Abstract
Schwannomas rarely present as intraocular tumors and are often misdiagnosed as malignant melanoma. We describe a choroidal schwannoma confirmed by sclerouvectomy.
A 30-year-old woman presented with a large nonpigmented intraocular mass of the choroid in the right eye and underwent surgical excision by sclerouvectomy. Histologically, the tumor was composed of a mixture of cellular solid components (Antoni A) and loose myxoid components (Antoni B). The tumor was eventually diagnosed as a schwannoma. Currently available ancillary studies are still of little value in definitively differentiating schwannomas from other choroidal tumors. In the case of atypical findings for a malignant melanoma, a benign neoplasm should be included in the differential diagnosis. This patient avoided enucleation by first having the mass excised. We are unaware of previous reports in which a choroidal schwannoma was diagnosed by surgical excision.
Schwannomas are encapsulated tumors consisting of a pure proliferation of Schwann cells. The cells in these tumors are characteristically arranged as either solid sheets of cells (Antoni A pattern) or as stellate-to-ovoid cells in a mucinous background (Antoni B pattern). Because these tumors are cytologically benign, they require treatment only to prevent visual loss resulting from their progressive enlargement. However, it is difficult to distinguish schwannomas from amelanotic malignant melanomas. We report a case in which we diagnosed a choroidal schwannoma by surgical excision.
A 30-year-old woman was referred to our clinic for evaluation of an intraocular mass lesion in her right eye. Her best corrected visual acuity was 30/50 in the right eye and 20/20 in the left eye. Intraocular pressures were within normal limits for both eyes at 17 mmHg. Her ophthalmoscopic history was unremarkable except for mild myopia. Although the anterior segment showed no pathologic findings, including the absence of an afferent pupillary defect, ophthalmoscopy revealed a 3×1×1 cm-sized nonpigmented choroidal mass with subretinal fluid in the superonasal quadrant of the fundus, extending from the equator to the ora serrata (Fig. 1). The other eye was unremarkable. The mass showed relatively medium internal reflectivity and contained a cystic portion on ultrasonography (Fig. 1). Magnetic resonance imaging (MRI) showed high signal intensity in T1-weighted images with enhancement and low signal intensity in T2-weighted images (Fig. 1). A PET (18-FDG) whole body scan was performed to rule out a metastatic lesion; the scan showed no remarkable FDG uptake. We subsequently decided to perform a fine needle aspiration biopsy of the lesion with a 25G pars plana vitrectomy. The cytology showed no malignant cells. Approximately 20% of cytological biopsy results can be errorneous due to inadequate selection of the aspiration site; therefore, we did not exclusively rule out choroidal melanoma. However, because of several atypical characteristics, including the presence of cystic portions and amelanotic nonpigmented lesions, and the relatively infrequent occurrence of malignant melanoma in Korea, our differential diagnosis contained benign masses such as schwannomas and leiomyomas. Although the patient's central vision was only mildly affected, the extent of subretinal fluid could have eventually involved the macula. We decided to surgically excise the lesion to obtain a definitive diagnosis and to prevent further visual deterioration. After lamellar scleral dissection, a complete choroidal mass excision was performed by sclerouvectomy. The gross specimen was approximately 3×1×1 cm in size and contained a cystic portion (Fig. 1). Interrupted sutures were places at the scleral flaps and cryotherapy was performed at the margins of excision. A small retinal defect was found in the superonasal quadrant. Trans pars plana vitrectomy and barrier endolaser photocoagulation were performed around the retinal defect. A silicone oil injection was also performed (Fig. 1). The patient's corrected vision was 20/100 at 4 months postoperatively.
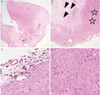
Light microscopy revealed that the tumor was composed of spindle cells with bland palisading nuclei in an Antoni A pattern. The findings were consistent with a schwannoma (Fig. 2).
