Abstract
Liver abscesses are very rare complications of ulcerative colitis, and furthermore, there has been only one case of splenic abscess in a patient with ulcerative colitis reported in the English literature. We recently encountered a patient with ulcerative colitis accompanied by both hepatic and splenic abscesses. The patient was treated with abscess drainage as well as sulfasalazine and antibiotics. Follow-up sonography of the abdomen showed complete resolution of the lesions. To our knowledge, this is the first report of combined case of multiple liver abscesses combined with splenic abscess in a patient with ulcerative colitis.
Although liver abscesses are considered a hepatobiliary complication of inflammatory bowel disease (IBD), they are very uncommon. Most have been reported in patients with Crohn's disease, and several in patients with ulcerative colitis. Splenic abscesses are even more rare, and there has been only one case of splenic abscess in a patient with ulcerative colitis reported in the English literature (1).
Here, we describe an 18-yr-old woman with ulcerative colitis accompanied by both hepatic and splenic abscesses, which resolved completely with abscess drainage as well as sulfasalazine and antibiotics. This may be the first report of a case of combined liver and splenic abscesses in a patient with ulcerative colitis.
An 18-yr-old woman presented with a skin defect on the right leg: a pustule that had developed 15 days previously. After she squeezed it, the lesion grew bigger. She visited an outpatient clinic, but the lesion did not heal, so she was admitted to our hospital. Also she had suffered from intermittent diarrhea for one month. Her past medical history was unremarkable. She was pale, and her temperature was 38.2℃. There was slight tenderness on the right upper quadrant. The skin defect measured 20×15 cm. Her white blood cell count was 8,900 cells/µL (normal 4,000-10,000 cells/µL) with 76% segmented leukocytes (normal 50-75%); the hemoglobin level was 2.6 g/dL (normal 13-18 g/dL), and the platelet count was 289,000/µL (normal 150,000-450,000/µL). The serum alkaline phosphatase level was 295 IU/L (normal 50-130 IU/L), total bilirubin 0.9 mg/dL (normal 0.2-1.2 mg/dL), aspartate aminotransferase 41 IU/L (normal 12-33 IU/L) and alanine aminotransferase 17 IU/L (normal 5-35 IU/L). The total protein level was 7.5 g/dL (5.8-8.1 g/dL) and albumin 2.4 g/dL (normal 3.1-5.2 g/dL).
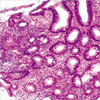
Colonoscopy revealed diffuse multiple ulcers and mucosal nodularity in the rectum and the entire colon (Fig. 1). A barium enema and radiography showed a shortened, haustrafree and narrow entire colon without skip lesions and a preserved terminal ileum (Fig. 2). Colonoscopic biopsy of the colon showed ulceration with infiltration of mixed inflammatory cells and focal glandular disruption (Fig. 3). These findings were compatible with ulcerative colitis. A biopsy from the skin defect demonstrated neutrophilic dermatosis consistent with pyoderma gangrenosum.
To identify the cause of the patient's anemia, a bone marrow biopsy and esophagogastroduodenoscopy were performed. The bone marrow biopsy showed a 4:1 ratio of granulocytic precursors to erythroid precursors. There was no evidence of stainable iron pigments in the particles. These findings were consistent with chronic iron deficiency anemia. The esophagogastroduodenoscopy disclosed no abnormalities.
Computed tomography scans of the abdomen revealed several non-enhancing hypodense lesions in the right hepatic lobe and spleen (Fig. 4). These were consistent with abscesses. Therefore, ultrasound-guided liver biopsy and aspiration was performed on the largest lesion. Thick yellowish pus was drained. Aspiration from the splenic abscess also showed thick yellowish pus. Histology of liver biopsies revealed the infiltration of inflammatory cells with fibrosis in the portal area and abscess formation. Bacterial, anaerobic, and mycobacterial cultures of pus were negative.
The patient was treated with a daily regimen of 4.0 g oral sulfasalazine, 2.0 g intravenous cefazoline, and 500 mg amikacin. One month later, follow-up abdominal ultrasonography showed marked improvement of the hepatosplenic abscesses. A split-thickness skin graft was applied at the skin defect site after debridement. Six months later, the abscesses had completely resolved, and there was complete wound healing over the skin defect site.
