The iris is connected to the sphincter and dilator muscles of the eye, which automatically change the size of the pupil depending on the amount of light available to the eye and the position of the eye. In addition, the iris is in the most anterior portion of the uvea and contains abundant vascular networks.1 It forms a delicate and movable diaphragm between the anterior and the posterior chambers.2,3
The iris has abundant vasculature, and disruption of the blood-aqueous barrier induces iritis. Melanocytes and fibroblasts are present in the iris stroma, and the pigmented epithelium is on the posterior side of the iris. In fluorescein iris angiography, fluorescein dye cannot penetrate the iris vessel wall because of the blood-iris barrier; nonetheless, in the ciliary body fluorescein dye penetrates the ciliary vessel wall. The leakage of fluorescein dye cannot be detected in the iris vessel of a normal eye under the age of 40 years. However, there is often fluorescein leakage at the pupillary margins in people older than 40 years, especially after 50 years of age.4-6
Iris vasculature has abundant blood flow and plays an important role in iritis. Thus, studies on the iris vascular network have been previously conducted. However, most anatomical studies on the human iris vascular network have been performed in vivo with fluorescein iris angiography.4,7,8 Other studies have been conducted in vitro and were performed with scanning electron microscopy after the injection of resin into the human iris vascular network.9-13
This study was conducted in order to assess the human iris vascular network as closely as possible to its normal state. Applying a flat preparation, the iris vascular network was examined by fluorescent and light microscopies.
Materials and Methods
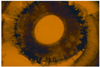
Human cadaver eyes were obtained from neonates (under one year of age), which have relatively low amounts of pigment granules in the uveas. No external malformation were found on gross examination. Each eyeball was physically divided into two parts at the equator, and the crystalline lens was removed. In the anterior portion of the eyeball, the ciliary body was carefully removed from the sclera by dissection with microforceps. Then the iris was separated from the ciliary body at the iris root (Fig. 1).
Pigment granules of the uvea make microscopic examination of the iris vascular network difficult. To remove the pigment granules from the dissected irises, the specimens were treated with trypsin using the method of Kuwabara and Cogan.14 The tissues were treated with 0.1 M Tris buffer (pH 7.8) containing 3% trypsin (1 : 250) and were placed in a 36℃ incubator for 30 minutes. After incubation, the pigment epithelium and melanocytes were partially removed from the iris surface with a fine brush.
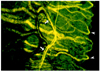
The partially depigmented irises were spread onto glass slides and dried at room temperature. Dehemoglobinized red blood cells within the blood vessels of the iris show pseudofluorescence;15 thus, it is possible to identify the shape of the blood vessels under fluorescent microscopy. The slides in this study were examined under a fluorescent microscope with a fluorescein isothiocyanate filter (450 to 500 nm).
The irises of the remaining eyeballs which were not treated with trypsin solution were spread onto glass slides, dried at room temperature, and stained with hematoxylin-eosin. Then the slides were examined under a light microscope.
Results
The ciliary body and iris were dissected from the sclera and were separated at the iris root (Fig. 1).
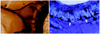
The long posterior ciliary artery (LPCA) branches in the sclera toward the ciliary body to form a V shape, travels to the inside of the iris, and forms a major arterial circle of the iris near the iris root (Fig. 2A). From the major arterial circle of the iris, the iris artery travels to the pupillary margin at a constant interval (Fig. 2B).
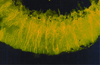
From the iris root to the pupillary margin, the iris vascular network is composed of iris arteries, veins, and capillaries in a relatively linear pattern (Fig. 3). Near the iris root, large vessels with an irregular course were seen, most likely veins (Fig. 3).
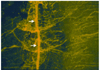
The diameters of the major arterial circle of the irises were variable. A relatively small sized vessel, a part of the major arterial circle of the iris, was observed near the iris root (Fig. 4). Relatively large sized iris vessels were seen around the ciliary processes (Fig. 5).
The iris vascular network in the pupillary margin forms a cone shape and then forms an arcade by connecting to adjacent vascular networks (Figs. 6, 7, 8, 9). The capillaries continue to the iris vein from the arcade. The minor arterial circle of the iris travels perpendicular to the arcade of the vascular network of the pupillary margin with a variable diameter.
Discussion
In this study, the ciliary body and the iris were separated during preparation of the iris. Therefore, the contribution of the anterior ciliary artery (ACA) to the formation of the major arterial circle of iris could not be assessed. However, it was observed that the LPCA that travels from the ciliary body to the pupil was branched into a V shape and formed the major arterial circle of the iris near the iris root.
