bone-block arthrodesis. A prospective study. J Bone Joint Surg Br. 2004; 86:659–668.
27. Garras DN, Santangelo JR, Wang DW, Easley ME. Subtalar distraction arthrodesis using interpositional frozen structural allograft. Foot Ankle Int. 2008; 29:561–567.

28. Easley ME, Trnka HJ, Schon LC, Myerson MS. Isolated subtalar arthrodesis. J Bone Joint Surg Am. 2000; 82:613–624.

29. Baravarian B. Block distraction arthrodesis for the treatment of failed calcaneal fractures. Clin Podiatr Med Surg. 2004; 21:241–250.

30. Clare MP, Lee WE 3rd, Sanders RW. Intermediate to long-term results of a treatment protocol for calcaneal fracture malunions. J Bone Joint Surg Am. 2005; 87:963–973.

31. Flemister AS Jr, Infante AF, Sanders RW, Walling AK. Subtalar arthrodesis for complications of intra-articular calcaneal fractures. Foot Ankle Int. 2000; 21:392–399.

32. Myerson MS, Neufeld SK, Uribe J. Fresh-frozen structural allografts in the foot and ankle. J Bone Joint Surg Am. 2005; 87:113–120.

33. Chung HJ, Bae SY, Lee HS. Subtalar distraction two bone-block arthrodesis for calcaneal malunion. J Korean Foot Ankle Soc. 2009; 13:68–74.
34. Schepers T. The subtalar distraction bone block arthrodesis following the late complications of calcaneal fractures: a systematic review. Foot (Edinb). 2013; 23:39–44.

35. Schepers T, Kieboom BC, Bessems GH, Vogels LM, van Lieshout EM, Patka P. Subtalar versus triple arthrodesis after intra-articular calcaneal fractures. Strategies Trauma Limb Reconstr. 2010; 5:97–103.

36. Schepers T. The primary arthrodesis for severely comminuted intra-articular fractures of the calcaneus: a systematic review. Foot Ankle Surg. 2012; 18:84–88.

37. Lee MS, Tallerico V. Distraction arthrodesis of the subtalar joint using allogeneic bone graft: a review of 15 cases. J Foot Ankle Surg. 2010; 49:369–374.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download