This article has been corrected. See "Erratum: Figure Correction" in Volume 26 on page 1531.
Abstract
Early differentiation between bacterial infections and disease flares in autoimmune disease patients is important due to different treatments. Seventy-nine autoimmune disease patients with symptoms suggestive of infections or disease flares were collected by retrospective chart review. The patients were later classified into two groups, disease flare and infection. C-reactive protein (CRP) and serum procalcitonin (PCT) levels were measured. The CRP and PCT levels were higher in the infection group than the disease flare group (CRP,11.96 mg/dL ± 9.60 vs 6.42 mg/dL ± 7.01, P = 0.003; PCT, 2.44 ng/mL ± 6.55 vs 0.09 ng/mL ± 0.09, P < 0.001). The area under the ROC curve (AUC; 95% confidence interval) for CRP and PCT was 0.70 (0.58-0.82) and 0.84 (0.75-0.93), which showed a significant difference (P < 0.05). The predicted AUC for the CRP and PCT levels combined was 0.83, which was not significantly different compared to the PCT level alone (P = 0.80). The best cut-off value for CRP was 7.18 mg/dL, with a sensitivity of 71.9% and a specificity of 68.1%. The best cut-off value for PCT was 0.09 ng/mL, with a sensitivity of 81.3% and a specificity of 78.7%. The PCT level had better sensitivity and specificity compared to the CRP level in distinguishing between bacterial infections and disease flares in autoimmune disease patients. The CRP level has no additive value when combined with the PCT level when differentiating bacterial infections from disease flares.
Early differentiation between bacterial infections and disease flares in patients with autoimmune disease is important due to different treatment modalities. Unfortunately, discriminating between bacterial infections and disease flares in patients with underlying autoimmune diseases is difficult because of the similar clinical presentations and laboratory findings. The white blood cell (WBC) count, erythrocyte sedimentation rate (ESR), and C-reactive protein (CRP) level are not always helpful in distinguishing between bacterial infections and disease flares in patients with autoimmune diseases because these markers are elevated not only in infectious conditions, but also when the underlying disease flares (1). Moreover, inflammatory signs can be masked and the CRP level decreased with corticosteroid therapy or immunosuppression (2), which are basic treatments for autoimmune disease, rendering CRP inconsistently reliable as a biomarker for bacterial infection in these patient groups.
Recently, several studies have focused on new markers to distinguish between bacterial infections and disease flares in patients with autoimmune diseases. Procalcitonin (PCT) is one such marker, for which a number of clinical studies have been published. PCT is a protein with a molecular weight of 13 kDa that is produced by the C cells of the thyroid gland as a precursor protein of calcitonin (3). The origin of the synthesis and secretion of PCT during infections are considered to be extra-thyroidal because it has been possible to demonstrate its production in the lung, liver, pancreas, colon, and other organs (4, 5). PCT behaves like an acute phase protein (6) similar to other positive reactants, such as CRP, the production of which is also increased by inflammatory stimuli, including infections (7). After a bacterial stimulus in healthy volunteers, the PCT level rise within 4 hr, reaching peak levels after 6 hours, and maintaining a plateau between 8 and 24 hr (8). Serum PCT is normally undetectable (< 0.05 ng/mL) and PCT levels > 0.5 ng/mL are used to distinguish infections from non-infectious inflammation (9, 10). Most of the published observational studies on PCT in autoimmune diseases have used a semi-quantitative test for PCT measurement (functional assay sensitivity, < 0.5 ng/mL).
The object of this study was to determine the usefulness of serum PCT levels in patients with underlying autoimmune disease. We compared the PCT level in groups with autoimmune disease flares and groups with autoimmune disease complicated by infectious diseases. A highly sensitive PCT immunoassay with a functional assay sensitivity of 0.09 ng/mL (11) was used.
The serum PCT and CRP levels were measured in 79 patients (23 males and 56 females) with underlying autoimmune disease (adult-onset Still's disease [AOSD], n = 3; ankylosing spondylitis [AS], n = 9; Behcet's disease [BD], n = 8; microscopic polyangitis [MPA], n = 1; polyarteritis nodosa [PAN], n = 1; rheumatoid arthritis [RA], n = 33; Sjogren's disease [SD], n = 2; systemic lupus erythematosus [SLE], n = 16; systemic sclerosis [SSc], n = 5; Wegener's granulomatosis [WG], n = 1) who were admitted to the university hospital between September 2009 and September 2010.
