Abstract
Cow's milk is one of the most common food allergens in children with atopic dermatitis (AD). This study was conducted to describe the natural course of cow's milk allergy in children with AD, and to identify factors predictive of outcome. To accomplish this, we reviewed the medical records of 115 children who were diagnosed with AD and cow's milk allergy before 24 months of age to evaluate their clinical characteristics and prognostic factors. During a follow-up period of 24 to114 months, the median age for tolerance to cow's milk was found to be 67 months. Multivariate analysis using the Cox proportional hazard model revealed that the peak cow's milk-specific IgE level within 24 months after birth was the most important factor for prediction of the outcome of cow's milk allergy. In conclusion, half of the children younger than 24 months of age with AD and cow's milk allergy could tolerate cow's milk at 67 months of age. The peak cow's milk-specific IgE level within the first 24 months of birth is useful to predict the prognosis of cow's milk allergy in children with AD.
Atopic dermatitis (AD), which is a common allergic disease that often develops during infancy, is a chronic inflammatory skin disease that occurs concurrently with severe itching. According to a cohort study conducted in Britain, the prevalence of AD in children born in 1946, 1958, and 1970 continuously increased, being 5.1%, 7.3%, and 12.2%, respectively (1). Surveys of allergic diseases in school age children conducted in 1979 and 1991 in Sweden also showed that the prevalence of AD increased from 7.05 to 18.25% (2). Moreover, according to the results of the International Study of Asthma and Allergies in Children (ISAAC) Phase One and Three, AD is increasing worldwide (3). When reviewing the results of an epidemiological study conducted by the Korean Academy of Pediatric Allergy and Respiratory Disease (KAPARD) in 2000, the domestic prevalence of AD was 24.9% in elementary school students and 12.8% in middle school students, which increased from values reported in 1995 (4). Another study showed that the prevalence of AD in elementary school students was 33.9% in Ilsan in 2005 (5). According to a recent study, the prevalence of AD in children in Korea was 28.9% in 2006 based on questionnaires (6).
AD is often associated with food allergy (7-9), and some studies have reported that 37% of patients have AD (8). Cow's milk allergy is a relatively common disease that occurs in 2% to 3% of infants (10), and 1/3 of patients with AD have cow's milk allergy (11). Conversely, 40% to 50% of cow's milk allergic patients less than one year of age have been diagnosed with AD (11). The prognosis of cow's milk allergy is relatively good. Host reported that cow's milk allergy spontaneously disappeared in 50%, 70%, and 85% of 1, 2, and 3 yr-old children, respectively (12). However, these results differed depending on geographic region, race, and diagnostic criteria (13, 14).
In Korea, the prevalence of cow's milk allergy in patients with AD is reportedly 4.5%; however, this was based on the results of a study conducted at a single institution (15). In addition, no studies of the natural course of cow's milk allergy in Korea have been conducted to date.
Therefore, this study was conducted to determine the natural course of cow's milk allergy in Korean children with AD and analyzed prognostic factors that affected the outcome of cow's milk allergy.
Of the patients who visited the Samsung Medical Center Allergy Clinic between January 2000 and May 2008, 115 children, diagnosed with both AD and cow's milk allergy within the first 24 months of birth, were included in this study. The patients were followed for at least 24 months in the outpatient clinic. AD was diagnosed according to the criteria described by Hanifin and Rajka (16). Those with a convincing history of adverse reaction within two hours of a single ingestion of cow's milk and with serum cow's milk-specific IgE levels higher than 0.35 kU/L were considered to have cow's milk allergy. Adverse reactions included skin rash, urticaria, angioedema, diarrhea, vomiting, coughing, wheezing or breathing difficulty. When the cow's milk-specific IgE level was 5 kU/L or higher, the patients were also diagnosed with cow's milk allergy according to the 95% positive predictive value diagnostic criteria (17, 18), even if the clinical symptoms were vague or uncertain. Cow's milk-specific IgE testing was conducted using the immunoCAP (Pharmacia, Uppsala, Sweden) system. When the cow's milk-specific IgE level was 100 kU/L or higher, the value was reported as 101 kU/L.
The medical records of 115 patients were retrospectively reviewed for gender, age at AD occurrence, family history of allergic disease, duration of breastfeeding, restriction of milk by mothers during lactation prior to the diagnosis of cow's milk allergy, age at the introduction of solid food, serum total IgE and cow's milk-specific IgE level at the first visit, peak serum total IgE and cow's milk-specific IgE during the first 24 months after birth to identify prognostic factors associated with the resolution time for cow's milk allergy.
