Abstract
Purpose
The aims of this study were to evaluate the efficacy of laparoscopic totally extraperitoneal (TEP) repair of femoral hernia.
Methods
Eight patients who underwent laparoscopic TEP repair for femoral hernia between 2008 and 2010 were reviewed retrospectively. In total, 256 adult patients underwent inguinal or femoral hernia repair; TEP was performed in 224 patients. The preoperative diagnosis, clinical symptom, operative finding, postoperative complications, chronic pain, and recurrence were analyzed.
Results
The incidence of femoral hernia was 8 (3.1%) in the present study. The female to male ratio was 3:1 (6 females and 2 males). Seven patients were preoperatively misdiagnosed with inguinal hernia using ultrasonography. Computed tomography (CT) was performed in three patients, and femoral hernia was diagnosed in two patients. Two patients had synchronous femoral hernia with direct or indirect inguinal hernia. One patient has previously undergone ipsilateral inguinal hernia repair. In all patients, the hernia sac was irreducible by gas insufflation. Seven patients had lipoma-like soft tissue in hernia sac. Peritoneal tears developed in three patients. There was one postoperative complication: chronic discomfort due to seroma. There was no recurrence during median 6.5 months (range 2~26).
Figures and Tables
Fig. 1
(A) The schematic drawing of relevant anatomy of right femoral hernia.(1) (B) Laparoscpic view of right groin area.

Fig. 2
The ultrasonographic finding of right femoral hernia. The Doppler image shows the femoral hernial sac nearby the femoral vessel.

Fig. 3
The CT finding of left femoral hernia. There are typical findings of femoral hernia: venous compression and localized hernial sac in femoral area (arrow).
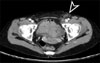
Fig. 4
Laparoscopic view of right femoral hernia. The lipoma-like mass observed in femoral area defect.

References
1. Ramshaw B. Soper NJ, editor. Surgical anatomy of the inguinal region and abdominal wall: clinical application of the total extraperitoneal approach for laparoscopic inguinal hernia repair. Problems in General Surgery. Abdominal Hernias. 2002. Vol. 19. Philadelphia: Lippincott Williams & Wilkins;14–26.
2. Amid PK, Shulman AG, Lichtenstein IL. The femoral canal: the key to femoral herniorrhaphy. Int Surg. 1990. 75:69–72.
3. McVay CB, Savage LE. Etiology of femoral hernia. Ann Surg. 1961. 154:25–32.
4. Rahaman QM, Goswami B, Gumta MK, Samanta S, Mukhopadhyay S, Chattopadhyay M. Bilateral femoral hernia in male--a case report. J Indian Med Assoc. 2005. 103:237. 242.
5. Lichtenstein IL. Herniorrhaphy. A personal experience with 6,321 cases. Am J Surg. 1987. 153:553–559.
6. Bátorfi J. The treatment of inguinofemoral hernias with laparoscopic herniorraphy. Our experience of 1210 transabdominal preperitoneal (TAPP) reconstructions. Magy Seb. 2005. 58:385–397.
7. Yalamarthi S, Kumar S, Stapleton E, Nixon SJ. Laparoscopic totally extraperitoneal mesh repair for femoral hernia. J Laparoendosc Adv Surg Tech A. 2004. 14:358–361.
8. Fitzgibbons RJ Jr, Camps J, Cornet DA, Nguyen NX, Litke BS, Annibali R, et al. Laparoscopic inguinal herniorrhaphy. Results of a multicenter trial. Ann Surg. 1995. 221:3–13.
9. Napier T, Olson JT, Windmiller J, Treat J. A long-term follow-up of a single rural surgeon's experience with laparoscopic inguinal hernia repair. WMJ. 2008. 107:136–139.
10. Sandblom G, Haapaniemi S, Nilsson E. Femoral hernias: a register analysis of 588 repairs. Hernia. 1999. 3:131–134.
11. Naude GP, Ocon S, Bongard F. Femoral hernia: the dire consequences of a missed diagnosis. Am J Emerg Med. 1997. 15:680–682.
12. Mjåland O, Bakken IJ, Skjeldestad FE, Johnson E. Inguinal and femoral hernia repair in Norway 1990-2003. Tidsskr Nor Laegeforen. 2005. 125:1338–1340.
13. Yoo H, Lee K, Choi U. The diagnostic concordance of femoral hernia and the factors influencing diagnosis. J Korean Surg Soc. 2009. 76:179–186.
14. Mikkelsen T, Bay-Nielsen M, Kehlet H. Risk of femoral hernia after inguinal herniorrhaphy. Br J Surg. 2002. 89:486–488.
15. Bendavid R. Femoral hernias: primary versus recurrence. Int Surg. 1989. 74:99–100.
16. Rhind JR. Lateral femoral hernia. J R Coll Surg Edinb. 1971. 16:299–300.
17. Chan G, Chan CK. Longterm results of a prospective study of 225 femoral hernia repairs: indications for tissue and mesh repair. J Am Coll Surg. 2008. 207:360–367.
18. Malangoni MA, Rosen MJ. Townsend CM, Beauchamp RD, Evers BM, Mattox KL, editors. Hernias. Sabiston Textbook of Surgery: The Biological Basis of Modern Surgical Practice. 2008. 18th ed. Philadelphia: W.B. Saunders;1155–1179.
19. Zhang GQ, Sugiyama M, Hagi H, Urata T, Shimamori N, Atomi Y. Groin hernias in adults: value of color Doppler sonography in their classification. J Clin Ultrasound. 2001. 29:429–434.
20. Suzuki S, Furui S, Okinaga K, Sakamoto T, Murata J, Furukawa A, et al. Differentiation of femoral versus inguinal hernia: CT findings. AJR Am J Roentgenol. 2007. 189:W78–W83.
21. Lovisetto F, Zonta S, Rota E, Mazzilli M, Bardone M, Bottero L, et al. Use of human fibrin glue (Tissucol) versus staples for mesh fixation in laparoscopic transabdominal preperitoneal hernioplasty: a prospective, randomized study. Ann Surg. 2007. 245:222–231.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download