The patients were retrospectively classified into 2 groups (disease flares and infections). Serum PCT and CRP levels were measured using an enzyme-linked fluorescent assay (bioMerieux Co., Marcy L'Etoile, France) and a turbidimetric immunoassay (Hitachi High-Technologies Corp., Tokyo, Japan).
Infections were diagnosed in 32 patients. The diagnosis of a bacterial infection was made based on the presence of a positive pathogen test from various specimens (blood, sputum, pus, and urine), clear evidence of infection (pneumonic infiltration on computed tomography [CT]), and clear clinical signs correlating with infection. The infection group was further classified into two subgroups (systemic inflammatory response syndrome [SIRS] and non-SIRS), following the criteria described by Bone et al. (12). SIRS was diagnosed when 2 or more of the following conditions were observed: 1) temperature > 38℃ or < 36℃; 2) heart rate > 90 beats per minute; 3) respiratory rate > 20 breaths per minute or PaO2 < 32 mmHg; and 4) white blood cell count > 12,000/µL, < 4,000/µL, or > 10% immature (band) forms.
Disease flare was diagnosed in 47 patients. The diagnosis of a disease flare was made when there was a significant increase in the activity score based on the following disease activity index compared to the previous condition which was not caused by any other conditions, such as infection or drug use, and when hospitalization was clinically needed for further treatment. The disease activity index used in each disease was as follows; DAS-28CRP (Disease Activity Score; 13) in RA patients; Systemic Lupus Erythematosus Disease Activity Index (SLEDAI; 14) in SLE patients; highly increased ferritin level in AOSD patients (15); Bath Ankylosing Spondylitis Disease Activity Index (BASDAI) (16) in AS patients; Behcet's Disease Current Activity Form (BDCAF) (17) in Behcet's disease patients; European League Against Rheumatism Sjogren's Syndrome Disease Activity Index (ESSDAI) (18) in Sjogren's disease patients; Valentini Scleroderma Disease Activity Index (SDAI) (19) in SSc patients; and Birmingham Vasculitis Disease Activity Score (BVDAS) (20) in vasculitis patients.
There were no cases in this study in which an infection and disease flare were suspected at the same time. This study was conducted retrospectively and diagnostically-ambiguous cases were excluded.
Statistical analysis was carried out using the Statistical Package for the Social Sciences (version 18.0; SPSS, Inc., Chicago, IL, USA). For comparing the two samples, the Mann-Whitney U test was used. An estimated receiver operating characteristic (ROC) curve was used to evaluate the diagnostic power of the CRP and PCT levels by determining the area under the curve (AUC). The sensitivity and specificity of the estimated best cut-off values were also calculated from the ROC curve. A value of P < 0.05 was considered significant.
Among the 79 patients reviewed, 47 were identified with disease flares and 32 were identified with bacterial infections. Thirty-four patients had fever (disease flare [n = 11] and infection [n = 23]) and 20 patients satisfied the criteria for SIRS (disease flare [n = 9] and infection [n = 11]). The mean ages for disease flares and bacterial infections were 47 ± 17 yr and 59 ± 16 yr, respectively (Table 1).
In the bacterial infection group, bacteria were identified in 14 of 32 cases. Nine cases had pneumonic infiltration on chest CT and 9 cases had clinical signs correlated with infection.
The odds ratio (OR) for fever in the differentiation of bacterial infections from disease flares was 8.36 (95% confidence interval [CI], 3.00-23.39), which was superior to SIRS (OR, 2.21; 95% CI, 0.79-6.19).
The CRP and PCT levels were higher in the infection group than the disease flare group (CRP, 11.96 ± 9.60 mg/dL vs 6.42 ± 7.01 mg/dL, P = 0.003; PCT, 2.44 ± 6.55 ng/mL vs 0.09 ± 0.09 ng/mL, P < 0.001; Figs. 1, 2).
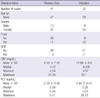
The area under the ROC curves (AUC; 95% CI) for CRP and PCT was 0.70 (0.58-0.82) and 0.84 (0.75-0.93), respectively, which was a significant difference (P < 0.05). The predicted AUC for CRP and PCT combined was 0.83, which was not significantly different compared to PCT alone (P = 0.80). The best cutoff value for CRP was 7.18 mg/dL, with a sensitivity of 71.9% and a specificity of 68.1%. The best cut-off value for PCT was 0.09 ng/mL, with a sensitivity of 81.3% and a specificity of 78.7% (Fig. 3).
