Abstract
Small pancreatic cancers (longest diameter ≤2 cm) have been regarded as preliminary to early pancreatic cancer, which was thought to be highly curable. During our experience since 1989, we evaluated 542 cases of pancreatic cancer. Among them we found 74 cases of tumors ≤2 cm in diameter, small pancreatic cancer (TS1 pancreatic cancer). Well-differentiated adenocarcinomas (18.9%) and absence of symptoms (8.1%) were more frequent in patients with TS1 than in those with larger pancreatic tumors. Only 16 of the 74 patients (21.6%) with small pancreatic cancers had T1 tumors. According to the International Union Against Cancer (UICC) staging, only 11 patients (14.9%) were stage IA: their 5-yr survival rate was 23.3% and their median survival was 30.0 months. Among these 11 patients, 3 had tumors <1 cm; their median survival time was 30.0 months and their 5-yr survival rate was 50.0%. These findings may indicate that 'small' pancreatic cancer is not equivalent to 'early' pancreatic cancer.
Patients with early cancers of the esophagus and stomach have been found to have better prognosis than patients with advanced cancers. With regard to tumors of the pancreas, however, there is considerable controversy about the diagnosis of early pancreatic cancer. The relationship between the tumor size and postoperative long-term survival was mentioned for the first time in 1964, with pancreatic cancers ≤2 cm in diameter being classified as small (1). In an analysis of 106 patients with small pancreatic cancer (≤2 cm in diameter) (2), however, only 44% of tumors were classified as stage I, remaining within the pancreas, and these patients did not have better prognosis than those with advanced stage tumors. It has been suggested that the majority of pancreatic ductal carcinomas ≤1 cm in diameter are carcinoma in situ and would therefore have better postoperative prognosis, thus being early pancreatic cancers (3). In a study of 36 patients with minute cancers measuring ≤1 cm in diameter, however, the 5-yr post-pancreatectomy survival rate was only 57% (4).
Most retrospective studies of small pancreatic cancers have been performed in Japan, with fewer performed in other countries. Despite the very poor prognosis of patients with these tumors, there have been no large population-based studies, especially regarding small-sized pancreatic cancer. We therefore attempted to identify the clinicopathological aspects of patients with small pancreatic cancer.
We collected data on patients with pancreatic cancer who were treated from October 1989 to May 2006 at one university hospital. Of the over 700 patients with pathologically defined pancreatic malignancy, those with conventional ductal pancreatic cancer were enrolled in this study. Patients with cystic neoplasms, intraductal papillary mucinous neoplasms (IPMN), endocrine tumors, and islet cell tumors were excluded, leaving a total of 542 patients with conventional pancreatic cancer.
The whole tumor was sectioned continuously, and the sections were stained with hematoxylin and eosin and carefully examined microscopically. Tumor size (TS), capsular invasion, retroperitoneal invasion, invasion to the peripancreatic tissues, and metastasis to regional lymph nodes were histologically evaluated. The histologic subtype of each tumor was determined by pathologists well experienced in pancreatic cancers.
The TS was categorized by the criteria of the Japan Pancreas Society (JPS) as TS1, ≤2 cm; TS2, 2.1-4.0 cm; TS3, 4.1-6.0 cm; or TS4, >6.0 cm, and the tumor location was categorized as the head, body, or tail. All tumors were staged according to the International Union Against Cancer (UICC) 6th edition 2004 and JPS staging systems 5th edition 2002, and tumor (T) and nodal (N) factors were determined by histologic findings of the resected specimens (pathological TNM classification).
Initial patient symptoms were evaluated relative to the tumor size; if patients presented with more than one symptom, the chief complaint was selected by a chart review. Tumor markers, including CA19-9 and carcinoembryonic antigen (CEA), were evaluated relative to the tumor size, and their concentrations at the inifial detection of the tumor were determined.
