Abstract
It has been suggested that hyperuricemia and possibly gout are associated with the metabolic syndrome, but there have been no direct studies. This study was undertaken to obtain the prevalence of the metabolic syndrome in patients with gout and to compare it with those from the general population studies. This was a 4-institutional case-historical control study composed of 168 patients with gout. We assessed the prevalence of metabolic syndrome according to the ATP III criteria and compared the prevalence with that of the historical controls. To elucidate the factors in gout that were associated with metabolic syndrome, a multivariate analysis was done. The age-adjusted prevalence of metabolic syndrome in gout patients was 43.6%, which was significantly higher than that of the Korean control population (5.2%) from the previous studies. Patients with gout had more components of metabolic syndrome than did the controls. Body mass index (BMI, OR=1.357 (95%CI 1.111-1.657)) and high density lipoprotein (HDL, OR=0.774 (95%CI 0.705-0.850)) were the variables most significantly associated with the occurrence of metabolic syndrome in gout, but alcohol consumption did not show such associations. Gout is associated with the metabolic syndrome, and furthermore, obesity and dyslipidemia were the factors most associated with the syndrome in these patients.
Gout is an inflammatory arthritis that is associated with hyperuricemia, and also is widely known to be associated with obesity, dyslipidemia, hyperglycemia and hypertension. Such metabolic abnormalities have recently been increasingly recognized as not being separate illnesses, but rather they are a clustered syndrome that has been termed the "metabolic syndrome" (1). Metabolic syndrome has gained significant attention through the ATP (Adult Treatment Panel) III guidelines and it is considered to be an independent risk factor for cardiovascular diseases that is comparable to smoking.
It has been suggested that hyperuricemia and possibly gout are associated with insulin resistance or with metabolic syndrome (2-6), but no prevalence study has been done using the ATP III classification criteria. We recently conducted a single-center study (7) concerning this issue, and found the prevalence of metabolic syndrome with gout to be significantly higher than that in the general population (42.2% vs. 6.8%, gout vs. historical control, ATP III criteria used). This study is an expansion of our previous study with the purpose to discover the prevalence of the metabolic syndrome in patients with gout and compare it with the historical controls. We also determined the factors associated with metabolic syndrome.
This was a case-historical control study undertaken in four institutes; Korea University Anam and Guro Hospital, Daegu Catholic University Medical Center and Dong-A University Hospital. A total of 168 patients with gout were recruited and they were checked for the presence of metabolic syndrome according to the ATP III criteria (1). The presence of metabolic syndrome was defined as those patients having ≥3 of the following 5 parameters: a waist circumference >102 cm for males or >88 cm for females, serum triglyceride levels ≥150 mg/dL, serum HDL cholesterol levels <40 mg/dL for males or <50 mg/dL for females, systolic blood pressure ≥130 mmHg or diastolic blood pressure ≥85 mmHg, and a fasting blood glucose ≥110 mg/dL. Those patients with primary gout, as defined by the ACR preliminary criteria for the classification of acute gout (8), were included in the study, and patients with secondary gout (e.g., drug-induced or due to chronic renal failure) were excluded. As corticosteroid therapy may influence metabolic factors, patients who were on chronic steroid therapy (defined as more than a month of any steroid dosage) were also excluded. Due to the cross-sectional nature of this study, missing data occurred in some cases pertaining to the classification criteria (nine cases), and these cases were negatively coded (they were regarded as not fulfilling the criteria).
The prevalence of metabolic syndrome obtained from this study was age-adjusted with using the male population from the year 2000 Population Projection for Korea (9). The prevalence of metabolic syndrome in this study was compared with that from the previous studies done in Korea with the general population, which prevalence was also age-adjusted by using epidemiologic methods. Among the reports, we used the prevalence reported by Lee et al. (10) (5.2%: male sex only, total prevalence: 6.8%) as the prevalence of the general population since it was based on the largest sample size (40,698 persons). There has been a study derived from a national health survey (11) and it reported a 22.1% prevalence among males, but that study used the modified ATP III criteria, in which the waist circumference criteria is adjusted to males ≥90 cm and females ≥80 cm according to the WHO Asia-Pacific obesity criteria (APC) (12), and so our results were compared separately to that study. Historical controls were used for the reason that such data would be more representative of the general population than using clinical data from institutions and so this should make a more objective comparison. As hyperuricemia and hypertriglyceridemia are associated with alcohol consumption and this may confound the results, the amount of alcohol consumption was checked in a categorized fashion. We classified the patients by the average daily alcohol consumption into three groups; non-drinkers, moderate drinkers (≤30 g/day), or heavy drinkers (>30 g/day).