Intraocular schwannomas are very rare, benign, peripheral nerve neoplasms that usually appear as solitary, amelanotic lesions of the ciliary body or choroid. Although schwannomas are cytologically benign, they may progressively enlarge at a rate similar to or greater than that of choroidal melanomas.1 Ophthalmoscopic, MRI, and ultrasonographic findings are not helpful in differentiating schwannomas from uveal melanomas.2 In two reported cases of anterior uveal schwannomas, the tumors were noted to transilluminate brightly.3,4 This may be a helpful clinical finding because it is unusual for anterior uveal melanomas to transilluminate in this way.
Most previously reported schwannoma cases have been diagnosed after enucleations performed because of the possibility of malignant melanoma.5,6 In some reported cases, early diagnosis was made using anterior chamber biopsy techniques for ciliary body masses.7 Other cases have utilized local block excision of ciliary body tumors to confirm the diagnosis of a schwannoma.8 However, it is not known if this can always be done to confirm the presence of a schwannoma.
As was illustrated in our case, it is difficult to differentiate between an amelanotic melanoma, metastatic carcinoma, a choroidal schwannoma, or a medulloepithelioma using ancillary techniques. Immunohistochemical staining techniques were not utilized in this case. When clinical features exist that are not typical of melanoma, such as the presence of cystic components or amelanotic nonpigmented lesions (amelanotic melanoma is very rare in Korea), we recommend performing an aspiration biopsy or even surgical excision to first rule out the presence of a benign neoplasm before performing enucleation.
Figures and Tables
Fig. 1
(A) Fundus photography of the superonasal quadrant of the right eye. Note the presence of a nonpigmented choroidal mass with serous fluid. (B) Ultrasonogram showing a choroidal mass containing a cystic component and demonstrating medium reflectivity. (C) MRI (magnetic resonance imaging) showing low signal intensity in T2-weighted images. (D) Signal intensity in T1-weighted images showing marked enhancement. (E) Gross specimen approximately 3×1×1 cm in size with a cystic component. (F) Postoperative fundus photography.

Fig. 2
(A) A well circumscribed mass with multifocal cystic changes (H-E, ×12). (B) The mass shows alternating hypercellular (Antoni A: stars) and hypocellular (Antoni B: arrows) areas (H-E ×40). (C) The periphery of the mass shows melanin-containing cells. The mass seems to arise from the choroid membrane (H-E ×200). (D) The hypercellular area shows bland spindle cells with whorling patterns (×200). These histologic features are consistent with a schwannoma.
References
1. Shields JA, Sanborn GE, Kurz GH, et al. Benign peripheral nerve tumor of the choroid : a clinicopathologic correlation and review of the literature. Ophthalmology. 1981. 88:1322–1329.
2. Fan JT, Campbell RJ, Robertson DM. A survey of intraocular schwannoma with a case report. Can J Ophthalmol. 1995. 30:37–41.
3. Hufnagel TJ, Sears ML, Shapiro M, Kim JH. Ciliary body neurilemoma recurring after 15 years. Graefes Arch Clin Exp Ophthalmol. 1988. 226:443–446.
4. Smith PA, Damato BE, Ko MK, Lyness RW. Anterior uveal neurilemmoma: a rare neoplasm simulating malignant melanoma. Br J Ophthalmol. 1987. 71:34–40.
5. Matsuo T, Notohara K. Choroidal schwannoma: immunohistochemical and electron-microscopic study. Ophthalmologica. 2000. 214:156–160.
6. Lee SH, Hong JS, Choi JH. Choroidal schwannoma. Acta Ophthalmol Scand. 2005. 83:754–756.
7. Pineda R 2nd, Urban RC Jr, Bellows AR, Jakbiec FA. Ciliary body neurilemoma. Unusual clinical findings intimating the diagnosis. Ophthalmology. 1995. 102:918–923.
8. Kuchle M, Holbach L, Schlotzer-Schrehardt U, Naumann GO. Schwannoma of the ciliary body treated by block excision. Br J Ophthalmol. 1994. 78:397–400.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download