Abstract
Acoustic pharyngometry is a relatively new noninvasive method that quantifies geometrically complexed pharyngeal dimensions. Our study aimed to investigate the predictability and usefulness of acoustic pharyngometry in diagnosis of obstructive sleep apnea (OSA), and we developed a prospective clinical trial in 16 subjects without apnea and 54 subjects with apnea. All seventy subjects received polysomnography (PSG) to assess the sleep architecture, including breathing and the degree of apnea hypopnea index. Acoustic pharyngometry was performed in four body positions (sitting, supine, right and left lateral) while awake with tidal breathing in addition to morphometric measurements (Kushida index) of oral cavity. This study shows that the cross-sectional area and volume of the upper airway is smaller in the supine position than any other positions. As well, the oropharyngeal junction area of the supine position is the most predictive parameter to discriminate between subjects with or without OSA. Acoustic pharyngometry can be a clinically useful tool for localizing the narrowed portion of the upper airway and predicting obstructive sleep apnea.
Obstructive sleep apnea (OSA) is characterized by recurrent total or partial upper airway (UA) narrowing or collapsing that occurs at different sites from the oropharynx to the hypopharynx during sleep. It is manifested clinically with loud and irregular snoring, apneas, restless sleep, daytime sleepiness, and can cause death as well as cardiovascular, metabolic and neuropsychological morbidity. Its prevalence increases with age, has a male preponderance with up to 25% of working age men having disturbed breathing during sleep (1) and up to 80% of cases of OSA remaining undiagnosed. The pathophysiological basis of OSA is periodic airway occlusion resulting in sleep and blood gas disturbance which leads to cardiovascular disease, hypertension, arrhythmia, increased risk of traffic accidents, disturbed psychosocial performance and metabolic and neuroendocrine dysfunction (2). However, the exact pathophysiology of OSA has not been fully understood up to date.
Through upper airway imaging and many other studies, the narrowing or collapse of the upper airway has been a major focus of investigation for OSA and some contributory factors were suggested, including (a) a sleep-induced decrease in upper airway dilator muscle activity, (b) an anatomically small pharyngeal airway, (c) relatively thick lateral pharyngeal walls, and (e) an increase in the total volume of parapharyngeal fat, (f) decrease or complete cessation of superior pharyngeal constrictor muscle activity (3, 4). Among these factors pharyngeal size, compliance and the dynamic behavior of UA have been considered important factors in the pathogenesis of OSA. So, the assessment of the precise narrowing site of the UA in OSA patients may not be only one of the keys in understanding the pathogenesis of this disorder, but also in improving the management of this condition and the success rate of the surgical treatment (5). Therefore, identification of the sites of UA obstruction is an important step in determining the treatment choice. Several methods have been used to localize the obstructed area of the UA in OSA patients. Such methods are physical examination, physiologic measurement of pressure and resistance along the UA, fiberoptic endoscopy with the so-called Müller maneuver, as well as cephalometric roentgenograms, fluoroscopy, computerized tomography, and magnetic resonance imaging (6). But, some of these methods are invasive, other require exposure to radiation, or are not cost effective. Since the cross-sectional area of the upper airway varies with respiration phase and body position, and occlusion and narrowing are also most apparent during tidal breathing because of the dynamic alterations in the pharyngeal airway associated with changes in lung volume (7-9), we need dynamic methods for evaluation that are more cost-effective, non-invasive, easy, and do not require radiation exposure. Acoustic pharyngometry has the potential for localizing such sites in an easy, rapid, cost-effective and reproducible manner. Therefore, the implementation of acoustic pharyngometry for the assessment of dynamic changes in UA offers a potentially simple way to obtain information about the anatomy of the pharyngeal airway, the location of abnormal sites, and the presence of apnea.
Fifty-four subjects with OSA and sixteen subjects without OSA were recruited to the study. This study was approved by the Human Ethics Review Committee of Sydney University and informed consent was obtained before each evaluation. Information collected for each subject included standardized medical history, physical examination, general demographics (age, sex, ethnicity, BMI, neck circumference), standard overnight diagnostic polysomnography, acoustic pharyngometry, and morphometric measurements of oral cavity (Kushida index). We excluded any subjects with underlying pulmonary diseases or nasal obstructive diseases, such as asthma, chronic obstructive pulmonary disease, nasal septal deviation, allergy, nasal polyp, chronic paranasal sinusitis.