Identifying bacterial infections and disease flares in patients with autoimmune diseases is important because the treatment modalities for each condition differ. The immediate use of antibiotics is needed in the bacterial infection group while immunosuppressive drugs are needed in the disease flare group. The wrong choice between the two treatment modalities may aggravate the patient's condition and sometimes the results are fatal. This study showed the CRP and PCT levels to be significantly higher in the infection group than in the autoimmune disease flare group.
Most of the published observational studies on PCT in patients with autoimmune diseases have used a semi-quantitative test for PCT measurement (functional assay sensitivity, 0.5 ng/mL). The normal serum procalcitonin level is < 0.05 ng/mL and because 0.5 ng/mL exceeds the average normal value by > 10-fold, many mild increases in PCT were missed. Therefore, most studies published that the serum PCT level > 0.5 ng/mL is useful in distinguishing infectious from non-infectious inflammation(9, 10), and some studies (2) have used PCT levels to distinguish sepsis from disease flares. In the current study we used an enzyme-linked fluorescent assay (bioMerieux Co.) with a functional sensitivity of 0.09 ng/mL, which made levels < 0.5 ng/mL detectable with accuracy. This functional sensitivity enabled not only sepsis, but also localized bacterial infection to be accurately differentiated from disease flares.
Lanoix et al. (21) reported that the serum PCT level is not different between infections and disease flares in patients with SLE. Specifically, Lanoix et al. used an automated immunofluorometric assay (Brahms Co., Berlin, Germany) to measure PCT levels, which considered PCT levels < 0.5 ng/mL to be normal. Five people were categorized in the infection group (which is a limitation of that study) and the PCT was normal in the all 5 patients using the above standard. In the current study we used a more refined assay method to define serum PCT levels and the normal value was < 0.05 ng/mL. In the current study 4 of 5 SLE patients in the infection group had elevated PCT levels (> 0.09 ng/mL).
Two AOSD patients and one Wegener's granulomatosis patient in the disease flare group had high serum PCT levels without infections. It has been reported that serum PCT levels are higher in patients with active antineutrophil cytoplasmic antibody-associated vasculitis and in patients with AOSD (22, 23). Different PCT levels can be expected in different autoimmune diseases. However, the optimal cut-off values for PCT in different patient groups with different autoimmune diseases have not been established.
The OR for fever in distinguishing bacterial infections from disease flares is superior compared to SIRS. The probable reason for this is the fact that most of the patients in this study had localized infections and there were only two patients with positive bacterial blood cultures.
One patient with a positive bacterial blood culture had a high PCT level (29.7 ng/mL). Higher PCT levels can be expected in sepsis compared to localized bacterial infections (24), but there were not a sufficient number of sepsis patients to accurately calculate the optical cut-off value for sepsis.
Previous studies have reported the diagnostic accuracy of serum PCT for bacterial infections, but the sensitivity and specificity were variable. In the current study the PCT level had better sensitivity and specificity compared to the CRP level (81.3% vs 71.9% and 78.7% vs 68.1%, respectively). A meta-analysis reported a serum PCT sensitivity range from 42%-100% and a specificity range from 54%-100%, while a CRP sensitivity range from 35%-100% and a specificity range from 18%-82% (25). There are no meta-analyses involving serum PCT levels in differentiating bacterial infections from disease flares in patients with autoimmune diseases.
The best cut-off value for CRP in differentiating infections from autoimmune disease flares was 7.18 mg/dL. This value varies with different autoimmune diseases, but is similar to the study by Pepys et al. (26) which reported that a marked CRP elevation (> 6 or 7 mg/dL) in febrile lupus patients favors the diagnosis of bacterial infections.
The predicted AUC for CRP and PCT combined was 0.83, which was not significantly different compared to PCT alone. The CRP level had no additive value when combined with the PCT level in differentiating bacterial infections from autoimmune disease flares. Indeed, this is the first study in which the combined AUC for CRP and PCT was analyzed.