Cow's milk ingestion was strictly restricted once patients were diagnosed with cow's milk allergy. Mothers of breastfed patients avoided to cow's milk and its products, and formula fed patients received extensively hydrolyzed formula. The patients were asked to visit the hospital regularly for clinical evaluation and blood testing to determine cow's milk-specific IgE and total IgE level at least once a year. The development of tolerance to cow's milk was confirmed by either an open food challenge test conducted in the hospital or based on a medical history of no specific symptoms after ingesting milk at home. Patients who had persistent cow's milk allergy until the last visit and were not followed up for more than one year underwent a telephone survey to determine the cow's milk allergy resolution time.
SAS 9.2 (SAS institute, Inc., Cary, NC, USA) and SPSS 18 (SPSS Inc., Chicago, IL, USA) were used for the statistical analysis. To investigate the natural course of cow's milk allergy, an accumulative survival curve was drawn using the Kaplan-Meier method, and prognostic factors associated with cow's milk allergy resolution time were analyzed. The Cox proportional hazard model was used to analyze the impact of univariate and multivariate variables. In addition, standardized coefficients calculated by logistic regression analysis were used to analyze the most influential factors associated with cow's milk allergy resolution. To determine the trend in the cow's milk-specific IgE level by age, the trend line with the highest value of adjusted R2 was used in regression analysis. A P value < 0.05 was considered statistically significant.
The 115 patients enrolled in this study consisted of 38 girls (33.0%) and 77 boys (67.0%). The mean duration of follow-up was 47.0 ± 20.4 months (range 24-114 months). Eighty-three patients (72.2%) were followed up as outpatients. Thirty-two patients had persistent cow's milk allergy until the last visit and were not followed up for more than one year, and 22 of these patients underwent a telephone survey to determine the development of tolerance to cow's milk. The remaining ten patients were lost. Of the 115 patients, 72 patients (62.6%) were diagnosed with cow's milk allergy based on a convincing history and positive cow's milk-specific IgE, and 43 patients (37.4%) were diagnosed based on serum cow's milk-specific IgE levels of 5 kU/L or higher. The most common symptoms of cow's milk allergy were skin rash, urticaria, and angioedema, and these were followed by gastrointestinal symptoms including vomiting and diarrhea, and respiratory symptoms such as coughing, wheezing, and breathing difficulty. Some patients experienced combinations rather than single symptom, such as concomitant skin, gastrointestinal and respiratory symptoms.
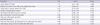
The clinical characteristics of the study subjects are summarized in Table 1. Fifty-one patients (44.3%) were cow's milk restricted by mothers during lactation prior to the diagnosis of cow's milk allergy. Fifty-seven patients (49.6%) had at least one family member who had AD, asthma or allergic rhinitis. The average age at AD diagnosis was 3.1 ± 2.0 months and the average age at introduction of solid food was 6.6 ± 1.8 months. The serum cow's milk-specific IgE and total IgE levels at the first visit were 24.5 ± 33.0 kU/L and 1,057.8 ± 2,167.0 kU/L, respectively. The peak serum cow's milk-specific IgE and total IgE during the first 24 months after birth were 37.2 ± 37.1 kU/L and 1,727.3 ± 3,046.2 kU/L, respectively.
Cow's milk allergy resolved in 47 patients (40.9%) during the follow-up period, and cow's milk tolerance was confirmed in seven of these patients via an open food challenge test in the hospital and in 40 patients by reintroduction of cow's milk at home. The cow's milk-specific IgE level at the time of tolerance was 2.0 ± 2.2 kU/L, respectively.
The Kaplan-Meier curve representing the spontaneous resolution of cow's milk allergy in patients with AD within the first 24 months after birth is presented in Fig. 1. The median age of cow's milk allergy resolution was determined to be 67 months based on the curve. Cow's milk allergy spontaneously resolved in 9.6%, 25.7%, 37.6%, and 43.3% of the patients at 24, 36, 48, and 60 months after birth, respectively.
Factors affecting the development of tolerance to cow's milk are displayed in Table 2. Family history of allergy, cow's milk-specific IgE at the first visit, and the peak serum total IgE and cow's milk-specific IgE during the first 24 months after birth significantly influenced the spontaneous resolution of cow's milk allergy in univariate analysis. Gender, age at diagnosis of AD, duration of breastfeeding, restriction of milk by mothers during lactation prior to the diagnosis of cow's milk allergy, age at introduction of solid food, and the serum total IgE at the first visit were irrelevant.