Sleep and breathing were assessed by full overnight polysomnography in the laboratory at Royal Prince Alfred Hospital Sleep Unit. Standard overnight polysomnography was performed, with two channels of electroencephalogram (EEG gg) (C1/A3, C2/A4), electro-oculogram (EOG), and one channel of submental electromyogram (EMG) electrodes applied in the standard fashion for sleep stage determination. Respiratory variables included chest wall and abdominal motion (Respitrace®; Ambulatory Monitoring Inc., Ardsley, NY, U.S.A.), nasal airflow and pressure with a calibrated pressure transducer (Grass volumetric; Grass Instrument Co., Quincy, MA, U.S.A.), and arterial oxyhemoglobin saturation (Biox 3700e; Ohmeda, Louisville, CO, U.S.A.). An electrocardiogram was recorded continuously. All variables were recorded continuously on a 16-channel electroencephalograph (Grass Instrument Co). Calculated respiratory variables incuded the respiratory disturbance index (RDI) which refers to the number of apneas and hypopneas per hour of sleep, as well as apnea duration, and minimal oxygen saturation during apneas. Data were recorded continuously on a computerized polygraph (Compumedics E series, Melbourne, Australia) and scored by a single technologist using American Academy of Sleep Medicine consensus methods (10).
Apneas were defined as cessation of airflow for at least 10 sec. Hypopnea was defined as a reduction in amplitude of airflow or thoracoabdominal wall movement of greater than 50% of baseline for more than 10 sec. These events were defined as obstructive if they occurred in association with continued diaphragm EMG activity and thoracoabdominal wall movement. Central events were defined as those accompanied by absence of diaphragm EMG activity and thoracoabdominal wall movement. We classified as severe OSA (RDI >30 events/hr), moderate OSA (RDI between 15-30 events/hr), mild OSA (RDI between 5-15 events/hr), and normal (RDI <5 events/hr).
Acoustic pharyngometric data were collected before sleep study usually in the sleep laboratory at Royal Prince Alfred Hospital sleep unit using acoustic pharyngometer (E. Benson Hood Laboratories, Pembroke, MA, U.S.A.) with a scuba diving type mouthpiece.
First, the subject was seated in a straight-backed exam chair and asked to assume a comfortable posture to allow the subject to maintain a fixed gaze. Any non-permanent orthotic appliances were removed for the test. Possible sources of artifacts were the head position in relation to cervical spine (extension or flexion), shoulder position, uncontrolled tongue position, malpositioned wave tube, subject's awareness of his or her breath and change in respiratory rate, and volume (11). As such, before evaluation, the examiner measured the distance between the chin and suprasternal notch. This distance was applied to all other positions to avoid extension or flexion of the head in relation to cervical spine. All subjects were asked to breathe through the mouth without a noseclip or vocalizing, to ensure the nasopharynx was kept occluded by the palate. This approach was employed to prevent the loss of sound waves into the nasal cavity (or the silent "oooh" will keep the velum closed). It was imperative that the lips fully seal the mouthpiece, otherwise the subject may have an acoustic leak, resulting in an erroneously large area. Before positioning the mouthpiece, subjects were advised to rest their teeth on the inner flanges of the mouthpiece, not bite down, and keep their tongue flat. In the supine position, pillows were not used to support the head, preventing neck flexion and subsequent upper airway narrowing. In the lateral position, one pillow was used for neck support (12). Ten measurements of the upper airway were taken at the beginning of inspiration during tidal breathing with the pharyngeal airway maintained by holding the neck in a neutral position. This sequence will be repeated in upright sitting, supine, right and left lateral body positions. To protect the microphone, saliva must be prevented from entering into the wave tube. To this end, the wave tube was held with microphone uppermost (the cable attachment is on the same side of the wave tube as the microphone) and parallel to the floor or perpendicular to the subject's head.
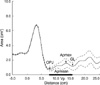
Cross sectional area versus distance down the airway trace was obtained and reconstructed on the computer screen. Traces were screened for having a standard curve of mouth peak, oropharyngeal minimum, pharyngeal peak and glottis minimum. From each mean trace, five upper airway landmarks, including OPJ (oropharyngeal junction area, cm2), Apmax (maximum pharyngeal area, cm2), GL (glottic area, cm2), Apmean (mean pharyngeal area from OPJ to GL, cm2), Vp (pharyngeal volume, as the integrated area under the curve between the OPJ and the GL, µL) were measured (Fig. 1).
