Abstract
Cardiovascular manifestations in hyperthyroidism occur frequently with various phenotypes. An association between hyperthyroidism and pulmonary arterial hypertension has been reported. In previously reported cases, the hemodynamic and symptomatic recovery of pulmonary arterial hypertension is usually concomitant with achievement of euthyroidism. We report a patient who had pulmonary arterial hypertension associated with Graves' disease, which persisted after euthyroidism was obtained.
Cardiovascular manifestations in hyperthyroidism occur frequently with various phenotypes. These include sinus tachycardia, atrial fibrillation, dilated cardiomyopathy, and high-output congestive heart failure.1) Recent studies have suggested a possible association between hyperthyroidism and pulmonary arterial hypertension.2-4) Although the exact mechanism of this combination has not yet been established, it has been hypothesized that thyroid hormones and autoimmunity have an important influence.5)
In the literature, the hemodynamic and symptomatic recovery of pulmonary arterial hypertension is usually concomitant with achievement of euthyroidism.5-8) We report a case of a patient who had persistent pulmonary arterial hypertension associated with Graves' disease. Although clinical and biochemical euthyroidism was attained within 1 month after the start of treatment, there was no improvement in right ventricular failure and echocardiographic pulmonary arterial hypertension.
A 48-year-old woman presented at our institution on June 10, 2009 with a 4-week history of dyspnea on exertion, fatigue, hot flushes, palpitations, generalized edema, and weight gain. She had a history of hyperthyroidism (3 years ago), but had not pursued follow-up. She denied any prior history of effort-induced dyspnea or chest discomfort before the diagnosis of thyroid disease was made. On physical examination, raised jugular venous pressure, a slightly enlarged thyroid gland, and marked lower limb edema were observed. There was no audible heart murmur. Chest radiography showed mild cardiomegaly with prominent pulmonary conus (Fig. 1). Electrocardiogram showed sinus rhythm at 100 beats per minute. She underwent transthoracic echocardiogram, which revealed a dilated right ventricle, reduced right ventricular systolic function, and an elevated systolic pulmonary arterial pressure over 57 mmHg. The left ventricular chamber size was normal with an ejection fraction of 65%, and the valves appeared normal. Transesophageal echocardiogram revealed no intracardiac shunts. Computed tomographic scanning of the chest did not reveal any evidence of parenchymal lung disease or pulmonary thromboembolism. A ventilation-perfusion scan of the chest showed that pulmonary embolism was unlikely. Pulmonary function test (FEV1/FVC=87.2%) revealed no evidence of chronic obstructive lung disease. Thyroid function tests showed a decreased serum thyroid-stimulating hormone (TSH) level of 0.06 uIU/mL (normal, 0-4 uIU/mL), an increased serum free thyroxin (FT4) level of 2.91 ng/dL (normal, 0.8-2.2 ng/dL). Anti-thyroperoxidase antibody was 404.97 IU/mL (nonreactive, 0-50 IU/mL) and TSH-receptor antibody was >404 U/I (normal, 0-14 U/l). Thyroid scan showed diffuse increased uptake suggestive of Graves' disease. A set of anti-nuclear antibody test which includes 13 antibodies against various component of nucleus was negative. We started treating the patient with methimazole (30 mg/day) and furosemide.
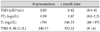
The patient was followed up clinically and went through repeated thyroid function tests and transthoracic Doppler echocardiography to determine pulmonary arterial pressure. Titration of methimazole dose continued, as well as monitoring by thyroid function tests and regular echocardiography. About 1 month after initiation of treatment, the patient became both clinically and biochemically euthyroid (Table 1), but echocardiography revealed no reduction in pulmonary artery pressure. Four months after therapy was initiated, we performed transthoracic echocardiography again but the pulmonary arterial pressure remained over 57 mmHg (Fig. 2).