The cumulative survival rate was calculated using the Kaplan-Meier method. Log-rank test was used to evaluate differences between survival curves and to check statistical significance. p values less than 0.05 were considered statistically significant. All analyses were performed using Statistical Package for the Social Sciences (SPSS), version 13.0 (SPSS Inc., Chicago, IL, U.S.A.).
We identified 74 patients (45 men and 29 women) with small pancreatic cancer, defined as having the longest diameter ≤2 cm regardless of stage, ranging in age from 35 to 77 yr (mean age, 57.6 yr). Sixty-five tumors (87.8%) were located in the head of the pancreas, 7 (9.5%) in the tail, and 2 (2.7%) in the body. Seventy-four patients out of 78 (94.8%) underwent pancreatectomy (37 pylorus-preserving pancreaticoduodenectomy or Whipple's operation, 17 distal pancreatectomy, 9 pancreaticoduodenectomy, and 11 total pancreatectomy) and others palliative resection or just surgical biopsy.
We identified a total of 542 patients with pancreatic cancer (all sizes); their histologic subtypes are shown in Table 1. The frequency of well-differentiated adenocarcinoma was higher in TS1 than in larger size tumors (TS2 and TS3) and was significantly higher in TS1 and TS2 than in TS4 tumors (p<0.01). The most frequently observed histologic subtype was moderately differentiated adenocarcinoma. The frequency of poorly differentiated adenocarcinomas was significantly higher in TS2 and TS3 tumors (p<0.01).
Initial symptoms according to the tumor size are shown in Table 2. Abdominal pain was the most frequent symptom (46%), followed by jaundice (28.0%). Similar findings were observed in patients with small pancreatic cancer. Interestingly, patients without any symptoms were more frequent in TS1 than in larger tumors.
In the JPS classification system, the local extent of the tumor (T factor) is graded according to 9 factors: tumor size and invasion of the distal bile duct, duodenal, serosal, and retropancreatic tissue, portal venous system, arterial system, extrapancreatic nerve plexus, and other organs. Lymph node metastasis (N factor) is divided into 3 groups, and distant metastasis (M factor) includes N3 lymph node metastasis. In the UICC classification system, T4 is decided by arterial invasion other than T4 of JPS, and lymph node metastasis is graded as N0 or N1. The positive rate of each factor and the resulting stages in patients with TS1 are summarized in Table 3.
CA19-9 concentrations averaged 344±1,209 U/mL in patients with TS1 tumors, 568±2,129 U/mL in TS2, 448±914 U/mL in TS3, and 3,780±15,574 U/mL in TS4. CA19-9 concentrations are largely dependent on bile duct strictures rather than cancer itself (5). After excluding patients with bile duct strictures, CA19-9 concentrations averaged 466±1,466 U/mL in patients with TS1 tumors, 617±2,714 U/mL in TS2, 313±736 U/mL in TS3, and 3,986±16,907 U/mL in TS4. We also found that CEA concentrations were 3.85±4.66 ng/mL in patients with TS1 tumors, 5.15±14.25 ng/mL in TS2, 17.72±103.17 ng/mL in TS3, and 243.15±634.18 ng/mL in TS4. Thus, these tumor markers did not differ with respect to the tumor size, except for TS4.
Fig. 1 shows the survival rate relative to UICC T stage. Patients with T1 tumors had a median survival time of 30.0 months and a 5-yr survival rate of 19.1%. When these patients were classified according to the JPS classification, their survival curves differed slightly (Fig. 2). In the UICC system, T4 indicates tumor invasion of the celiac or superior mesenteric artery, whereas JPS T4 is not necessarily indicative of arterial invasion. Fig. 3 shows the influence of lymph node metastasis on TS1 patient survival after pancreatectomy, while Fig. 4 shows the relationship between JPS stage and survival after pancreatectomy. Only one patient was stage II, so the p value relative to other stages could not be calculated. Even patients with stage IA tumors, however, had a median survival time of only 30.0 months and a 5-yr survival rate of only 23.3%. When these patients were classified by the UICC staging system (Fig. 5), there was an inversion of prognosis between stage IIB and stages III and IV. In patients with stage III disease and TS1 tumors, T4 invasion should worsen the survival. In addition, only a small number of patients (N=7) had stage III disease.