We applied Kushida et al.'s approch for predicting whether a subject has obstructive sleep apnea, and measured body mass index, neck circumference, and oral cavity measurements (13). Kushida index (KI) was calculated by P+(Mx-Mn)+3×0J+3×[Max (BMI-25, 0)]×(NC÷BMI)
P is palatal height (in millimeters) or the distance from the dorsum of the tongue at the median lingual sulcus to the highest point of the palate measured with the tongue in a relaxed position and the maxillary and mandibular incisor tips subtending an angle of 20 degrees from the mandibular condyle. Mx is the maxillary intermolar distance (in millimeters) between the mesial surfaces of the crowns of the maxillary second molars. Mn is the mandibular intermolar distance (in millimeters) between the mesial surfaces of the crowns of the mandibular second molars. OJ is the overjet (in millimeters), or the horizontal overlap of the crowns of the maxillary and mandibular right central incisors. BMI is the body mass index (kg/m2) and NC is neck circumference (in centimeters) measured at the level of the cricothyroid membrane. Oral cavity measurements were made with calipers after removal of the sharp tips. By placing the caliper tips between the oral cavity structures to be measured, carefully removing the caliper, and measured the distance between the tips with ruler.
We set the separation value between subjects with or without OSA at 70. In general KI of 70 or more correspond to subject with OSA, KI less than 70 correspond to subject without OSA.
Descriptive results are expressed as mean±standard deviation. Lineal regression analysis was performed in every pharyngeal parameter. The relationships among variables were evaluated with Tukey's post-hoc test to compare the acoustic pharyngometric data, Kushida index, polysomnographic data, and general demographics between subjects with or without OSA. Analysis was performed using standard software (SAS version 10.0; SAS Institute, Cary, NC, U.S.A.). Statistical significance was defined as p<0.05.
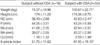
Seventy subjects were evaluated. The demographics of the subjects are summarized in Table 1. There were 54 subjects with OSA and 16 subjects without OSA. Most subjects were Caucasian, and there was a marked male predominance (90%).
Average Apnea-Hypoapnea Index (AHI) of subjects without OSA was 2.10 and 34.73 in subjects with OSA. Subjects with severe OSA (RDI >30 events/hr) were 26, moderate OSA (RDI between 15-30 events/hr) was 12, and mild OSA (RDI between 5-15 events/hr) was 16.
Table 2 shows pharyngeal measurements; OPJ (oropharyngeal junction area, cm2), Apmax (maximum pharyngeal area, cm2), GL (glottic area, cm2), Apmean (mean pharyngeal, cm2), Vp (pharyngeal volume, µL) according to body positions.
No significant differences were noted between subjects with or without OSA based on VP or Apmax. However, a statistically significant decrease was found at OPJ and Apmean in supine, left lateral and right lateral positions among subjects with OSA when compared with subjects without OSA. As well, a significant increase existed at GL in sitting position only among subjects with OSA when compared with subjects without OSA. This increment was thought to be the result of post-stenotic dilatation. The most significant differentiation between subjects with or without OSA was at OPJ in supine position. When the separation value was set as 1 cm2, the sensitivity (50 of 54) was 93% and the specificity (15 of 16) was 94% for differentiation of OSA. The positive predictive value (50 of 51) was 98% and the negative predictive value (15 of 19) was 79%. Pharyngometric measurements were not correlated with age, Kushida index.
Table 3 shows the Kushida index. Statistically significant increase was found in subjects with OSA. The sensitivity (48 of 54) was 89% and the specificity (15 of 16) was 94% for differentiation of OSA, when the separation value was set as 70. The positive predictive value (48 of 49) was 98% and the negative predictive value (15 of 21) was 71%. The Kushida index was also highly correlated with BMI, but not with age or other pharyngometric measurements.
OSA is a complex disease process characterized by repeated UA obstruction during sleep. The etiology is multifactorial and not fully understood, but the final result of this disease process is obstruction of the UA during sleep. Pharyngeal size and dynamic behavior of the pharyngeal airway may be important factors in pathogenesis of OSA. The examination and evaluation of the UA anatomy provide important information to the physician to confirm diagnosis and support decision-making among various treatments. However, the lack of simple, accurate, non-invasive, repeatable method has been an obstacle for the systematic evaluation of UA.