This study showed that serum PCT is useful for differentiating bacterial infections from disease flares in patients with autoimmune disease. It should be clear that no single biomarker is sufficiently sensitive or specific to be relied on completely, and PCT alone cannot replace a physical examination or a thorough medical history. A more accurate analysis can be expected in future studies with a larger number of patients and with each different autoimmune disease group analyzed separately.
Figures and Tables
Fig. 1
Box-plot diagram for CRP in disease flare and infection groups, with box encompassing the range of levels from the 25th percentile (lower bar) to the 75th percentile (upper bar). The horizontal line within the box indicates the median value. The extreme values (within 1.5 times the inter-quartile range [IQR] from the upper or lower quartile) are the ends of the lines extending from the IQR.

Fig. 2
Boxplot for procalcitonin (PCT) in disease flare and infection groups. The explanation is the same as in Fig. 1.

AUTHOR SUMMARY
Serum Procalcitonin for Differentiating Bacterial Infection from Disease Flares in Patients with Autoimmune Diseases
Kowoon Joo, Won Park, Mie-Jin Lim, Seong-Ryul Kwon and Jiyeol Yoon
Early differentiation between bacterial infection and disease flares in autoimmune disease patients is important due to conflicting treatments. Unfortunately discriminating between these two groups is difficult because of the similar clinical presentation and laboratory findings. Recently procalcitonin has been proposed as a new marker for diagnosing infection. Our study revealed that the area under the curve (AUC) of procalcitonin was higher than CRP in terms of its sensitivity and specificity. It is suggested that procalcitonin is useful for differentiating bacterial infection from disease flares.
References
1. Sheldon J, Riches PG, Soni M, Jurges E, Gore M, Dadian G, Hobbs JR. Plasma neopterin as an adjunct to C-reactive protein in assessment of infection. Clin Chem. 1991. 37:2038–2042.
2. Tamaki K, Kogata Y, Sugiyama D, Nakazawa T, Hatachi S, Kageyama G, Nishimura K, Morinobu A, Kumagai S. Diagnostic accuracy of serum procalcitonin concentrations for detecting systemic bacterial infection in patients with systemic autoimmune diseases. J Rheumatol. 2008. 35:114–119.
3. Russwurm S, Oberhoffer M, Zipfel PF, Reinhart K. Procalcitonin: a novel biochemical marker for the mediator-directed therapy of sepsis. Mol Med Today. 1999. 5:286–287.
4. Russwurm S, Stonans I, Stonane E, Wiederhold M, Luber A, Zipfel PF, Deigner HP, Reinhart K. Procalcitonin and CGRP-1 mRNA expression in various human tissues. Shock. 2001. 16:109–112.
5. Müller B, White JC, Nylén ES, Snider RH, Becker KL, Habener JF. Ubiquitous expression of the calcitonin-I gene in multiple tissues in response to sepsis. J Clin Endocrinol Metab. 2001. 86:396–404.
6. Nijsten MW, Olinga P, The TH, de Vries EG, Koops HS, Groothuis GM, Limburg PC, ten Duis HJ, Moshage H, Hoekstra HJ, Bijzet J, Zwaveling JH. Procalcitonin behaves as a fast responding acute phase protein in vivo and in vitro. Crit Care Med. 2000. 28:458–461.
7. Gabay C, Kushner I. Acute-phase proteins and other systemic responses to inflammation. N Engl J Med. 1999. 340:448–454.
8. Dandona P, Nix D, Wilson MF, Aljada A, Love J, Assicot M, Bohuon C. Procalcitonin increase after endotoxin injection in normal subjects. J Clin Endocrinol Metab. 1994. 79:1605–1608.
9. Eberhard OK, Haubitz M, Brunkhorst FM, Kliem V, Koch KM, Brunkhorst R. Usefulness of procalcitonin for differentiation between activity of systemic autoimmune disease (systemic lupus erythematosus/systemic antineutrophil cytoplasmic antibody-associated vasculitis) and invasive bacterial infection. Arthritis Rheum. 1997. 40:1250–1256.
10. Delèvaux I, André M, Colombier M, Albuisson E, Meylheuc F, Bègue RJ, Piette JC, Aumaître O. Can procalcitonin measurement help in differentiating between bacterial infection and other kinds of inflammatory processes? Ann Rheum Dis. 2003. 62:337–340.