Since early pancreatic cancer has not been well defined, we classified early pancreatic cancers as those with the longest diameter <1 cm or carcinoma in situ, as suggested by Ariyama et al. (3). Of the eleven patients with UICC stage IA tumors, only three patients had tumors <1 cm in diameter, all of which were carcinoma in situ such as PanIN-3. These accounted for a very small proportion of total pancreatic cancer (3/542:0.55%) and small pancreatic cancer (3/74:4.05%) patients, but they showed a better prognosis than other TS1 patients. One died 9 yr after curative resection, whereas another died of malabsorption due complications of Whipple's operation. The third patient to underwent surgery about 6 months ago, and she remains alive and in good health.
When we divided UICC stage IA cancers into those <1 cm in diameter (subgroup A) and those 1-2 cm in diameter (subgroup B), we found that their 5-yr survival rates were 50% and 0%, respectively. One patient in the subgroup A, however, died not of pancreatic cancer itself but of complications of Whipple's operation (30 months after the operation); if this patient had been excluded, the 5-yr survival rate of the subgroup A would have been close to 100% (Fig. 6). However, the same assumption could be possible in subgroup B patients.
Since the relationship between the tumor size and postoperative long-term survival was first proposed (1), there have been many studies on this subject. In a retrospective evaluation of 106 patients with "small" pancreatic cancer (≤2 cm in diameter) from the Japanese registry, the 5-yr survival rate was only 30% (2). In a meta-analysis of 302 patients with small pancreatic cancer worldwide, an average of 42% of tumors per study were stage I, and the postoperative 5-yr survival rate in each study was less than 50% (6). In a series of 25 patients with small pancreatic cancer, it was suggested that early pancreatic cancer was indicated by tumors ≤1 cm in diameter and limited to the duct epithelium (3). However, a following review suggested that the ordinary type early pancreatic cancer could be defined as an intraductal adenocarcinoma with no or minimal invasion to the stroma, regardless of the size or extent (7). Although the concept of the PanIN (Pancreatic intraepithelial neoplasia) classification (8) has been proposed, many papers still describe pancreatic cancers as small or early. In addition, it has been suggested that radical resection with extensive soft tissue clearance might be more important for prognosis than tumor size alone (9, 10). Degrees of epithelial atypia of the cystic dilated lesions, corresponding to PanIN classifications, may be important in the detection of early-stage pancreatic cancers (11, 12).
A retrospective analysis (13) found that the resectability of TS1 tumors was nearly 89.6%, but the 5-yr survival rate was only 31.7%. When staged according to the JPS classification system, the 5-yr survival rates of patients with stages 1, 2, 3, 4a, and 4b tumors were 20.6%, 3.9%, 37.4%, 23.5%, and 14.6%, respectively. The median survival time of patients with stage 1 tumors was 76.8 months, and the 5 yr survival rate was 57.8%.
From an evaluation of TS1 patients, we found that the 5-yr survival rates for patients with stages IA, IB, IIA, IIB, III, and IV tumors were 23.3%, 0%, 20.6%, 12.7%, 0% and 0%, respectively, and the median survival times were 30.0 months, 12 months, 25.0 months, 10.0 months, 12.0 months, and 17.0 months, respectively (p>0.05 for each comparison). When we divided stage IA into patients with a tumor diameter <1 cm and those with a tumor diameter 1-2 cm, we found that the former subgroup had a median survival time of only 30 months and a 5-yr survival rate of 50.0% (p>0.05). After excluding one patient who died due to complications of Whipple's operation, the 5-yr survival rate in this subgroup approached 100%. Although our results indicate that the small size was not associated with better prognosis compared with larger tumors, tumor size <1 cm showed a trend toward improved prognosis, albeit without a statistical significance. The lack of statistical significance may be due to the relatively small numbers of patients.