Acoustic reflection technique is not a newly developed method. It was originally described by Jackson et al. (14) and further modified by Fredberg et al. (15), who used this technique to measure tracheal cross-sectional areas in human subjects. The technique is based on sending acoustic impulses along the respiratory tract. As they travel through the airways, they are partially reflected whenever there is a change in the airway cross-sectional area. By calculating the amplitude and temporal changes in the reflected pulse compared with the incident pulse, it is possible to assess cross-sectional area and volume from the oral cavity to hypopharynx. Through many studies the accuracy of pharyngometry-derived measurements has been evaluated. D'Urzo and associates (16) demonstrated excellent agreement between glottic area measurement derived acoustically (1.8±0.8 cm2) as compared to those obtained through CT (1.7±0.9 cm2). Marshall et al. (17) acoustically evaluated the pharyngeal dimensions of 10 normal human subjects and compared these measurements to those obtained through MRI. They demonstrated no significant difference in pharyngeal and glottic cross-sectional areas. Malhotra and associates (18) evaluated the two collapsibility measurement techniques in normal and apneic subjects during wakefulness and sleep. They suggested that upper airway collapsibility measured during wakefulness does provide useful physiologic information about pharyngeal mechanics during sleep and demonstrated clear differences between individuals with and without sleep apnea. Through our study, we found that subjects with OSA show consistently reduced pharyngeal airway area and volume compared with normal subjects. We also found that all subjects had smaller upper airway area and volume in supine position and larger upper airway area and volume in sitting position which may be due to the effect of gravity. This study suggests that acoustic pharyngometry provide a useful parameter for the cross sectional area of OPJ in supine position. Therefore, during evaluation by acoustic pharyngometry, it is necessary for the examiner to first identify the OPJ in supine position for screening OSA.
There are several other methods for the evaluation of the UA such as direct and fiberoptic visualization, UA pressure and resistance measurement, cephalometric roentgenogram, fluoroscopy, CT, and MRI. But, the acoustic reflection technique offers several advantages over other methods for objectively evaluating UA structure and function. As compared to fiberoptic pharyngoscopy, the acoustic technique is non-invasive and more easily quantitative. As compared to the radiographic assessment such as CT scan or cephalometry, the acoustic technique is inexpensive, quick, does not involve exposure to radiation and is easily repeatable. This technique also has it's the capability to provide a real-time display of the UA and assess the entire airway simultaneously and rapidly. The disadvantages of the technique are that it requires some degree of cooperation from the subject, it would be difficult to perform during sleep, and does not provide information on the nasopharynx.
The morphometric measurement of oral cavity and acoustic pharyngometry enables an examiner to predict the presence or absence of OSA rapidly and accurately during an initial visit. Through this study we found the sensitivity and specificity of the morphometric measurement of oral cavity to be 89% and 94%, and acoustic pharyngometry are 93% and 94%, respectively. Acoustic pharyngometry is a more accurate method for predicting the presence or absence of OSA.
Because PSG is not a popular screening tool for sleep apnea, an easily reproducible predictive tool such as acoustic pharyngometry is needed to screen the patients. A acoustic pharyngometry seems to have potential utility for localizing the possible narrowing area and offers a predictive value for subjects with OSA at the initial visit. However, these measurements are not suggested to replace polysomnography in the evaluation of OSA because these measurements do not assess the severity of OSA. Rather, using these measurements as a screening tool may help primary physician decide which patients should be referred to sleep centers for further evaluation and treatment of OSA.
To summarize, we conclude that acoustic pharyngometry is a useful alternative to invasive and expensive methods of measuring upper airway in subjects with OSA. In addition, the cross-sectional area at OPJ in supine position is a potentially important parameter in evaluation of OSA. Further study is needed to assess the relationship between pharyngeal dimension and subsequent development of OSA.
Figures and Tables
Fig. 1
Representative output of the acoustic pharyngometry. There are 5 parameters on graph as shown in arrow and thick line. OPJ, oropharyngeal junction area; Apmax, maximum pharyngeal area; GL, glottic area; Apmean, mean pharyngeal area from OPJ to GL; Vp, pharyngeal volume as the integrated area under the curve between the OPJ and the GL. All the parameters were calculated by computer system.
References
1. Young T, Palta M, Dempsey J, Skatrud J, Weber S, Badr S. The occurrence of sleep-disordered breathing among middle-aged adults. N Engl J Med. 1993. 328:1230–1235.

