Abstract
The bladder is involved in 1% to 3% of all hernia cases. We report a case of a large paraperitoneal bladder hernia (BH) in a 59-year-old man who had a palpable scrotal mass. Several techniques and approaches have been described for managing BHs. We performed a laparoscopic partial cystectomy and herniorrhaphy. This is the first case report on the repair of a large BH by use of a laparoscopic technique in Korea.
Herniation of the bladder is not rare and occurs in 1% to 3% of all inguinal hernias [1]. Such massive herniation accounts for only 1% of bladder hernias (BHs). In Korea, a case of inguinoscrotal BH was reported by Kim and Sul [2].
Patients with BH typically complain of a scrotal or inguinal palpable mass. Most BHs are asymptomatic and are found incidentally during herniorrhaphy or imaging studies performed for other purposes. Patients with BH may have dysuria, frequency, urgency, nocturia, or hematuria. In particular, patients with a large BH may have a pattern of two-stage voiding (the patient empties the normally located bladder and then voids again after manual compression of the hernia) [1]. BH can be diagnosed by excretory urography, retrograde cystography, computed tomography (CT), or sonography. The treatment of choice is surgical repair of the hernia.
Here, we report a case of inguinoscrotal herniation of the bladder in a 59-year-old man who was treated with laparoscopic intraperitoneal repair.
A 59-year-old man presented with a 1-year history of right scrotal swelling and irritative lower urinary tract symptoms (LUTS). He could occasionally void completely by manually compressing the inguinoscrotal mass area. He had no relevant medical history, including no abdominal surgeries. On physical examination, a 6-cm, nontender, reducible inguinal mass was noted that extended into the right scrotum (Fig. 1). No flank or abdominal masses were detected on examination. A digital rectal examination revealed a 20 g soft prostate. The patient's serum creatinine level was 1.0 mg/dL. The results of a urinalysis and urine culture were negative. The patient's International Prostate Symptom Score (IPSS) was 15.
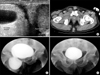
The findings of a scrotal ultrasound examination were consistent with a right inguinal anechoic lesion extending into the right hemiscrotum (Fig. 2A). A CT scan revealed that the right side of the bladder wall had herniated through the right inguinal canal (Fig. 2B). Retrograde cystography showed massive herniation of the right side of the bladder, both anteriorly and inferiorly (Fig. 2C).
To repair the hernia by laparoscopic surgery, the patient was placed in a supine position with slight Trendelenberg positioning. A CO2 pneumoperitoneum was established with a Veress needle. An 11 mm trocar, which was used as the camera port, was placed in the subumbilicus and in the right/left lower abdominal quadrant at the level of the midclavicle line. A 30°, 10-mm laparoscope was inserted into the peritoneal cavity. Laparoscopic repair of the BH was performed by a transperitoneal approach. A herniated bladder with part of the peritoneum in the right internal inguinal canal was found (Fig. 3A). The herniated bladder and the right inguinal canal area were dissected from the peritoneum, and the herniated bladder was repositioned. The BH resection margin was distinguished from normal bladder tissue by frozen section. The 2 cm right internal canal opening was closed by suturing with 4-0 Vicryl (Fig. 3B, C). The proximal margin of the herniated bladder portion, which was repositioned, was resected (Fig. 3D), and we established a right ureterovesicular opening to the bladder by stretching the tissue. The defective portion of the bladder was closed in two layers by using 3-0 and 2-0 Vicryl. The specimen was removed from the 11-mm camera port without an additional incision. No saline leaked from the sutured portion of the bladder when the bladder was filled with saline through a Foley catheter. The bladder portion was resected, and the operative time was 150 minutes. The estimated blood loss was about 100 mL. The postoperative times to initiate ambulation and diet were 0.8 and 1 day, respectively.
BH was confirmed by the pathological findings, including hypertrophy of the muscle layer. Seven days after the surgery, follow-up cystography showed a mild irregular contour on the repaired portion of the bladder (Fig. 2D). The patient's bladder capacity was approximately 450 mL. The postoperative period was uneventful, the patient's symptoms disappeared, the patient's LUTS improved, and his IPSS was 10.
Approximately 1% to 3% of all inguinal hernias involve the bladder, with a higher incidence (10%) in patients aged more than 50 years who have a large bladder [3]. Approximately 70% of BHs occur in an inguinal location, most often in men and on the right side [1]. In some cases, the bladder can herniate into the obturator, suprapubic, ischiorectal, or abdominal walls or into other pelvic or abdominal openings.