Hepatobiliary complications of IBD include fatty liver, cholelithiasis, primary sclerosing cholangitis, chronic active hepatitis, biliary carcinoma and liver abscesses (2). Liver abscesses are a rare complication of IBD, and most cases have been described in patients with Crohn's disease. However, they have also rarely been reported in association with ulcerative colitis, with only seven cases reported in the literature (3-9). Why liver abscesses are less frequent in patients with ulcerative colitis than in Crohn's disease is poorly understood (10).
Splenic abscesses are extremely rare complications of IBD; the only case reported in the English literature was a patient with a 15-yr history of ulcerative colitis, pyoderma gangrenosum, and a presumed primary sclerosing cholangitis. The splenic abscess was aseptic and treated with steroids and cyclophosphamide. Two months later, it had resolved (1).
In our patient, cultures of pus drained from the liver and splenic abscesses were all negative. However, treatment with a regimen of antibiotics as well as sulfasalazine improved the abscess. Therefore, we cannot conclude that they were aseptic.
Neutrophilic dermatoses such as pyoderma gangrenosum or Sweet's syndrome are conditions in which polymorphonuclear leukocyte infiltrates or abscesses can occur without an infectious cause (11). This patient presented with both pyoderma gangrenosum and hepatosplenic abscesses. There was no proven pathogen in the abscesses, so it seems that the two sets of lesions might share a common feature: aseptic neutrophilic infiltration.
Pathogenesis of hepatosplenic abscess in a patient with ulcerative colitis is not clear to the present. Two main possible pathogenic mechanisms are infectious and immunologic ones. Infection is proved basically by the growth of pathogen in cultures. The immunologic mechanism involves both humoral and cellular response. The role of cytokines has been emphasized in the development of neutrophilic dermatosis (granulocyte-colony stimulating factor, IL-1, and IL-8) (12) and of inflammatory bowel disease (tumor necrosis factor, IL-1β, IL-6, IL-8, and IL-10) (13-15). Interestingly for the pathogenesis of sterile abscesses, it is possible that upon stimulation with neutrophil activators, neutrophils promote a subsequent accumulation of mononuclear cells (16). Also impairment of the cytokine balance may bring about the evolution of aseptic collections of polymorphonuclear neutrophils.
The diagnosis of hepatic or splenic abscesses in patients with IBD are frequently delayed. Sine many of the symptoms and signs related to the presence of such abscesses in patients with IBD are similar to the manifestation of IBD per se, they are often incorrectly thought to be arising from exacerbation of the existing disease.
Therefore, many patients are treated with increasing doses of corticosteroids, and part of patients even undergo surgery for resection of the diseased bowel (10). Some recommend that the diagnosis of hepatosplenic abscesses should be considered in febrile patients with IBD whose clinical findings are inconsistent with an exacerbation of the IBD itself (10, 17).
An elevated serum alkaline phosphatase level is the single most reliable laboratory abnormality for the diagnosis of liver abscess, but its sensitivity and specificity are limited (18). Therefore, imaging studies are required for the early diagnosis of this condition. Usually children have higher levels of alkaline phosphatase than adults because children's bones are still growing. During growth spurts, levels can be as high as 500 IU/L. However, since the normal range of alkaline phosphatase in a 18-yr-old woman is 50-130 IU/L, this patient showed an elevated level of alkaline phosphatase (295 IU/L). Also the patient showed fever and tenderness on the right upper quadrant, so we performed computed tomography of the abdomen. This allowed early diagnosis of the hepatosplenic abscesses. An overall mortality of 21% has been reported in patients with Crohn's disease who develop liver abscesses; this is likely to be made worse by delayed diagnosis and immunosuppressive treatment (8).
To our knowledge, this is the first report of a combined case of multiple liver abscesses with splenic abscess in a patient with ulcerative colitis. The abscess was drained, and the patient was treated with sulfasalazine and antibiotics. Follow-up ultrasonography of the abdomen showed a complete resolution of the abscesses.
Liver abscess and splenic abscess are rare complications of ulcerative colitis. But we should bear in mind hepatosplenic abscesses can be complicated in a patient with ulcerative colitis. And its existence should be considered as a differential complication in a patient with ulcerative colitis.
Figures and Tables
Fig. 1
Colonoscopy showing hyperemic mucosa, diffuse multiple geographic ulcers, and mucosal nodularity.