3. Schwab RJ, Gupta KB, Gefter WB, Metzger LJ, Hoffmann EA, Pack AI. Upper airway and soft tissue anatomy in normal subjects and patients with sleep-disordered breathing. Am J Respir Crit Care Med. 1995. 152:1673–1689.
4. Kuna ST, Smickley JS. Superior pharyngeal constrictor activation in obstructive sleep apnea. Am J Respir Crit Care Med. 1997. 156:874–880.

5. Ikeda K, Oshima T, Shimomura A, Takasaka T. Surgical criteria for obstructive sleep apnea syndrome based on localization of upper airway collapse during sleep: a preliminary study. Tohoku J Exp Med. 1998. 185:1–8.

6. Shepard JW Jr, Gefter WB, Guilleminault C, Hoffman EA, Hoffstein V, Hudgel DW, Suratt PM, White DP. Evaluation of the upper airway in patients with obstructive sleep apnea. Sleep. 1991. 14:361–371.

7. Martin SE, Marshall I, Douglas NJ. The effect of posture on airway calibre in patients with the sleep apnoea/ hypopnoea syndrome. Am J Respir Crit Care Med. 1995. 152:721–724.
8. Stanford W, Galvin J, Rooholamini M. Effects of awake tidal breathing, swallowing, nasal breathing, oral breathing and the Muller and Valsalva maneuvers on the dimensions of the upper airway: evaluation by ultrafast computerized tomography. Chest. 1988. 94:149–154.
9. Brown IG, Zamel N, Hoffstein V. Pharyngeal cross-sectional area in normal men and women. J Appl Physiol. 1986. 61:890–895.

10. Sleep-related breathing disorders in adults: recommendations for syndrome definition and measurement techniques in clinical research. The Report of an American Academy of Sleep Medicine Task Force. Sleep. 1999. 22:667–689.
11. Rubinstein I, McClean PA, Boucher R, Zamel N, Fredberg JJ, Hoffstein V. Effect of mouth piece, noseclips and head position on airway area measured by acoustic reflections. J Appl Physiol. 1987. 63:1469–1474.
12. Jan MA, Marshall l, Douglas NJ. Effect of posture on upper airway dimensions in normal human. Am J Respir Crit Care Med. 1994. 149:145–148.

13. Kushida CA, Efron B, Guilleminault C. A predictive morphometric model for the obstructive sleep apnea syndrome. Ann Intern Med. 1997. 127:581–587.

14. Jackson AC, Butler JP, Millet EJ, Hoppin FG Jr, Dawson SV. Airway geometry by analysis of acoustic pulse response measurements. J Appl Physiol. 1977. 43:523–536.

15. Fredberg JJ, Wohl MEB, Glass GM, Dorkin HL. Airway area by acoustic reflections measured at the mouth. J Appl Physiol. 1980. 48:749–758.

16. D'Urzo AD, Rubinstein I, Lawson VG, Vassal KP, Rebuck AS, Slutsky AS, Hoffstein V. Comparison of glottic areas measured by acoustic reflections vs computerized tomography. J Appl Physiol. 1988. 64:367–370.
17. Marshall I, Maran NJ, Martin S, Jan MA, Rimmington JE, Best JJ, Drummond GB, Douglas NJ. Acoustic reflectometry for airway measurements in man: implementation and validation. Physiol Meas. 1993. 14:157–169.

18. Malhotra A, Pillar G, Fogel R, Beauregard J, Edwards J, White DP. Upper-airway collapsibility: measurements and sleep effects. Chest. 2001. 120:156–161.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download