BHs are classified into three main types depending on the relationship between the herniated bladder and the peritoneum [3]. The paraperitoneal type is the most common type of herniation. In this type, a portion of the parietal peritoneum herniates laterally and protrudes into the bladder. The second most common type is the intraperitoneal type, in which the herniated portion of the bladder is completely surrounded by the peritoneal lining. The extraperitoneal type of BH occurs when the bladder herniates without any relationship with the peritoneum.
Many factors contribute to the development of a BH, including the presence of a urinary outlet obstruction causing chronic bladder distention, loss of bladder tone with weakness of the supporting structures, pericystitis and perivesical bladder fat protrusion, and obesity.
Involvement of the bladder in inguinal hernias is often not recognized before surgery to repair the hernia. Less than 7% of BHs are diagnosed preoperatively; approximately 16% of BHs are diagnosed postoperatively owing to complications, and the remainder are diagnosed perioperatively. These risks include hematuria, sepsis, urinary leakage, and fistula formation. Other complications of BHs include strangulation, infarction, and perforation. Squamous cell carcinoma, transitional cell carcinoma, and caculi have been reported to occur within a herniated bladder [4-6]. Therefore, accurate diagnosis and treatment of a BH are important to avoid these potential complications. BHs can be distinguished from a bladder diverticulum on pathological findings but not on gross findings.
The standard treatment for a BH is surgical repair. Historically, a herniated bladder was resected only if the hernia was massive. Currently, bladder resection is recommended for cases with bladder wall necrosis, a true herniated bladder diverticulum, a tight hernia neck, or a tumor in the herniated bladder [7]. Conservative therapy may occasionally be selected, which may include watchful waiting or intermittent urethral catheterization to reduce the size of the herniated bladder. Several recent case reports have shown that repair of a BH by use of laparoscopic and robotic techniques is feasible [8,9]. Velasquez-Lopez et al. [8] reported that they laparoscopically repaired a BH through the obturator foramen by placing a mesh plug. This may be a safe, fast, and effective management option. Additionally, Sung et al. [9] reported a case of a scrotal BH in a 68-year-old man who was diagnosed with prostate cancer; those authors repaired the herniated portion of the bladder by using a robot after successfully performing a robotic prostatectomy. In our patient, we chose to repair the hernia laparoscopically without the use of mesh, and we found that this technique was safe and effective.
Patients with BHs who are aged 50 years and older are often diagnosed with an enlarged prostate. Whether the LUTS are caused by the herniated bladder, the prostate enlargement, or both must be carefully determined. Inguinal hernia repair is not recommended until after benign prostatic hyperplasia has been treated. Although our patient was 59 years old, he did not have an enlarged prostate, and his LUTS disappeared after repair of the BH.
Herniation of the bladder is not rare (incidence, 1% to 3%), but it may be confused with other types of inguinal hernia. Therefore, accurate diagnosis and successful management are important to prevent bladder complications. Thus far, surgical repair has been the treatment of choice, and laparoscopic or robotic-assisted surgical techniques are now highly feasible.
Figures and Tables
References
1. Curry N. Pollack HM, McClennan BL, Dyer RB, Kenney PJ, editors. Hernias of the urinary tract. Clinical urography. 2000. 2nd ed. Philadelphia: Saunders;2987–2989.
2. Kim SW, Sul CK. Evaluation of renal injury in patients with renal stone after ESWL. Korean J Urol. 1996. 37:325–330.
3. Iason AH. Repair of urinary bladder herniation. Am J Surg. 1944. 63:69–77.
4. Epner SL, Rozenblit A, Gentile R. Direct inguinal hernia containing bladder carcinoma: CT demonstration. AJR Am J Roentgenol. 1993. 161:97–98.
5. Papadimitriou SH, Chlepas MA, Kokinacos CP, Papadopoulos CB. Massive scrotal cystocele with bladder cancer. Br J Urol. 1991. 67:330–331.
6. Postma MP, Smith R. Scrotal cystocele with bladder calculi (case report). AJR Am J Roentgenol. 1986. 147:287–288.
7. Vindlacheruvu RR, Zayyan K, Burgess NA, Wharton SB, Dunn DC. Extensive bladder infarction in a strangulated inguinal hernia. Br J Urol. 1996. 77:926–927.
8. Velasquez-Lopez JG, Gil FG, Jaramillo FE. Laparoscopic repair of obturator bladder hernia: a case report and review of the literature. J Endourol. 2008. 22:361–364.
9. Sung ER, Park SY, Ham WS, Jeong W, Lee WJ, Rha KH. Robotic repair of scrotal bladder hernia during robotic prostatectomy. J Robot Surg. 2008. 2:209–211.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download