We used both the UICC and JPS classifications in the same patients. Although the former is used more often worldwide, it has several limitations (14), including the inability to adequately evaluate the lymph node status without surgical intervention, the inability to determine treatment options from a patient's TMN status, and a lack of association with prognosis. In contrast, while the JPS system has shown improved stratification as well as being more reliable in predicting outcome (15), it has not been used frequently outside Japan. Using the UICC classification system, survival curves were not delineated according to the advancing stage, and there was an inversion between stage IIB and stages III and IV. In contrast, the JPS classification showed more reliable survival curves and results. Although the UICC classification is simpler and easier to understand, the JPS classification may be more reliable in predicting the outcome. Since the numbers of patients evaluated in this study were not large enough to show differences clearly, further studies involving larger numbers of patients by both classification systems may provide a clearer answer.
Despite their limitations, tumor markers such as CEA and CA 19-9 are now used to screen for hidden malignancies in the general population. Although about 80% of patients with pancreatic cancer are positive for serum type 1 chain carbohydrate antigens such as CA19-9, mostly in advanced stages, false-positive rates are relatively high (20-30%) in patients with benign hepatobiliary and pancreatic diseases (16). Generally, high levels of serum tumor markers are associated with more advanced disease (17, 18). We found that CA19-9 and CEA levels were higher in patients with TS4 than in those with smaller tumors. In patients with TS1 tumors, however, CA19-9 and CEA concentrations were not elevated (19), suggesting that these markers are limited in the early detection of pancreatic cancer.
The CA19-9 levels were higher in patients with jaundice than in those without. Unexpectedly, when we excluded patients with jaundice, CA19-9 concentrations were decreased in patients with TS3 tumors. Many patients with pancreatic cancer show biliary tract involvement; after excluding these patients, the number of the remaining of patients was thought to be not sufficient for analysis.
Most pancreatic cancers are not completely curable because they are usually detected in advanced stages, with invasion of adjacent organs or tissues, at which time they are associated with symptoms. Of our patients, 5.5% had no symptoms, and 46.1% had only abdominal pain. Some of the latter patients underwent esophagogastroduodenoscopy (EGD) for abdominal pain, but their EGD findings were within normal limits. In these patients pancreatic cancers were detected by ultrasonography or other modalities several months later. At that time, however, most of these tumors were already inoperable. Conventional ultrasonography is limited by visualization difficulties in the presence of bowel gas or obesity and by its range of resolution (20, 21).
In conclusion, small pancreatic cancers, ≤2 cm in diameter, have a poor prognosis, indicating that small pancreatic cancer is not equivalent to early pancreatic cancer. Smaller sized tumors, <1 cm in diameter, had slightly better prognosis than larger tumors, so early detection of these small tumors is important.
Figures and Tables
Fig. 1
UICC T factor and survival rate after pancreatectomy for TS1 pancreatic cancer. T1, tumor limited to the pancreas, ≤2 cm in its greatest diameter; T3, tumor extending beyond the pancreas but without involvement of the celiac axis or superior mesenteric artery; T4, tumor involving the celiac axis or superior mesenteric artery (total p value <0.05).
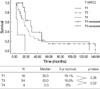
Fig. 2
JPS T factor and survival rate after pancreatectomy for TS1 pancreatic cancer. T1, tumor limited to the pancreas, ≤2 cm in its greatest diameter; T3, tumor extending into the bile duct, duodenum, or peripancreatic tissue; T4, tumor extending into the adjacent large vessels, extrapancreatic nerve plexus, or other organs (total p value <0.05).
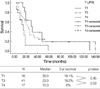
Fig. 3
JPS N factor and survival rate after pancreatectomy for TS1 pancreatic cancer. The grouping of the lymph nodes is described elsewhere (total p value >0.05).
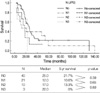
Fig. 4
JPS stage and survival rate after pancreatectomy for TS1 pancreatic cancer (total p value >0.05).
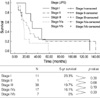
Fig. 5
UICC stage and survival rate after pancreatectomy for TS1 pancreatic cancer (total p value <0.05).

