Abstract
Purpose
To determine if MR myelography (MRM) improves the interpretation of the severity of stenosis in patients with a multi-level lumbar stenosis.
Materials and Methods
Among the patients referred for MRI with MRM prospectively, 100 patients over 50 years old with multiple lumbar stenosis were enrolled in this study. The most severe stenotic level and the degree of stenosis at that level according to the extent of the remaining subarachnoidal space (1: normal to 50%, 2: over 50% but not a total block, 3: total block) were evaluated in a blinded manner by two observers. Conventional MRI (class A), MRM (class B) and MRI+MRM (class C) was evaluated independently and the interobserver and intraobserver reliability were assessed.
Results
In the selection of the most severe level and degree of stenosis, both observers showed a higher level of consensus with classes B and C than classes A and C. The interobserver κ average values for the selection of the most severe level in classes A, B and C were 0.649, 0.782 and 0.832, respectively. In terms of the degree of stenosis, the average in classes A, B and C were 0.727, 0.771 and 0.784, respectively. The intraobserver κ values for the above two items were the highest in class (B), followed by (C) and (A) in all observers and within the range of "almost perfect" (0.81≤κ≤1) except for the selection of the level of one observer in clause A.
Figures and Tables
Fig. 1
Definition of the severity grading scales of stenosis (1 to 3). From class (A) which refers to conventional MRI including the sagittal and horizontal T1 and T2 weighted images, the level of the line a shows no subarachnoidal space, i.e. total block (grade 3). The level of line b shows subarachnoidal space < 50% of the normal subarachnoidal space, not a total block (grade 2). The levels of lines c and d show subarachnoidal space > 50% and a compression figure (grade 1), The same severity grading scales were used: class (B), which considered only MRM, and class (A+B), which considered MRI+MRM.

Fig. 2
Effectiveness in evaluating the severity of stenosis in MR myelography. The observers were inconsistent in judging the severity of stenosis in class (A). However, they agreed that the severity of the L3/4 was more severe than the L4/5 in class (B).

Fig. 3
MRM demonstrated the most severe stenotic level. The L3/4, shows a longer total block area (bidirectional arrow) than the L2/3 level with a dilated intradural vein (arrow).
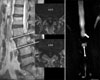
Fig. 4
The severity of the L1/2 level was evaluated as grade 3 in MRM. However, two observers selected the most severe stenotic level (grade 2) at the L4/5 level in conventional MRI. The degree of compression at the L1-2 level can be overestimated in MRM.
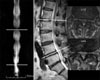
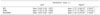
Table 1
Agreements between Each Clause

*The selection of the most severe stenotic level from T12-L1 to L5-S1, †Estimating the degree of stenosis as the extent of subarachnoidal space remaining from 1 to 3 at the selected level, ‡Cases of consensus of the most severe stenotic level. The figures in ( ) mean κ values which obtained two times.
References
1. Amundsen T, Weber H, Lilleas F, Nordal HJ, Abdelnoor M, Magnaes B. Lumbar spinal stenosis. Clinical and radiological features. Spine. 1995. 20:1178–1186.
2. Drew R, Bhandari M, Kulkarni AV, Louw D, Reddy K, Dunlop B. Reliability in grading the severity of lumbar spinal stenosis. J Spinal Disord. 2000. 13:253–258.

3. Eberhardt KE, Hollenbach HP, Tomandl B, Huk WJ. Three-dimensional MR myelography of the lumbar spine: comparative case study to X-ray myelography. Eur Radiol. 1997. 7:737–742.

4. Hashimoto K, Akahori O, Kitano K, Nakajima K, Higashihara T, Kumasaka Y. Magnetic resonance imaging of lumbar disc herniation. Comparison with myelography. Spine. 1990. 15:1166–1169.
5. Hennig J, Friedburg H, Strobel B. Rapid nontomographic approach to MR myelography without contrast agents. J Comput Assist Tomogr. 1986. 10:375–378.
6. Krudy AG. MR myelography using heavily T2-weighted fast spin-echo pulse sequences with fat presaturation. AJR Am J Roentgenol. 1992. 159:1315–1320.

7. Kuroki H, Tajima N, Hirakawa S, Kubo S, Tabe R, Kakitsubata Y. Comparative study of MR myelography and conventional myelography in the diagnosis of lumbar spinal diseases. J Spinal Disord. 1998. 11:487–492.

8. Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977. 33:159–174.

9. Pui MH, Husen YA. Value of magnetic resonance myelography in the diagnosis of disc herniation and spinal stenosis. Australas Radiol. 2000. 44:281–284.

10. Ross JS. MR imaging of the postoperative lumbar spine. Magn Reson Imaging Clin N Am. 1999. 7:513–524.

11. Schonstrom N, Hansson T. Pressure changes following constriction of the cauda equine. An experimental study in situ. Spine. 1988. 13:385–388.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download