Abstract
Purpose
The purpose of this study was to identify the occurrences and the factors contributing to constipation in the post surgical period following major orthopedic surgery.
Methods
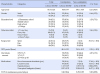
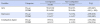
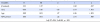
The sample included 133 patients who had surgery of the hip, knee, or spine. Patients were excluded from the study if there was a history of bowel surgery or constipation from chart review. Data were collected using questionnaires such as Korean version of Modified Barthel index (K-MBI), Hospital Anxiety and Depression Scale, and Constipation Assessment Scale (CAS) before surgery and on the third postoperative day.
Results
Reports of constipation occurred in 77 instances (57.9%). The first reported defecation was within 4.0±2.2 days following surgery. Mean days of first defecation of constipation group vs. non-constipation group was 5.5±1.7 days vs. 2.1±1.0 days. There were statistically significant differences between patients who reported than those who did not in terms of age, length of NPO period, postoperative ADL, and the reported incidents of preoperative and postoperative depressive symptoms. Postoperative ADL, age, and NPO period were significant influencing factors of constipation and explained 52.4% of the variance.
Figures and Tables
Table 1
Incidence of Constipation and Postoperative First Defecation in Patients underwent Orthopedic Surgery (N=133)

References
1. De Souza MS. Effectiveness of nursing interventions in alleviating perceived problems among orthopaedic patients. J Orthop Nurs. 2002; 6:211–219.
2. Şendir M, Bűyűkyilmaz F, Aşti T, Gűrpinar Ş, Yazgan İ. Postoperative constipation risk assessment in Turkish orthopedic patients. Gastroenterol Nurs. 2012; 35(2):106–113. DOI: 10.1097/SGA.0b013e31824d2945.

3. Hsieh C. Treatment of constipation in older adults. Am Fam Physician. 2005; 72:2277–2284.
4. Martin NS, Nicolas RS, Gerhard H, Karl S, Enrico T, Oliver PG. Constipation after thoraco-lumbar fusion surgery. Clin Neurol Neurosurg. 2014; 126:137–142. DOI: 10.1016/j.clineuro.2014.08.036.
5. Davies EC, Green CF, Mottram DR, Pirmohamed M. The use of opioids and laxatives, and incidence of constipation, in patients requiring neck-of-femur (NOF)surgery: a pilot study. J Clin Pharm Ther. 2008; 33:561–566. DOI: 10.1111/j.1365-2710.2008.00949.x.
6. De Lillo AR, Rose S. Functional bowel disorders in the geriatric patient: constipation, fecal impaction, and fecal incontinence. Am J Gastroenterol. 2000; 95(4):901–905. DOI: 10.1111/j.1572-0241.2000.01926.x.

7. Koloski NA, Jones M, Wai R, Gill RS, Byles J, Talley NJ. Impact of persistent constipation on health-related quality of life and mortality in older community-dwelling women. Am J Gastroenterol. 2013; 108:1152–1158. DOI: 10.1038/ajg.2013.137.

8. Pare P, Ferrazzi S, Thompson WG, Irvine EJ, Rance L. An epidemiological survey of constipation in Canada: definitions, rates, demographics, and predictors of health care seeking. Am J Gastroenterol. 2001; 96(11):3130–3137. DOI: 10.1111/j.1572-0241.2001.05259.x.

9. Nassar AP Jr, da Silva FM, de Cleva R. Constipation in intensive care unit: Incidence and risk factors. J Crit Care. 2009; 24(4):630.e9–630.e12. DOI: 10.1016/j.jcrc.2009.03.007.

10. Drossman DA, Sandler RS, McKee DC, Lovitz AJ. Bowel patterns among subjects not seeking health care. Use of a questionnaire to identify a population with bowel dysfunction. Gastroenterology. 1982; 83(3):529–534.
11. Kyle G. The older person: management of constipation. Br J Community Nurs. 2010; 15(2):58–64. DOI: 10.12968/bjcn.2010.15.2.46391.

12. Bouras EP, Tangalos EG. Chronic constipation in the elderly. Gastroenterol Clin North Am. 2009; 38(3):463–480. DOI: 10.1016/j.gtc.2009.06.001.

13. Shim HW. Constipation and activities of daily living of the institutionalized elderly. J Korean Acad Soc Nurs Educ. 2004; 10(2):252–261.
14. Kinnunen O. Study of constipation in a geriatric hospital, day hospital, old peoples home and at home. Aging (Milano). 1991; 3(2):161–170.
15. Cook SF, Lanza L, Zhou X, Sweeney CT, Goss D, Hollis K, et al. Gastrointestinal side effects in chronic opioid users: results from a population-based survey. Aliment Pharmacol Ther. 2008; 27(12):1224–1232. DOI: 10.1111/j.1365-2036.2008.03689.x.

16. Tuteja AK, Biskupiak J, Stoddard GJ, Lipman AG. Opioid induced bowel disorders and narcotic bowel syndrome in patients with chronic non-cancer pain. Neurogastroenterol Motil. 2010; 22(4):424–430. DOI: 10.1111/j.1365-2982.2009.01458.x.
17. Kim JH, Park JS. The effects of abdominal meridian massage on the degree of constipation among the patients with immobility after orthopedic surgery. Clin Nurs Res. 2006; 12(2):63–72.
18. Lee YA, Choi HJ, Jo YM, Lee IS. Effects of abdominal massage or lactic acid fermented milk for constipation in patients following spinal surgery. J Korean Clin Nurs Res. 2013; 19(2):208–217.
19. Jung HY, Park BK, Shin HS, Kang YK, Pyun SB, Paik NJ, et al. Development of the Korean version of modified Barthel index: Multi-center study for subjects with stroke. J Korean Acad Rehabil Med. 2007; 31(3):283–297.
20. Oh SM, Min KJ, Park DB. A study on the standardization of the Hospital Anxiety and Depression Scale for Koreans. J Korean Neuropsychiatr Assoc. 1999; 38(2):289–296.
21. Yang S. Effects of fluid intake, dietary fiber supplement and abdominal muscle exercise on antipsychotic drug-induced constipation in schizophrenics. J Cathol Med Coll. 1992; 45(4):1501–1514.
22. The Korean Geriatrics Society. Geriatric Medicine. 2nd ed. Seoul: Medical Pulishing;2005. p. 304.
23. Rasmussen LS, Pedersen , PU . Constipation and defecation pattern the first 30 days after thoracic surgery. Scand J Caring Sci. 2010; 24(2):244–250. DOI: 10.1111/j.1471-6712.2009.00713.x.
24. Loren M, Cathy M, Barbara AP. Comparison of two bowel treatments to prevent constipation in post-surgical orthopedic patients. Int J Orthop Trauma Nurs. 2010; 14(2):75–81. DOI: 10.1016/j.joon.2009.07.049.
25. Orji EO, Olabode TO, Kuti O, Ogunniyi SO. A randomised controlled trial of early initiation of oral feeding after cesarean section. J Matern Fetal Neonatal Med. 2009; 22(1):65–71. DOI: 10.1080/14767050802430826.

26. Lee KN, Sung KW. The factors affecting the constipation of the elderly at nursing home. J Korean Acad Community Health Nurs. 2008; 19(4):575–586.
27. Park AJ, Lim NY, Kim YS, Song JH. Prevalence and risk of constipation among the institutionalized elderly. J East West Nurs Res. 2011; 17(1):57–65.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download