The effects of thyroid hormones on myocardium and vascular system are well known, but the mechanisms underlying pulmonary arterial hypertension associated with hyperthyroidism have not been clearly identified. Possible mechanisms include direct effects of thyroid hormone and immune-mediated endothelial damage and/or dysfunction.5) The present patient had severe pulmonary arterial hypertension with clinical signs of right ventricular failure. The normal left ventricular function on echocardiography suggested that the pulmonary hypertension was not due to left-sided or high-output cardiac failure, and chronic pulmonary thromboembolism was excluded by chest CT and perfusion lung scan. The pulmonary function test showed no evidence of chronic obstructive lung disease. On physical examination, there was no severe goiter or proptosis, but thyroid function tests were compatible with Graves' disease. The possibility of autoimmune disease, which can also present with thyroid abnormalities and pulmonary hypertension, was considered negligible due to the negative result of the anti-nuclear antibody screening test. Thus, hyperthyroidism was thought to be the most likely etiology.
The successful treatment of Graves' disease leading to improvement in pulmonary arterial pressures has been previously reported with hemodynamic and symptomatic recovery usually obtained concomitantly with achievement of euthyroidism.5-8) A long time gap between achieving euthyroidism and normalization of systolic pulmonary arterial pressure has rarely been reported.9) The present patient was followed up clinically and with repeated transthoracic echocardiography and thyroid function tests. The clinical and biochemical euthyroidism was achieved within 1 month of initial therapy, but there was no improvement in right ventricular failure and echocardiographic pulmonary arterial hypertension after four months. It is conceivable that the recovery time to normalization of pulmonary artery pressure in this patient is just longer than those of most previous reports. Alternatively, this patient may represent refractory pulmonary arterial hypertension with partial irreversible structural change due to long-standing hyperthyroid state.
A significant percentage of patients with pulmonary arterial hypertension have concomitant thyroid dysfunction, either hyperthyroidism or hypothyroidism.2-4) Treatment of pulmonary arterial hypertension associated with hyperthyroidism primarily depends on the control of the thyrotoxic state. Thyroid function abnormalities should be considered in the investigation of every patient with unexplained systolic pulmonary arterial hypertension, even with normal physical examination findings. Delayed recognition and treatment of hyperthyroidism might lead to refractory pulmonary arterial hypertension as in the present case.
Figures and Tables
References
1. Klein I. Thyroid hormone and cardiovascular system. Am J Med. 1990. 88:631–637.
2. Marvisi M, Brianti M, Marani G, Del Borello R, Bortesi ML, Guariglia A. Hyperthyroidism and pulmonary hypertension. Respir Med. 2002. 96:215–220.
3. Armigliato M, Paolini R, Aggio S, et al. Hyperthyroidism as a cause of pulmonary arterial hypertension: a prospective study. Angiology. 2006. 57:600–606.
4. Chu JW, Kao PN, Faul JL, Doyle RL. High prevalence of autoimmune thyroid disease in pulmonary arterial hypertension. Chest. 2002. 122:1668–1673.
5. Nakchbandi IA, Wirth JA, Inzucchi SE. Pulmonary hypertension caused by Graves' thyrotoxicosis: normal pulmonary hemodynamics restored by (131)I treatment. Chest. 1999. 116:1483–1485.
6. Virani SS, Mendoza CE, Ferreira AC, de Marchena E. Graves' disease and pulmonary hypertension: report of 2 cases. Tex Heart Inst J. 2003. 30:314–315.
7. Marvisi M, Zambrelli P, Brianti M, Civardi G, Lampugnani R, Delsignore R. Pulmonary hypertension is frequent in hyperthyroidism and normalizes after therapy. Eur J Intern Med. 2006. 17:267–271.
8. Kang BD, Cho DK, Byun KH, Eun YM, Cho YH. Isolated pulmonary arterial hypertension: Janus' faces of hyperthyroidism. Korean Circ J. 2009. 39:168–170.
9. Hegazi MO, El Sayed A, El Ghoussein H. Pulmonary hypertension responding to hyperthyroidism treatment. Respirology. 2008. 13:923–925.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download