11. Hur M, Moon HW, Yun YM, Kim KH, Kim HS, Lee KM. Comparison of diagnostic utility between procalcitonin and C-reactive protein for the patients with blood culture-positive sepsis. Korean J Lab Med. 2009. 29:529–535.
12. Bone RC, Balk RA, Cerra FB, Dellinger RP, Fein AM, Knaus WA, Schein RM, Sibbald WJ. Definitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis: the ACCP/SCCM Consensus Conference Committee: American College of Chest Physicians/Society of Critical Care Medicine. Chest. 1992. 101:1644–1655.
13. van der Heijde DM, van't Hof M, van Riel PL, van de Putte LB. Development of a disease activity score based on judgment in clinical practice by rheumatologists. J Rheumatol. 1993. 20:579–581.
14. Bombardier C, Gladman DD, Urowitz MB, Caron D, Chang CH. Derivation of the SLEDAI: a disease activity index for lupus patients. The Committee on Prognosis Studies in SLE. Arthritis Rheum. 1992. 35:630–640.
15. Bagnari V, Colina M, Ciancio G, Govoni M, Trotta F. Adult-onset Still's disease. Rheumatol Int. 2010. 30:855–862.
16. Garrett S, Jenkinson T, Kennedy LG, Whitelock H, Gaisford P, Calin A. A new approach to defining disease status in ankylosing spondylitis: the Bath Ankylosing Spondylitis Disease Activity Index. J Rheumatol. 1994. 21:2286–2291.
17. Lawton G, Bhakta BB, Chamberlain MA, Tennant A. The Behçet's disease activity index. Rheumatology (Oxford). 2004. 43:73–78.
18. Seror R, Ravaud P, Bowman SJ, Baron G, Tzioufas A, Theander E, Gottenberg JE, Bootsma H, Mariette X, Vitali C. EULAR Sjögren's syndrome disease activity index (ESSDAI): development of a consensus systemic disease activity index for primary Sjögren's syndrome. Ann Rheum Dis. 2010. 69:1103–1109.
19. Valentini G, Della Rossa A, Bombardieri S, Bencivelli W, Silman AJ, D'Angelo S, Cerinic MM, Belch JF, Black CM, Bruhlmann P, Czirják L, De Luca A, Drosos AA, Ferri C, Gabrielli A, Giacomelli R, Hayem G, Inanc M, McHugh NJ, Nielsen H, Rosada M, Scorza R, Stork J, Sysa A, van den Hoogen FH, Vlachoyiannopoulos PJ. European multicentre study to define disease activity criteria for systemic sclerosis: II. identification of disease activity variables and development of preliminary activity indexes. Ann Rheum Dis. 2001. 60:592–598.
20. Luqmani RA, Bacon PA, Moots RJ, Janssen BA, Pall A, Emery P, Savage C, Aden D. Birmingham vasculitis activity score (BVAS) in systemic necrotizing vasculitis. QJM. 1994. 87:671–678.
21. Lanoix JP, Bourgeois AM, Schmidt J, Desblache J, Salle V, Smail A, Mazière JC, Betsou F, Choukroun G, Duhaut P, Ducroix JP. Serum procalcitonin does not differentiate between infection and disease flare in patients with systemic lupus erythematosus. Lupus. 2011. 20:125–130.
22. Scirè CA, Cavagna L, Perotti C, Bruschi E, Caporali R, Montecucco C. Diagnostic value of procalcitonin measurement in febrile patients with systemic autoimmune diseases. Clin Exp Rheumatol. 2006. 24:123–128.
23. Chen DY, Chen YM, Ho WL, Chen HH, Shen GH, Lan JL. Diagnostic value of procalcitonin for differentiation between bacterial infection and non-infectious inflammation in febrile patients with active adult-onset Still's disease. Ann Rheum Dis. 2009. 68:1074–1075.
24. Kim MH, Lim G, Kang SY, Lee WI, Suh JT, Lee HJ. Utility of procalcitonin as an early diagnostic marker of bacteremia in patients with acute fever. Yonsei Med J. 2011. 52:276–281.
25. Becker KL, Snider R, Nylen ES. Procalcitonin assay in systemic inflammation, infection, and sepsis: clinical utility and limitations. Crit Care Med. 2008. 36:941–952.
26. Pepys MB, Lanham JG, De Beer FC. C-reactive protein in SLE. Clin Rheum Dis. 1982. 8:91–103.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download