Fig. 6
Minute cancer subgroup A (carcinoma in situ or size <1 cm with minimal invasion to stroma) vs. subgroup B (tumor size 1-2 cm) and survival rate after pancreatectomy for TS1 pancreatic cancer.
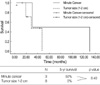
Table 3
Extent of disease in 74 patients with TS1 cancer

TS1, tumor size; UICC, International Union Against Cancer; JPS, Japan Pancreas Society; CH, distal bile duct invasion; DU, duodenal invasion; S, serosal invasion; RP, retropancreatic tissue invasion; PV, portal venous system invasion; A, arterial system invasion; PL, extrapancreatic nerve plexus invasion; OO, invasion of other organ.
References
1. Monge JJ, Dockerty MB, Wollaeger EE, Waugh JM, Priestley JT. Clinicopathologic observations on radical pancreatoduodenal resection for peripapillary carcinoma. Surg Gynecol Obstet. 1964. 118:275–283.
2. Tsuchiya R, Noda T, Harada N, Miyamoto T, Tomioka T, Yamamoto K, Yamaguchi T, Izawa K, Tsunoda T, Yoshino R, Eto T. Collective review of small carcinomas of the pancreas. Ann Surg. 1986. 203:77–81.

3. Ariyama J, Suyama M, Satoh K, Sai J. Imaging of small pancreatic ductal adenocarcinoma. Pancreas. 1998. 3:396–401.

4. Ishikawa O, Ohigashi H, Imaoka S, Nakaizumi A, Uehara H, Kitamura T, Kuroda C. Minute carcinoma of the pancreas measuring 1cm or less in diameter--collective review of Japanese case reports. Hepatogastroenterology. 1999. 46:8–15.
5. Albert MB, Steinberg WM, Henry JP. Elevated serum levels of tumor marker CA19-9 in acute cholangitis. Dig Dis Sci. 1988. 33:1223–1225.

6. Tsunoda T, Yamamoto Y, Kimoto M, Imai H, Iwamoto S, Kawasaki S, Kawashima K, Tadaoka Y, Majima T, Onuma E, Iki K, Kubozoe T, Eto T. Staging and treatment for patients with pancreatic cancer. How small is an early pancreatic cancer? J Hepatobiliary Pancreat Surg. 1998. 5:128–132.

7. Tsuchiya R, Tajima Y, Matsuzaki S, Onizuka S, Kanematsu T. Early pancreatic cancer. Pancreatology. 2001. 1:597–603.

8. Hruban RH, Adsay NV, Albores-Saavedra J, Compton C, Garrett ES, Goodman SN, Kern SE, Klimstra DS, Klöppel G, Longnecker DS, Lüttges J, Offerhaus GJ. Pancreatic intraepithelial neoplasia: a new nomenclature and classification system for pancreatic duct lesions. Am J Surg Pathol. 2001. 25:579–586.
9. Birk D, Fortnagel G, Formentini A, Beger HG. Small carcinoma of the pancreas. Factors of prognostic relevance. J Hepatobiliary Pancreat Surg. 1998. 5:450–454.

10. Pantalone D, Ragionieri I, Nesi G. Improved survival in small pancreatic cancer. Dig Surg. 2001. 18:41–46.

11. Kimura W. How many millimeters do atypical epithelia of the pancreas spread intraductally before beginning to infiltrate? Hepatogastroenterology. 2003. 50:2218–2224.
12. Kimura W. Pancreatic carcinoma in the early stage and limited dilated lesions of the pancreatic ductuli. Nippon Rinsho. 2006. 64:Suppl 1. 165–169.
13. Egawa S, Takeda K, Fukuyama S, Motoi F, Sunamura M, Matsuno S. Clinicopathological aspects of small pancreatic cancer. Pancreas. 2004. 28:235–240.

14. Fernandez-del Castillo C, Jimenez RE. Feldman M, Friedman LS, Brandt LJ, editors. Pancreatic cancer, cystic pancreatic neoplasms, and other nonendocrine pancreatic tumors. Sleisenger and Fordtran's Gastrointestinal and Liver Disease. 2006. 8th ed. 1309–1330.
15. Isaji S, Kawarada Y, Uemoto S. Classification of pancreatic cancer: comparison of Japanese and UICC classifications. Pancreas. 2004. 28:231–234.
16. Sawabu N, Watanabe H, Yamaguchi Y, Ohtsubo K, Motoo Y. Serum tumor markers and molecular biological diagnosis in pancreatic cancer. Pancreas. 2004. 28:263–267.

17. Gattani AM, Mandeli J, Bruckner HW. Tumor markers in patients with pancreatic carcinoma. Cancer. 1996. 78:57–62.

18. Kim HJ, Kim MH, Myung SJ, Lim BC, Park ET, Yoo KS, Seo DW, Lee SK, Min YI. A new strategy for the application of CA19-9 in the differentiation of pancreaticobiliary cancer: analysis using a receiver operating characteristic curve. Am J Gastroenterol. 1999. 94:1941–1946.

19. Steinberg W. The clinical utility of the CA 19-9 tumor-associated antigen. Am J Gastroenterol. 1990. 85:350–355.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download