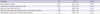
The results of multivariable analysis of the factors affecting the development of tolerance to cow's milk are shown in Table 3. The results showed that family history of allergic disease was significant and that the probability of persistent allergy to cow's milk was higher in patients without a family history of allergic disease than in patients with a family history of allergic disease (HR, 0.41; 95% CI, 0.22-0.78). Furthermore, the probability of developing tolerance to cow's milk decreased as the peak cow's milk-specific IgE during the first 24 months after birth increased (HR, 0.96; 95% CI, 0.93-1.00). As the peak cow's milk-specific IgE increased by 1 kU/L during the first 24 months after birth, the hazard ratio became 0.96, leading to a reduced probability for cow's milk allergy resolution. Logistic regression analysis was conducted to identify individual factors that were important to the resolution of cow's milk allergy. As shown in Table 4, the absolute value of standardized estimates of the peak cow's milk-specific IgE during the first 24 months after birth was the highest; therefore, the peak cow's milk-specific IgE during the first 24 months after birth was shown to be the most important factor for prediction of the development of cow's milk allergy tolerance.
We attempted to investigate the relevance of developing tolerance to cow's milk to cow's milk-specific IgE. To accomplish this, the patients were divided into two groups, each with cow's milk-specific IgE levels greater or less than 15 kU/L during the first 24 months after birth. The groups were then analyzed using a tolerance survival curve (Fig. 2). When the peak cow's milk-specific IgE values were less than 15 kU/L, cow's milk allergy spontaneously resolved in 21.2%, 46.4%, 61.3%, and 73.9% of the patients at 24, 36, 48, and 60 months after birth, respectively. For peak cow's milk-specific IgE levels of 15 kU/L or higher, no spontaneous resolution of cow's milk allergy was observed in any patient at 24 months after birth. Cow's milk allergy disappeared in 11.5% and 19.1% of the patients at 36 and 48 months, respectively. The spontaneous resolution of cow's milk allergy at 60 months was similar to that at 48 months. Therefore, tolerance to cow's milk developed more rapidly when the highest cow's milk-specific IgE values during the first 24 months after birth were low.
The trend in changes in cow's milk-specific IgE with age was investigated in patients who developed tolerance to cow's milk with persistent cow's milk allergy (Fig. 3). The serum level of cow's milk-specific IgE was shown to decrease as the age at which patients developed tolerance to cow's milk allergy increased. In contrast, the level of cow's milk-specific IgE was shown to increase and remain high as the age of the patients who had persistent cow's milk allergy increased.
In this study, we analyzed the natural course of cow's milk allergy with AD in Korean children via a survival curve. We found that cow's milk-specific IgE levels at 2 yr of age could be used to predict the development of tolerance to cow's milk. Specifically, the results of our study showed that half of the patients with cow's milk allergy tolerated cow's milk at 67 months of age. The development of tolerance to cow's milk appears to be slow when compared with previous studies (12, 13). In one study, the spontaneous resolution rate was 50%, 70%, and 85% in the one-, two- and three-year age groups, respectively (12). In that study, about 50% to 70% of the patients had cutaneous symptoms, while 50% to 60% had gastrointestinal symptoms, and 20% to 30% had respiratory symptoms. Another study showed that the spontaneous resolution rate was 56% in the four-year age group and 78% in the six-year age group (13), in which only 21% of the study population had atopic eczema. In contrast, cow's milk allergy in children with AD was reported to be spontaneously resolved in 50% of patients at 7 yr and 11 months after birth (14). In a recent study in the United States, IgE-mediated cow's milk allergy was found to be spontaneously resolved in 19%, 42%, 64%, and 79% of patients by 4, 8, 12, and 16 yr, respectively (19). Of these patients, 71% had eczema, 49% had asthma, and 40% had allergic rhinitis. These differences in resolution rate may have been due, at least in part, to different characteristics of the study population and different inclusion criteria in each study. All patients in the present study had AD, which was not the case in the aforementioned studies. In addition, race, geographic region and genetic background are also likely to have influenced the results.