The ACA flows mostly to the anterior uvea. It travels in parallel to the rectus muscles, penetrates the sclera, and forms intramuscular loops by generating many branches in the external layer of the ciliary muscles. It also forms the major arterial circle of the iris together with the LPCA, which is the major blood supplier to the iris and the ciliary body.16
Hayreh et al.6 have reported that the temporal branches of the ACA and LPCA have less influence on the blood supply to the temporal portion of the iris than do the nasal, superior, and inferior portions, based on fluorescein iris angiography taken after strabismus surgery. Funk and Rohen10 have reported that the ACA and LPCA are connected in almost all areas of the human postmortem eyeball. Nevertheless, the results of vascular casting performed on these blood vessels selectively showed that most of the area of the major arterial circle of the iris was supplied from a branch of the LPCA.
In the current study, the iris artery was observed to travel from the major arterial circle of the iris toward the pupillary margin with a regular interval and diameter. Conversely, Shimizu and Ujiie17 have reported that the iris artery has a regular diameter and interval, and that it shows a difference in shape from the blood vessels of the ciliary process. The veins and capillaries of the ciliary processes are large and irregularly dilated and therefore have a sinusoid appearance. The minor arterial circle of the iris was located in the pupillary constrictor muscle and was observed to travel perpendicularly to the arcade of the vascular network of the iris with diverse diameters. This minor arterial circle of the iris is formed by a branch from the iris artery traveling from the iris root to the pupil. The branches from the minor arterial circle of the iris travel to the pupillary margin and form the capillary arcade. However, according the Shimizu and Ujiie,17 blood vessels comprising the minor arterial circle of the iris were detected intermittently and reached only a few hundred micrometers, and thus, did not form a complete circle. In our study, the minor arterial circle of the iris was also observed to not form a continuous circle.
The iris vein ran on a path similar to that of the artery, but as it got closer to the iris root, the vein's diameter became larger and thus could be distinguished from the iris artery.
In fluorescein iris angiography, during the arterial phase, fluorescein first fills the nasal side, and then fills the temporal side.8 A possible explanation of this finding was reported by Amalric and Rebiere18 who explained that the preferential filling was due to the distribution of blood vessels being most dense in the superior-nasal sector. In addition, Hayreh and Scott8 showed that blood vessels were evenly distributed in all areas, but in some eyeballs the blood vessels might be more densely distributed in the nasal side.
Fluorescein iris angiography often shows sectoral filling patterns. Hayreh and Scott8 reported that such sectoral filling is physiological and is most probably due to the fact that the various supply arteries to the iris arise at different points along the ophthalmic artery and show a large amount of variation from eye to eye.
In our study, the distribution of blood vessels was observed to be similar in each area of the iris. Several branches of the LPCA showed a V-shape prior to entering the iris root, and they formed the major arterial circle of the iris. Based on these findings, it is likely that sectoral filling in fluorescein angiography is due to the difference in time that it takes for fluorescein to fill all of the vessels. First, the iris arteries that continue to the branches of the two LPCA are filled. After that, fluorescein fills the major arterial circle of the iris and the connected iris arteries. Such a finding is in disagreement with the observations of Amalric and Rebiere,18 and Hayreh and Scott6 In addition, the variation in diameter of the major arterial circles of the iris may explain the time difference in fluorescein filling from the major arterial circle of the iris to the iris artery.
In our study, iris capillaries were observed distinctly in the pupillary margin, which is in agreement with the observation of Hayreh and Scott6 that neovascularization occurs first in this area as rubeosis of the iris. In addition, physiologic fluorescein leakage in a normal eye after the age of 50 years occurs due to the loosening of the tight junction due to aging. It is believed that blood vessels in this area are the terminal vessels, vesseas capillaries, and are vulnercape to agingseascesses. The abundant arterial vascular network in the pupillary constrictor muscle implies active nutritional support and metabolism in this area and is considered to be associated with hippus.
Because our study used flat preparation, as opposed to vascular casting which allows observation of blood vessels in three dimensions, the distribution of blood vessels could not be evaluated by distinguishing the anterior and posterior parts.
In vascular casting, resin is injected into the blood vessels, the remaining tissues are enzymatically removed, and the frame is examined three-dimensionally with a scanning electronelectron microscope.9-13 In our study, the shapes of the iris blood vessels were examined without removing the vascular tissues. Observation of the iris blood vessels under microscopy is made difficult by pigment epithelium and pigment granules of melanocytes. We treated the tissues with trypsin, an established method for removal of retinal pigments. Importantly, since dehemoglobulinized red blood cells show psuedofluorescence we were able to use fluorescein microscopy to observe the iris vascular network, providing a new view of this system.
Through anatomical observation of the iris vascular network, this study provides a theoretical basis for the sectoral filling of fluorescein in iris angiography.




 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download