A case-only analysis for comparing gout patients with or without metabolic syndrome by multiple logistic regression analysis was conducted to determine the strongest factors associated with the occurrence of metabolic syndrome with gout. Statistical analysis was done with SPSS for Windows 10.0 (SPSS Inc. Chicago, U.S.A.). Comparisons between the continuous or categorical variables were done by t-tests or chi-square tests, respectively. To compare variables among the different alcohol consumption groups, we used one-way analysis of variance (ANOVA). The prevalence, expressed as rates, was compared using chi-square tests of homogeneity. Multiple logistic regression analysis was applied for the multivariate analysis as described above, and the results are given in odds ratios (OR) with 95% confidence intervals (95% CI). Variables with p values of <0.05 were considered significant.
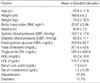
A total of 168 patients with gout were recruited from the four hospitals. Table 1 shows the descriptive data of these patients. All the patients were males, and the mean age was 53±11.9 yr. Almost half (47.6%) were hypertensive and 10.7% were diabetic, and this is similar to previous data from patients with gout (13). Forty-two percent (42.9%) drank in moderation (≤30 g/day) and 28.6% drank heavily (>30 g/day) (Table 2). Differences in the variables among the alcohol consumption groups could be seen for the triglyceride and glucose levels. The triglyceride levels increased linearly in proportion to the alcohol consumption levels, while the glucose levels were lowest among the moderate drinkers. The urate levels were not significantly different among the groups (Table 2).
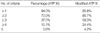
The age-adjusted prevalence of metabolic syndrome with gout was 43.6%, which is significantly higher than that of the control population (10) (p<0.001) (Table 3). When using the modified ATP III criteria where the waist criteria is lowered to ≥90 cm in males and ≥80 cm in females, the prevalence jumped up to 57.2%, and this is also significantly higher than that of the control population (11). According to these results, gout is strongly associated with the metabolic syndrome. The prevalence of metabolic syndrome according to the age groups is shown in Table 4. The prevalence is nearly uniform (50-60%) across the age groups when using the modified ATP III criteria. The percentage of patients who fulfilled the individual components of the ATP III or modified ATP III criteria is shown in Table 5. Among the components, hypertension and hypertriglyceridemia were the most common components, and this is similar to both the control populations. Table 6 shows the percentage of patients who simultaneously fulfilled several components of each set of criteria in an incremental order. Seventy-two percent of the patients with gout had at least 2 components of metabolic syndrome (85.7% with the modified ATP III criteria), which is much higher than the values of 23.2% (ATP III) (10) or 46.4% (modified ATP III) (11) from the control populations.
The multivariate analysis displayed on Table 7 shows the independent variables associated with the occurrence of metabolic syndrome (ATP III criteria) with gout. The patients with higher body mass index (BMI) levels were at the greatest risk of having metabolic syndrome (OR 1.357, 95%CI 1.111-1.657, p=0.003), while the patients with higher high density lipoprotein (HDL) levels were at the lowest risk (OR 0.774, 95% CI 0.705-0.850, p<0.001). When considering the difference in the weights of the units among the variables, (i.e., increasing BMI by 1 is far more difficult than increasing blood pressure or glucose by 1), systolic blood pressure (SBP) could be the strongest variable with an OR of 2.203 (increments in 10 mmHg). However, neither the urate levels nor the alcohol consumption levels were significantly associated with metabolic syndrome.
The concept of metabolic syndrome was first suggested by Reaven in 1988 (14), and it is now an acknowledged major risk factor for cardiovascular diseases in the ATP III guidelines. Its components can be divided into hypertension, obesity, hyperglycemia and dyslipidemia. As gout is also generally known to be associated with such metabolic abnormalities, it seems somewhat unusual that there have not been few, if not any, epidemiologic studies concerning the prevalence of metabolic syndrome in patients with gout up to this time. This study is the first in Korea to determine the association of metabolic syndrome with gout by performing a prevalence comparison with using the ATP III classification criteria. There is an article reporting that 86% of patients with gout have metabolic syndrome (15). As discussed in this report, this difference in prevalence may reflect a difference