We found that cow's milk-specific IgE during the first 24 months after birth is highly predictive of cow's milk allergy outcome. The diagnostic levels of cow's milk-specific IgE differed by 2 yr of age. Specifically, after 2 yr of age, 15 kU/L had a positive predictive value of 95% (17, 18). Therefore, we divided our patients into two groups based on 15 kU/L. For patients with a peak cow's milk-specific IgE less than 15 kU/L, cow's milk allergy spontaneously resolved in 73.9% of the patients at 60 months of age, while the spontaneous resolution rate was only 19.1% at 60 months for the children with the peak cow's milk-specific IgE levels of 15 kU/L or higher. Similar findings were reported in previous studies regarding the usefulness of cow's milk-specific IgE level as a prognostic factor (19, 20). Based on the results of the present study, the cow's milk-specific IgE levels in patients with cow's milk allergy need to be followed until 2 yr of age. Physicians should also counsel families about the prognosis of cow's milk allergy and work on better patient compliance.
In this study, the change in cow's milk-specific IgE was analyzed depending on development of tolerance to cow's milk. As a result, cow's milk-specific IgE was shown to gradually decrease as the age of patients that tolerated cow's milk increased. In contrast, cow's milk-specific IgE was shown to increase and maintain levels as the age of patients with persistent cow's milk allergy increased. These findings were consistent with those of a study conducted by Skripak et al. (19), in which a different trend in IgE level over time was shown between the group with tolerance and the group with persistent cow's milk allergy. These findings are also likely to be helpful for clinicians to analyze test results and explain the prognosis of cow's milk allergy.
It should be noted that this study has some limitations. First, double-blind, placebo-controlled food challenge test (DBPCFC), the gold standard for the diagnosis of food allergy, was not performed to confirm cow's milk allergy. Instead, we used a convincing history plus positive cow's milk-specific IgE for diagnosis. However, 37.4% of the participants in this study were diagnosed with cow's milk allergy because the serum level of cow's milk-specific IgE was over the 95% positive predictive value. Second, this was not a prospective study. Rather, we retrospectively reviewed medical records and had to rely on parental reports obtained via telephone interviews to determine the outcome of cow's milk allergy. Third, the follow-up duration was not very long, although the mean duration was 47 months. Some patients in our study may have outgrown cow's milk allergy if they were followed for a longer period. Fourth, the presence of other food allergies and severity of atopic dermatitis were not considered.
In conclusion, half of the patients with cow's milk allergy with AD tolerated cow's milk at 67 months of age. The results of this study suggest that the peak cow's milk-specific IgE level during the first 24 months of life is the most important factor for prediction of the prognosis of cow's milk allergy. The tolerance to cow's milk develops as the serum level of cow's milk-specific IgE decreases with age. Regular follow-up with testing for cow's milk-specific IgE would be helpful for predicting the appropriate timing of re-introduction of cow's milk to the diet.
Figures and Tables
Fig. 1
Development of tolerance to cow's milk. Kaplan-Meier survival curve shows cow's milk allergy resolution over time in children with atopic dermatitis.
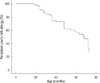
Fig. 2
Development of tolerance to cow's milk according to peak cow's milk-specific IgE level during the first 24 months after birth. (—) Solid line shows tolerance to cow's milk by patients with peak cow's milk-specific IgE levels during the first 24 months after birth of less than 15 kU/L. (---) Dotted line shows tolerance to cow's milk by patients with peak cow's milk-specific IgE levels during the first 24 months after birth of 15 kU/L or more.

Fig. 3
Trend in cow's milk-specific IgE levels over time based on final cow's milk allergy status. Each dot represents all cow's milk-specific IgE levels recorded by age. (A) All values in the group with tolerance of cow's milk allergy. (B) All values in the group with persistence of cow's milk allergy.

AUTHOR SUMMARY
Natural Course of Cow's Milk Allergy in Children with Atopic Dermatitis
Jungmin Suh, Hyeonyoung Lee, Jung Hyun Lee, Joongbum Cho, Jung-Seok Yu, Jihyun Kim, Youngshin Han, Kangmo Ahn and Sang-Il Lee
Cow's milk is one of the most common foods to cause allergy in children with atopic dermatitis (AD). We investigated the natural course of cow's milk allergy in children with atopic dermatitis, and to identify factors predictive of outcome. Multivariate analysis by Cox proportional hazard model revealed that family history of allergic diseases and peak cow's milk-specific IgE level during 24 months after birth were prognostic factors.