Fig. 2
Barium enema radiograph revealing a shortened, haustra-free and narrowed entire colon without skip lesions.

References
1. Andre M, Piette JC, Frances C, Wechsler B, Delevaux I, Aumaitre O. Retropharyngeal and splenic aseptic abscesses treated with prednisone and cyclophosphamide in a patient with ulcerative colitis. Dig Dis Sci. 2003. 48:1193–1195.
2. Williams SM, Harned RK. Hepatobiliary complications of inflammatory bowel disease. Radiol Clin North Am. 1987. 25:175–188.
3. Lansbury J, Bargen JA. The association of multiple hepatic abscesses and chronic ulcerative colitis. Med Clin North Am. 1993. 16:1427–1431.
4. Treusch JV. Multiple liver abscesses complicating non-specific chronic ulcerative colitis: report of a case. Gastroenterology. 1952. 20:166–173.

6. MacDonald PH, Mercer CD. Hepatic abscess associated with subclinical ulcerative colitis. Can J Gastroenterol. 1989. 3:123–125.

7. Dabrowski M, Koc J, Kus J. Liver abscess in the course of ulcerative colitis. Wiad Lek. 1997. 50:117–119.
8. Song J, Swekla M, Colorado P, Reddy R, Hoffmann S, Fine S. Liver abscess and diarrhea as initial manifestations of ulcerative colitis: case report and review of the literature. Dig Dis Sci. 2003. 48:417–421.
9. Margalit M, Elinav H, Ilan Y, Shalit M. Liver abscess in inflammatory bowel disease: report of two cases and review of the literature. J Gastroenterol Hepatol. 2004. 19:1338–1342.

10. Mir-Madjlessi SH, McHenry MC, Farmer RG. Liver abscess in Crohn's disease: report of four cases and review of the literature. Gastroenterology. 1986. 91:987–993.
11. Callen JP. Pyodema gangrenosum. Lancet. 1998. 351:581–585.
13. Stevens C, Walz G, Singaram C, Lipman ML, Zanker B, Muggia A, Antonioli D, Peppercorn MA, Strom TB. Tumor necrosis factor-α, interleukin-1β, and interleukin-6 expression in inflammatory bowel disease. Dig Dis Sci. 1992. 37:818–826.

14. Jones SC, Evans SW, Lobo AJ, Ceska M, Axon AT, Whicher JT. Serum interleukin-8 in inflammatory bowel disease. J Gastroenterol Hepatol. 1993. 8:508–512.

15. Kucharzik T, Stoll R, Lugering N, Domschke W. Circulating antiinflammatory cytokine IL-10 in patients with inflammatory bowel disease. Clin Exp Immunol. 1995. 100:452–456.
16. Taub DD, Anver M, Oppenheim JJ, Longo DL, Murphy WJ. T lymphocyte recruitment by interleukin-8. J Clin Invest. 1996. 97:1931–1941.
17. Teague M, Baddour LM, Wruble LD. Liver abscess: a harbinger of Crohn's disease. Am J Gastroenterol. 1998. 83:1412–1414.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download