between diverse ethnic populations. Our results were remarkably similar to the results of that of the single-center study (7), and they suggest that gout is associated with metabolic syndrome as there is a much higher prevalence of metabolic syndrome in patients with gout than in the general population. This is true even when comparing with a study from a middle-aged Korean population (17.6%) (16), which age distribution may match the gout-prevalent ages. The majority of patients with gout (>70%) had at least two metabolic risk factors, suggesting that these patients may have a higher risk for cardiovascular complications than normal individuals. Obesity (or hypertension) may have stronger effects on the development of metabolic syndrome in gout than the other components. However, the urate levels, and more importantly, alcohol consumption did not have significant effects on the occurrence of metabolic syndrome in patients with gout. This has significance in terms of the effects of alcohol on the lipid levels. Alcohol consumption has been recently confirmed to have an effect on the development of gout (17). Also, such alcohol consumption could lead to higher triglyceride levels and lower HDL levels, which may lead to an increased prevalence of metabolic syndrome. However, this was not the case in our study. Because the prevalence of metabolic syndrome did not differ across the levels of alcohol consumption, and also because the triglyceride and HDL variables, even when they were adjusted for alcohol consumption, remained significant on the multivariate analysis, the effects of alcohol on metabolic syndrome in patients with gout does not seem to be significant. As the effects of alcohol consumption on the development of metabolic syndrome or insulin resistance are not consistent, as was shown in previous studies (18-22), interpretation of our results should be done cautiously. We give the meanings that alcohol consumption did not influence metabolic factors such as lipid levels to make more cases of the metabolic syndrome, and so did not confound us that gout has more individuals with metabolic syndrome through alcohol consumption. Although gout seems to be associated with metabolic syndrome due to its higher prevalence, serum urate did not play a significant role in the development of metabolic syndrome in our patients. This might have happened due to the fact that many of the patients should have been on hypouricemic therapy, and more importantly, since virtually all patients with gout are hyperuricemic, it may be expected to have made no differences. However, uric acid was included in the model for the purpose of controlling for possible confounding, and the results are the same without the urate variable. Therefore, a more generalized case-control study might indicate the significance of uric acid in metabolic syndrome. There is a study that uric acid is related to the components of the metabolic syndrome in the Korean population. (23)
This study might have some weakness, as there were 7 cases (4.2%) missing from the waist data and 2 cases (1.2%) missing from the blood pressure data. However, as the missing values were negatively coded, these should not have had an influence on our conclusions. The significance of obesity and HDL as the strongest positive and negative factors for metabolic syndrome in gout patients should be revalidated and if it is so, this may give insights into the development of hyperuricemia and gout and hopefully, lead to its effective management. Obesity, as well as low HDL levels combined with hypertriglyceridemia are suggested to be associated with insulin resistance (24-26), and as they were the variables with the strongest effects on metabolic syndrome in patients with gout, our data indicates that gout (or hyperuricemia) is more related with dyslipidemia and obesity rather that hyperglycemia or hypertension. As patients with gout are essentially a subgroup of hyperuricemic individuals, larger samples are needed to generalize to, or to compare with the asymptomatic hyperuricemic individuals, who in fact represent the majority of the hyperuricemic population. The results from such studies may give more perspectives on the development of hyperuricemia.
Figures and Tables
References
1. Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) final report. Circulation. 2002. 106:3143–3421.
2. Cigolini M, Targher G, Tonoli M, Manara F, Muggeo M, De Sandre G. Hyperuricaemia: relationships to body fat distribution and other components of the insulin resistance syndrome in 38-year-old healthy men and women. Int J Obes Relat Metab Disord. 1995. 19:92–96.
3. Bonora E, Targher G, Zenere MB, Saggiani F, Cacciatori V, Tosi F, Travia D, Zenti MG, Branzi P, Santi L, Muggeo M. Relationship of uric acid concentration to cardiovascular risk factors in young men. Role of obesity and central fat distribution. The Verona Young Men Atherosclerosis Risk Factors Study. Int J Obes Relat Metab Disord. 1996. 20:975–980.
4. Rathmann W, Funkhouser E, Dyer AR, Roseman JM. Relations of hyperuricemia with the various components of the insulin resistance syndrome in young black and white adults: the CARDIA study. Ann Epidemiol. 1998. 8:250–261.