References
1. Taylor B, Wadsworth J, Wadsworth M, Peckham C. Changes in the reported prevalence of childhood eczema since the 1939-45 war. Lancet. 1984. 2:1255–1257.
2. Aberg N, Hesselmar B, Aberg B, Eriksson B. Increase of asthma, allergic rhinitis and eczema in Swedish schoolchildren between 1979 and 1991. Clin Exp Allergy. 1995. 25:815–819.
3. Asher MI, Montefort S, Björkstén B, Lai CK, Strachan DP, Weiland SK, Williams H. Worldwide time trends in the prevalence of symptoms of asthma, allergic rhinoconjunctivitis, and eczema in childhood: ISAAC Phases One and Three Repeat Multicountry Cross-Sectional Surveys. Lancet. 2006. 368:733–743.
4. Hong SJ, Ahn KM, Lee SY, Kim KE. The prevalence of asthma and allergic diseases in Korean children. Pediatr Allergy Respir Dis. 2008. 18:15–25.
5. Son KY, Park KS, Hwang HH, Yun BS, Lee SJ, Kim MA, Park JY, Kim KE, Jang KC. Prevalence of allergic diseases among primary school children in Ilsan, Gyeonggi and Changes of symptoms after environmental control in 2005. Pediatr Allergy Respir Dis. 2007. 17:384–393.
6. Jee HM, Kim KW, Kim CS, Sohn MH, Shin DC, Kim KE. Prevalence of asthma, rhinitis and eczema in Korean children using the international study of asthma and allergies in childhood (ISAAC) questionnaires. Pediatr Allergy Respir Dis. 2009. 19:165–172.
7. Sampson HA, McCaskill CC. Food hypersensitivity and atopic dermatitis: evaluation of 113 patients. J Pediatr. 1985. 107:669–675.
8. Eigenmann PA, Sicherer SH, Borkowski TA, Cohen BA, Sampson HA. Prevalence of IgE-mediated food allergy among children with atopic dermatitis. Pediatrics. 1998. 101:E8.
9. Eigenmann PA, Calza AM. Diagnosis of IgE-mediated food allergy among Swiss children with atopic dermatitis. Pediatr Allergy Immunol. 2000. 11:95–100.
10. Høst A. Frequency of cow's milk allergy in childhood. Ann Allergy Asthma Immunol. 2002. 89:6 Suppl 1. 33–37.
11. Novembre E, Vierucci A. Milk allergy/intolerance and atopic dermatitis in infancy and childhood. Allergy. 2001. 56:Suppl 67. 105–108.
12. Høst A. Cow's milk protein allergy and intolerance in infancy: some clinical, epidemiological and immunological aspects. Pediatr Allergy Immunol. 1994. 5:5 Suppl. 1–36.
13. Bishop JM, Hill DJ, Hosking CS. Natural history of cow milk allergy: clinical outcome. J Pediatr. 1990. 116:862–867.
14. Cantani A, Micera M. Natural history of cow's milk allergy: an eight-year follow-up study in 115 atopic children. Eur Rev Med Pharmacol Sci. 2004. 8:153–164.
15. Han DK, Kim MK, Yoo JE, Choi SY, Kwon BC, Sohn MH, Kim KE, Lee SY. Food sensitization in infants and young children with atopic dermatitis. Yonsei Med J. 2004. 45:803–809.
16. Hanifin JM, Rajka G. Diagnostic features of atopic dermatitis. Acta Derm Venereol (Stockh). 1980. 92. 44–47.
17. Sicherer SH, Sampson HA. 9. Food allergy. J Allergy Clin Immunol. 2006. 117:S470–S475.
18. García-Ara C, Boyano-Martínez T, Díaz-Pena JM, Martín-Muñoz F, Reche-Frutos M, Martín-Esteban M. Specific IgE levels in the diagnosis of immediate hypersensitivity to cows' milk protein in the infant. J Allergy Clin Immunol. 2001. 107:185–190.
19. Skripak JM, Matsui EC, Mudd K, Wood RA. The natural history of IgE-mediated cows' milk allergy. J Allergy Clin Immunol. 2007. 120:1172–1177.
20. Vassilopoulou E, Konstantinou G, Kassimos D, Douladiris N, Xepapadaki P, Manoussakis E, Saxoni-Papageorgiou P, Papadopoulos NG. Reintroduction of cows' milk in milk-allergic children: safety and risk factors. Int Arch Allergy Immunol. 2008. 146:156–161.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download