6. Fam AG. Gout, diet, and the insulin resistance syndrome. J Rheumatol. 2002. 29:1350–1355.
7. Rho YH, Choi SJ, Lee YH, Ji JD, Choi KM, Baik SH, Song GG. Prevalence of the metabolic syndrome in patients with gout. J Korean Rheum Assoc. 2004. 11:349–357.
8. Wallace SL, Robinson H, Masi AT, Decker JL, McCarty DJ, Yu TF. Preliminary criteria for the classification of the acute arthritis of primary gout. Arthritis Rheum. 1977. 20:895–900.

9. Korea National Statistical Office. Population projections for Korea: 2000-2050. 2001. 63.
10. Lee WY, Park JS, Noh SY, Rhee EJ, Kim SW, Zimmet PZ. Prevalence of the metabolic syndrome among 40,698 Korean metropolitan subjects. Diabetes Res Clin Pract. 2004. 65:143–149.

11. Kim MH, Kim MK, Choi BY, Shin YJ. Prevalence of the metabolic syndrome and its association with cardiovascular diseases in Korea. J Korean Med Sci. 2004. 19:195–201.

12. Steering Committee of the WHO Western Pacific Region, IASO & IOTF. The Asia-Pacific perspective: Redefining obesity and its treatment. 2000. Australia:
13. Jeon CH, Kim HJ, Kim EH, Ahn JK, Koh JH, Cha HS, Koh EM. Clinical manifestations of gout in Korea. Korean J Med. 2002. 62:648–656.
14. Reaven GM. Banting lecture 1988. Role of insulin resistance in human disease. Diabetes. 1988. 37:1595–1607.

15. Vazquez-Mellado J, Garcia-Garcia C, Guzman-Vazquez S, Medrano G, Ornelas M, Alcocer L, Marquez A, Burgos-Vargas R. Ischemic heart disease and metabolic syndrome in gout. J Clin Rheumatol. 2004. 10:105–109.
16. Kwon HS, Park YM, Lee HJ, Lee JH, Choi YH, Ko SH, Lee JM, Kim SR, Kang SY, Lee WC, Ahn MS, Noh JH, Kang JM, Kim DS, Yoon KH, Cha BY, Lee KW, Kang SK, Son HY. The prevalence and clinical characteristics of the metabolic syndrome in middle-aged Korean adults. Korean J Med. 2005. 68:359–368.
17. Choi HK, Atkinson K, Karlson EW, Willett W, Curhan G. Alcohol intake and risk of incident gout in men: a prospective study. Lancet. 2004. 363:1277–1281.

18. Kiechl S, Willeit J, Poewe W, Egger G, Oberhollenzer F, Muggeo M, Bonora E. Insulin sensitivity and regular alcohol consumption: large, prospective, cross sectional population study (Bruneck study). BMJ. 1996. 313:1040–1044.

19. Goude D, Fagerberg B, Hulthe J. Alcohol consumption, the metabolic syndrome and insulin resistance in 58-year-old clinically healthy men (AIR study). Clin Sci (Lond). 2002. 102:345–352.

20. Park YW, Zhu S, Palaniappan L, Heshka S, Carnethon MR, Heymsfield SB. The metabolic syndrome: prevalence and associated risk factor findings in the US population from the Third National Health and Nutrition Examination Survey, 1988-1994. Arch Intern Med. 2003. 163:427–436.
21. Rosell M, De Faire U, Hellenius ML. Low prevalence of the metabolic syndrome in wine drinkers--is it the alcohol beverage or the lifestyle? Eur J Clin Nutr. 2003. 57:227–234.

22. Yoon YS, Oh SW, Baik HW, Park HS, Kim WY. Alcohol consumption and the metabolic syndrome in Korean adults: the 1998 Korean National Health and Nutrition Examination Survey. Am J Clin Nutr. 2004. 80:217–224.

23. Yoo TW, Sung KC, Kim YC, Hwang ST, Oh SY, Shin HS, Kim BJ, Kim BS, Kang JH, Lee MH, Park JR, Kim H, Lee KB, Lhee HY, Ryu SH, Keum DG. The relationship of the hypertension, insulin resistance, and metabolic syndrome in the serum uric acid level. Korean Circulation J. 2004. 34:874–882.

24. Tai ES, Emmanuel SC, Chew SK, Tan BY, Tan CE. Isolated low HDL cholesterol: an insulin-resistant state only in the presence of fasting hypertriglyceridemia. Diabetes. 1999. 48:1088–1092.

25. Bo S, Cavallo-Perin P, Gentile L, Repetti E, Pagano G. Low HDL-cholesterol: a component of the metabolic syndrome only in the presence of fasting hypertriglyceridemia in type 2 diabetic patients. Diabetes Metab. 2001. 27:31–35.




 PDF
PDF ePub
ePub Citation
Citation Print
Print







 XML Download
XML Download